Top Billing and Coding Practice Test to Ace Your Exam
Are you preparing for the Certified Professional Coder (CPC) exam or any other medical billing and coding certification test? In 2025, the medical coding industry continues to evolve, requiring professionals to stay ahead with updated knowledge and coding guidelines. A billing and coding practice test is your ultimate tool for exam success, as it replicates real-world scenarios and enhances your understanding of medical coding systems, including ICD-10-CM, CPT®, and HCPCS Level II.

This guide will walk you through everything you need to know about medical billing and coding practice tests, how they help in certification exams, and the best strategies for excelling in the field of healthcare reimbursement.
Key Takeaways for Success in the CPC Exam and Medical Coding
The Certified Professional Coder (CPC) exam consists of 100 multiple-choice questions covering 17 knowledge areas. Candidates must score at least 70% within a four-hour time limit.
Engaging in practice medical billing and coding tests helps identify knowledge gaps, understand updated coding guidelines, and simulate real-world case studies.
Reputable organizations like AMBCI.org provide expert guidance, certified billing and coding specialist certification practice tests, and flexible payment options to support exam candidates.
Budgeting for certification is critical. Candidates should consider AAPC membership fees, exam fees, and other costs associated with study materials.
Why Medical Billing and Coding Practice Tests Matter
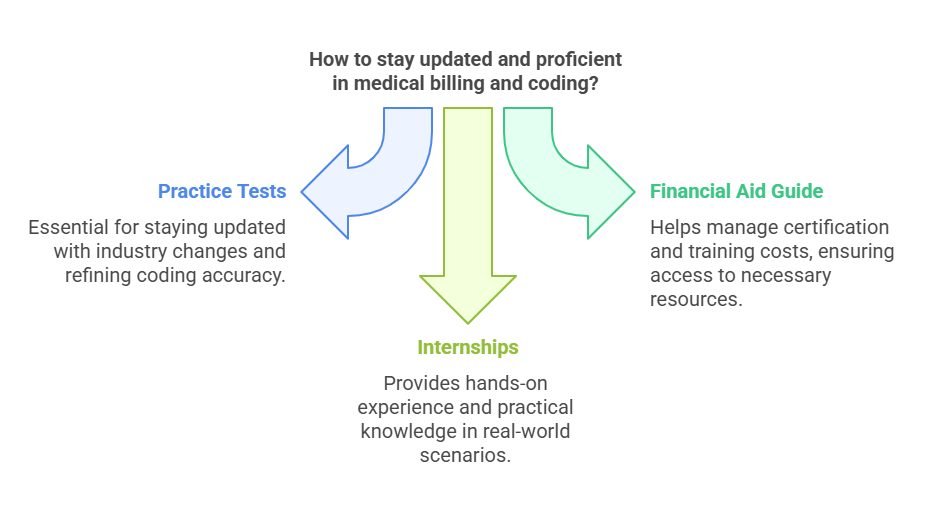
The healthcare industry is evolving rapidly, with new compliance regulations and insurance policies shaping how medical billing and coding professionals operate. A Financial Aid Guide for billing and coding can assist students and professionals in navigating the costs of certification and training programs, ensuring that they have access to the resources needed for success in the field. Practice medical billing and coding tests serve as essential tools to ensure you stay updated with these changes while refining your ability to accurately code medical procedures and diagnoses.
By 2025, AI-powered coding tools and automated claim processing are becoming standard in healthcare administration. However, human coders remain irreplaceable due to their expertise in handling complex medical cases, reimbursement disputes, and compliance audits.
Taking certified revenue cycle specialist practice tests helps you master the entire medical billing process, from patient registration to insurance claim submission, ensuring accuracy and efficiency in medical coding. Medical coding internships further provide hands-on experience, allowing you to apply your skills in real-world scenarios while gaining practical knowledge of the healthcare industry's billing and coding procedures.
Understanding the Certified Professional Coder (CPC) Exam
The CPC exam is a rigorous certification test conducted by the American Academy of Professional Coders (AAPC). This exam measures your knowledge in medical coding principles, regulatory compliance, and reimbursement methodologies.
What to Expect in the CPC Exam?
100 multiple-choice questions covering topics like medical terminology, anatomy, compliance, coding guidelines, and case-based scenarios.
