Essential Guide to AHIMA Verification for Healthcare Professionals
If you’ve ever felt like verifying healthcare credentials is as confusing as deciphering a doctor’s handwriting—welcome to the club. AHIMA verification is the golden key to ensuring that healthcare professionals are qualified, certified, and ready to handle patient data like a pro.
But in 2025, credential verification is more than just a formality—it’s a safeguard against fraud, a compliance requirement, and a career booster. Whether you're an employer, a healthcare organization, or a professional looking to validate your qualifications, understanding AHIMA verification is non-negotiable.
So, grab your coffee (or your fourth cup if it’s been that kind of day) because we’re about to dive deep into the world of AHIMA credentialing. By the end of this guide, you’ll be an AHIMA verification expert, ready to verify, validate, and vouch for the best professionals in the industry!

What is AHIMA Verification and Why Does It Matter?
The Power of Credential Verification
This is vital in the fast paced healthcare practice where making a wrong choice of who to hire as a worker, or more so a patient’s data handler can be disastrous. AHIMA (American Health Information Management Association) ensures the legitimacy of healthcare professionals by providing a verification system that helps employers and organizations verify the credentials of a candidate instantly.
Why Employers Trust AHIMA for Credential Checks
Prevents Fraud – Ensures that medical coders, billing specialists, and health information managers hold valid certifications.
Compliance Assurance – Many healthcare regulations (HIPAA, CMS, etc.) require credential validation to meet industry standards.
Quality Control – Organizations need skilled professionals who can handle medical records with accuracy and compliance.

How Does AHIMA Verification Work?
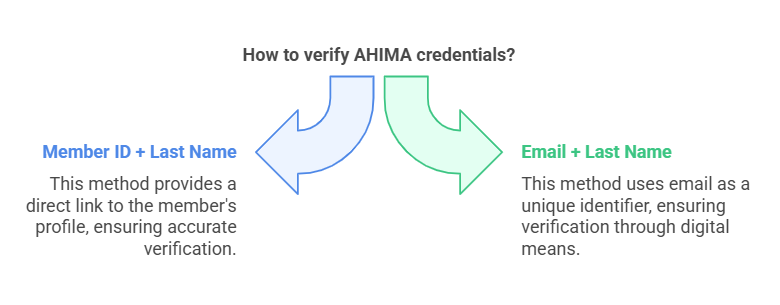
AHIMA allows employers and organizations to verify credentials in multiple ways:
Using a Member ID + Last Name
Using an Email + Last Name
This system ensures only authorized professionals have access to patient data, reducing the risk of errors, breaches, and malpractice.
How to Prepare for AHIMA Certification Exams in 2025
Which AHIMA Certifications are Available?
Before you verify credentials, it’s essential to understand the different types of AHIMA certifications.

