Essential Reads on Medical Billing and Coding for Professionals
Medical billing and coding are essential processes in healthcare that ensure proper insurance reimbursement for the services rendered. These tasks involve translating medical services into standardized codes, and their accuracy is crucial for the financial health of healthcare providers. This article provides an overview of the key responsibilities, types of codes used, challenges in the field, and the impact of technology on these processes. Whether you're new to the field or updating your knowledge, this article offers valuable insights.
Understanding Medical Billing and Coding
Medical billing and coding involve translating healthcare services into universally recognized codes for insurance reimbursement. This includes converting patient diagnoses and prescribed treatments into alphanumeric codes. These codes are essential for insurance claims processing and ensure that healthcare providers are properly compensated for their services. Individuals in this field must have a strong understanding of medical terminology and coding systems to ensure accuracy and efficiency. Earning a Medical Billing and Coding Certification from a reputable institution like AMBCI (American Medical Billing and Coding Institute) provides individuals with the necessary skills and knowledge to excel in this vital healthcare role, opening doors to numerous career opportunities in the growing field.
Accurate medical documentation is also critical. If a procedure or treatment isn't documented in the medical records, it won't be reimbursed. Thus, medical billers and coders must work closely with healthcare providers to ensure that records are complete and precise. The process also requires compliance with regulations like HIPAA, which governs the security of health information.
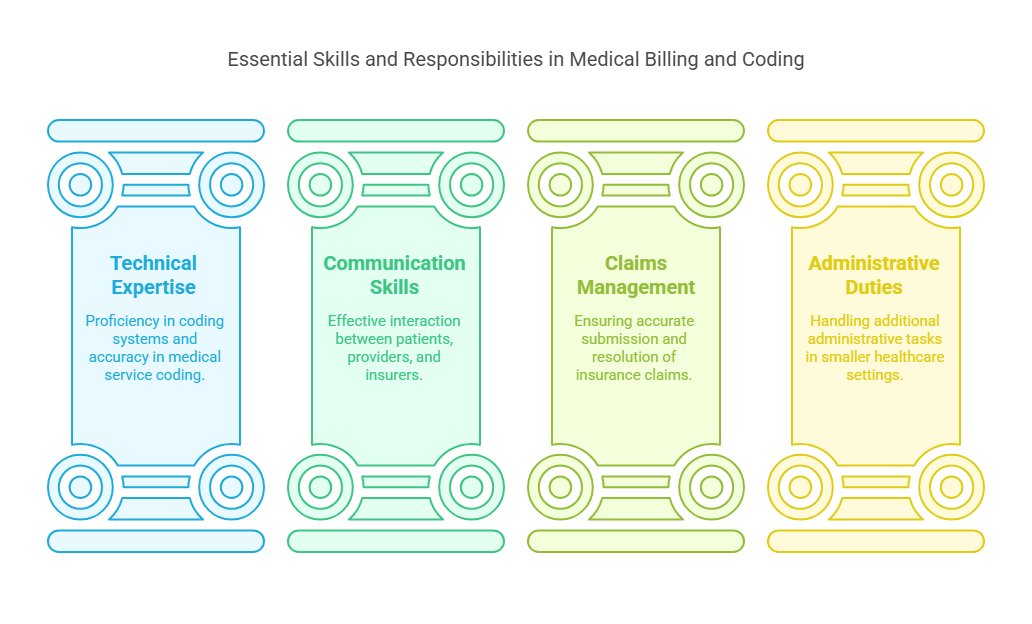
Key Responsibilities of Medical Billers and Coders
Medical billers and coders play a vital role in the financial sustainability of healthcare organizations. They ensure that medical services are correctly coded and that insurance claims are submitted accurately. These professionals must gather all necessary data, check the accuracy of the entered codes, and resolve any rejected claims. Their work directly influences the revenue cycle of healthcare providers.
In addition to technical expertise with coding systems, medical billers and coders must possess strong communication skills. They act as intermediaries between patients, healthcare providers, and insurers, ensuring that the claims process is smooth and that payments are received on time. In smaller healthcare settings, these professionals may also handle other administrative duties, making precision even more important.
Types of Medical Codes: A Comprehensive Guide
Medical coding is categorized into diagnosis and procedure codes. Diagnosis codes are used to describe the medical condition being treated, with the most common set being the International Classification of Diseases (ICD) codes. These include both ICD-10-CM for clinical modifications and ICD-10-PCS for procedures. Procedure codes, on the other hand, are used to describe the treatments or services provided to the patient. These are primarily categorized under Current Procedural Terminology (CPT) codes, which are divided into three categories:
Category I: Used for procedures and services.
Category II: Used for performance measures.
Category III: Used for emerging technologies and procedures.
Additionally, the Healthcare Common Procedure Coding System (HCPCS) includes codes for non-physician services and durable medical equipment.
The Importance of Accurate Medical Documentation
Accurate medical documentation is the foundation of effective medical billing and coding. Inaccurate documentation can lead to coding errors, which can result in claim denials or delays in reimbursement. Healthcare providers must ensure that their documentation is complete and precise, following the guidelines established by organizations like the Centers for Medicare & Medicaid Services (CMS).