Exam duration: 4 hours.
Allowed reference materials: CPT®, ICD-10-CM, and HCPCS Level II manuals.
Scoring requirement: Minimum 70% to pass.
Passing the CPC exam is crucial for professionals aiming for higher salaries and better job opportunities in the medical coding industry. In 2025, certified coders earn approximately $25,000 more annually than non-certified counterparts.
Eligibility & Registration
To take the CPC exam, candidates must:
Have at least two years of professional medical coding experience OR
Complete an AAPC-approved training program.
Additionally, candidates should prepare for the medical billing and coding certification test with extensive practice exams and study materials.
Key Areas Covered in Billing and Coding Practice Tests
Taking a certified billing and coding specialist certification practice test provides exposure to the most critical areas tested in the CPC exam.
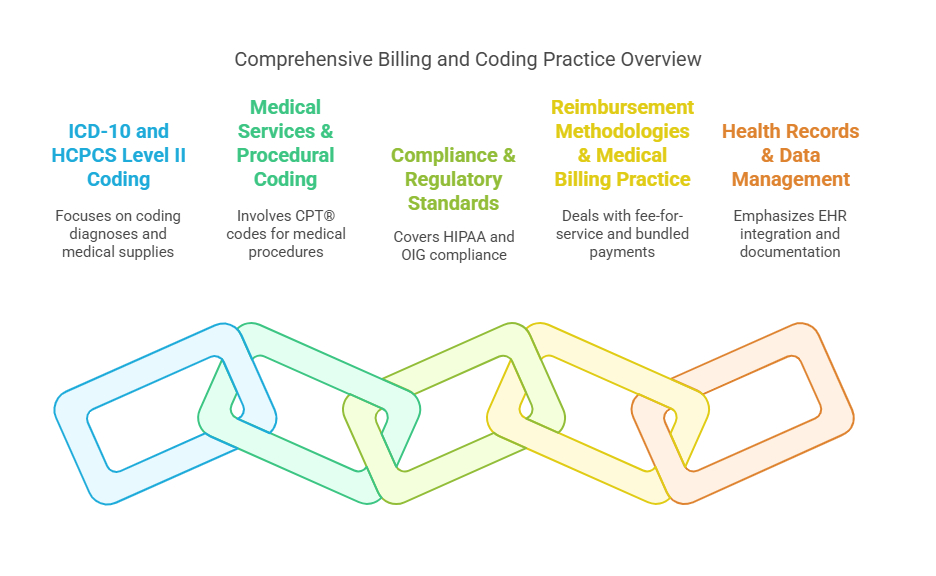
1. ICD-10 and HCPCS Level II Coding
ICD-10-CM is used to code diagnoses and inpatient procedures.
HCPCS Level II covers medical supplies, non-physician services, and transportation.
CMS updates HCPCS codes annually, requiring coders to stay informed about new changes.
2. Medical Services & Procedural Coding
CPT® codes are used for surgical, radiological, and diagnostic procedures.
Medical billing practice tests enhance skills in accurately assigning procedural codes.
Coders must understand documentation requirements to ensure proper reimbursement.
3. Compliance & Regulatory Standards
Federal laws like HIPAA and OIG compliance play a crucial role in medical billing.
Avoiding fraudulent billing is essential for ethical medical coding practices.
Certified revenue cycle specialist practice tests train coders in insurance claims processing and denial management.
4. Reimbursement Methodologies & Medical Billing Practice
Understanding fee-for-service models, bundled payments, and value-based reimbursement is key.
Errors in medical billing can lead to claim denials and financial losses for healthcare providers.
Mastering medical billing practice tests ensures coders optimize revenue cycles.
5. Health Records & Data Management
Proper documentation of diagnoses, treatments, and patient encounters is necessary.
EHR (Electronic Health Records) integration is increasingly important in 2025.
Coders must ensure accuracy in clinical documentation to avoid reimbursement delays.