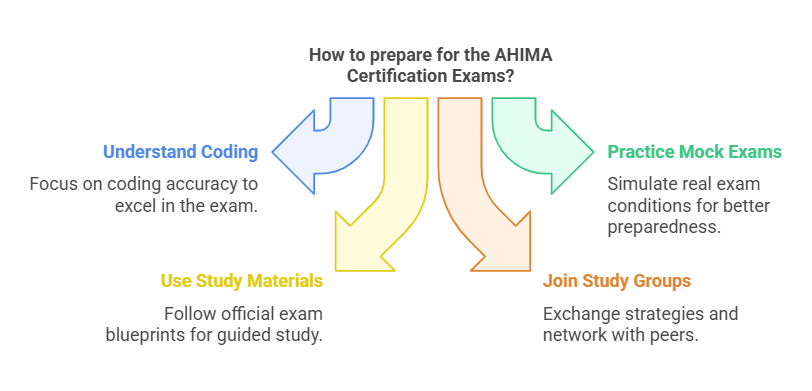
Tips to Pass the AHIMA Certification Exams
Understand ICD-10-CM and ICD-10-PCS Codes – 70% of your exam will focus on coding accuracy.
Practice with Full-Length Mock Exams – AHIMA offers official practice tests that mimic real exam conditions.
Use AHIMA-Approved Study Materials – While AHIMA doesn’t endorse specific resources, their official exam blueprints are a great guide.
Join Study Groups – Network with other candidates on AHIMA forums to exchange study strategies.
Maintaining and Advancing Your AHIMA Credentials
Why Continuing Education is a Must in 2025
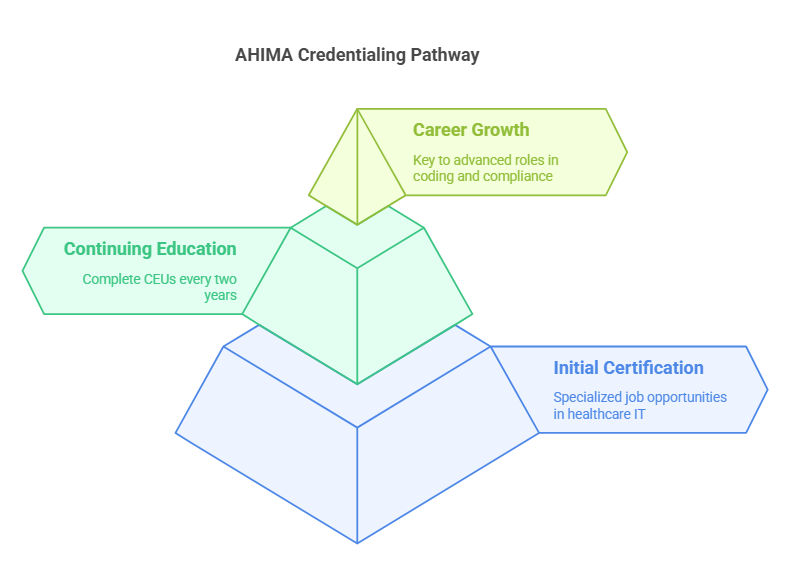
AHIMA certification isn’t a one time process it is a continuous one. To maintain your AHIMA credentials, you need to complete continuing education units (CEUs) every two years.
Career Growth with AHIMA Certifications
Getting an AHIMA certification is the key to specialized job opportunities in healthcare IT, medical coding, compliance, and privacy protection.
How to Verify AHIMA Credentials (Step-by-Step Guide)
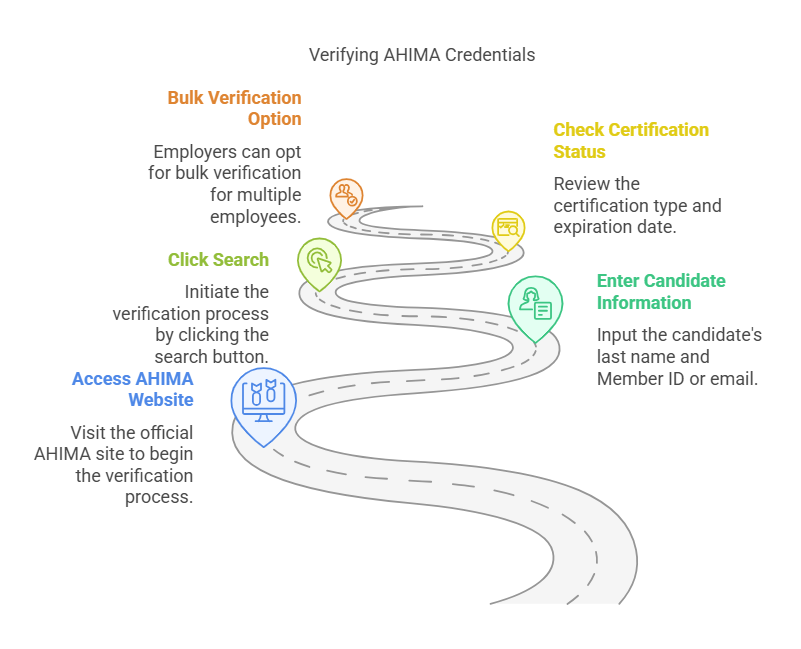
Go to AHIMA’s official website.
Enter the candidate’s last name and Member ID or email.
Click "Search" to verify their certification status.
Check the certification type and expiration date.
Employers can also request bulk verification services for multiple employees at once.
AHIMA vs. AAPC: Which Credential Matters More?
Both AHIMA and AAPC are industry leaders in medical coding and health information management certifications. However, they serve slightly different purposes:

For a broader career path in health information management, AHIMA certifications offer more flexibility and career growth potential.
10 Less Commonly Known Facts About AHIMA Verification
AHIMA has been verifying credentials for over 95 years.
CEUs can be earned through free webinars on the AHIMA website.
Employers can set up automated alerts for credential expirations.
AHIMA offers student discounts on certification exams.
Some states require AHIMA certification for Medicaid billing roles.
AHIMA’s CCHIIM oversees certification integrity and updates exam content regularly.
AHIMA-certified professionals earn 20-30% more than non-certified counterparts.
Credential verification can be done via mobile devices on AHIMA’s site.
Global recognition—AHIMA certifications are valid in multiple countries.
AHIMA is actively working on AI-driven coding assistance tools.
People Also Ask: 8 Common Questions
-
Typically, less than a minute if you have the Member ID or Email.
-
Yes! You must renew them every two years with CEUs.
-
Yes! AHIMA offers bulk verification services.
-
Depends on your career path—AHIMA is better for health information management, AAPC for medical coding.
-
You’ll have to pay a reinstatement fee and complete extra CEUs.
-
Yes, credential verification is free for employers and organizations.
-
Yes! AHIMA certifications are valid worldwide.
-
Online or at authorized Pearson VUE test centers.
Final Thoughts: The Best Medical Coding and Billing Certificates
If you're looking for the best medical coding and billing certificates, be sure to check out AMBCI. They offer top-tier certifications that help professionals advance their careers, increase earning potential, and stay competitive in the ever-evolving healthcare industry.
Need to verify an AHIMA credential? Now you know how to do it like a pro!