Medical billing specialists review each claim line-by-line to identify and correct errors before submission. This process is crucial for securing the rightful reimbursement and ensuring the financial stability of healthcare organizations.
Challenges in Medical Billing and Coding
Professionals in medical billing and coding face several challenges, including keeping up with frequent changes in regulations and procedures. Errors like incorrect code entry, often due to typographical mistakes, can lead to rejected claims. Compliance with regulations such as HIPAA adds an additional layer of complexity. To stay compliant, medical billers and coders must undergo continuous education and training.
Technological advancements in reimbursement systems, such as bundled payments and accountable care organizations (ACOs), also require professionals to stay updated with new methods and policies. Many healthcare organizations now outsource billing and coding to specialized third-party services to ensure that they remain compliant and up-to-date with the latest standards.
The Role of Technology in Medical Billing and Coding
Technology is transforming the medical billing and coding industry. Tools like Robotic Process Automation (RPA) and Artificial Intelligence (AI) are making the process more efficient and accurate. AI and Natural Language Processing (NLP) can automatically review clinical notes and assign appropriate codes, reducing human error and increasing the speed of claims processing.
Medical billing software plays a significant role in this transformation by automating claim submission, scrubbing claims for errors, and managing patient eligibility verification. These advancements allow healthcare providers to process claims more quickly, reducing the likelihood of denials and speeding up reimbursements.
Training and Certification for Medical Billers and Coders
To succeed in medical billing and coding, professionals must undergo specialized training and certification. Training programs typically include diploma or associate degree courses, with certification being crucial for career advancement. Certifications like the Certified Coding Associate (CCA) and Certified Professional Coder (CPC) validate a professional’s skills and knowledge in coding practices.
Continuing education is required to maintain certifications, and medical billers and coders must stay updated on industry trends, coding guidelines, and regulations. With the growing demand for skilled medical billers and coders, professionals in this field have ample opportunities for career growth.
Career Development in Medical Billing and Coding
A career in medical billing and coding can be both rewarding and challenging. With increasing healthcare demand, there is a growing need for skilled professionals in this field. Certification can lead to better job opportunities and higher salaries. As they gain experience, medical billers and coders can advance to positions like coding auditors, compliance officers, and practice managers.
The future of this career looks bright, with many healthcare organizations offering competitive salaries and benefits to attract qualified professionals. With the proper education and certifications, individuals can excel in this dynamic field and contribute to the success of healthcare institutions.
Best Practices for Medical Billing and Coding
To improve efficiency and accuracy, medical billers and coders should follow best practices such as implementing automated claim scrubbing tools and tailoring claims to meet individual payer requirements. Outsourcing billing services to specialized companies can also help healthcare providers stay compliant with regulations and reduce administrative burdens.
Future Trends in Medical Billing and Coding
The future of medical billing and coding is shaped by advancements in technology. The use of AI, machine learning, and blockchain technology is expected to further enhance the accuracy and security of billing operations. These technologies will automate processes, reduce errors, and improve reimbursement rates. Healthcare providers must adapt to these changes to stay competitive in the evolving landscape.
Benefits of Outsourcing Medical Billing and Coding Services
Outsourcing medical billing and coding services can offer numerous benefits to healthcare providers, especially smaller practices. It reduces overhead costs, minimizes errors, and accelerates reimbursement processes. By outsourcing, healthcare providers can focus on delivering quality care while ensuring that billing operations run smoothly and efficiently.
Medical Billing and Coding in Different Healthcare Settings
Medical billing and coding are essential in various healthcare settings, including hospitals, clinics, and private practices. These professionals handle a wide range of tasks, from processing inpatient claims to managing outpatient billing for small practices. Their work is crucial to the financial health of healthcare providers across the board.
6 Lesser-Known Facts About Medical Billing and Coding
ICD-11 is coming: The World Health Organization (WHO) is gradually transitioning to ICD-11 codes, which offer more precise and extensive options compared to ICD-10.
CPT Codes for Telehealth: There are specific CPT codes for telehealth services, ensuring providers can receive reimbursement for virtual consultations.
Coding is not one-size-fits-all: Different insurance companies may require distinct coding practices, making coding a highly tailored process.
Medical coders must stay updated: Codes and regulations change regularly, and coders must maintain Continuing Education Units (CEUs) to keep certifications active.
AI in coding: Artificial intelligence (AI) is improving accuracy by automating the review and assignment of codes, potentially reducing errors.
Global Impact: Medical billing and coding are used internationally, although coding systems like ICD and CPT may vary by country.
Frequently Asked Questions (FAQs)
-
Description text goes here
-
Description text goes here
-
Description text goes here
-
Item description
-
Item description
As of 2025, medical billing and coding continues to evolve with the integration of advanced technologies such as AI, machine learning, and blockchain. These innovations are expected to enhance the accuracy, security, and efficiency of billing processes, ensuring healthcare providers are reimbursed promptly and accurately.