Preparing for the CPC Exam: Study Resources & Tips
Success in the medical billing and coding certification test requires structured preparation. Here are some proven study strategies:
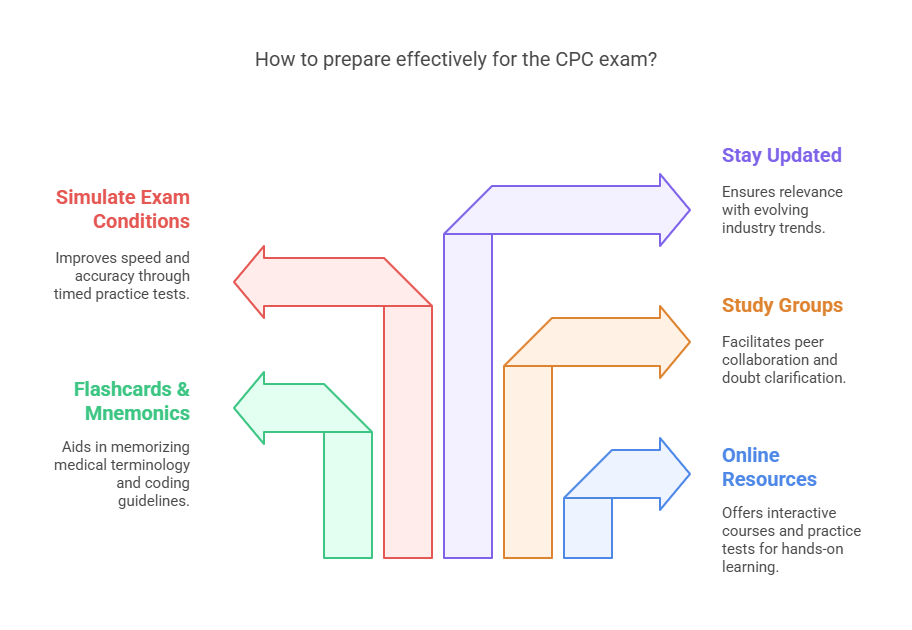
1. Use Online Resources & Courses
Platforms like AMBCI.org offer interactive courses, study guides, and video tutorials.
Engage in certified billing and coding specialist certification practice tests for hands-on learning.
2. Flashcards & Mnemonics
Memorizing medical terminology and coding guidelines becomes easier with flashcards.
Utilize mnemonics to retain complex billing regulations.
3. Join Study Groups & Forums
Collaborate with peers to discuss challenging CPC exam questions.
Online study communities help clarify doubts and improve coding accuracy.
4. Simulate Real Exam Conditions
Take timed practice medical billing and coding tests to improve speed and accuracy.
Develop test-taking strategies to efficiently navigate complex coding questions.
5. Stay Updated with Industry Trends
In 2025, telemedicine billing codes, AI-assisted coding tools, and EHR compliance are evolving rapidly.
Regularly reviewing AAPC updates ensures relevance in the job market.
Test Day Strategies: What to Expect
On the day of the exam, candidates must:
Arrive early and bring permitted coding manuals.
Manage time effectively, allocating 2-3 minutes per question.
Carefully review case-based scenarios to ensure correct coding selections.
Scoring is based on the number of correct answers, and passing the CPC exam grants official certification valid for one year. Maintaining certification requires continuing education credits.
Why Choose AMBCI.org for Your CPC Exam Preparation?
AMBCI.org offers a comprehensive study platform designed for aspiring medical coders. Their benefits include:
Expert-led practice exams mimicking real CPC test conditions.
Flexible payment plans, starting at $189 per month.
Job placement guarantee within six months of certification.
By leveraging AMBCI.org's extensive resources, you can confidently pursue your medical billing and coding certification test and secure a rewarding career in healthcare reimbursement.
FAQs:
-
The CPC exam is a certification test conducted by the AAPC to evaluate knowledge in medical coding. It is essential for coders aiming for better job opportunities and higher salaries, as certified professionals earn significantly more than non-certified coders.
-
Effective preparation involves using online resources, engaging in practice tests, joining study groups, and simulating real exam conditions to enhance speed and accuracy in coding.
-
The CPC exam covers ICD-10-CM for diagnosis coding, CPT® for procedural coding, and HCPCS Level II for medical supplies and services, along with compliance and reimbursement methodologies.
-
You must either have at least two years of professional medical coding experience or complete an AAPC-approved training program before registering for the CPC exam.
-
On test day, bring your coding manuals (ICD-10, CPT®, and HCPCS Level II), a photo ID, and any permitted materials. Managing your time efficiently during the exam is crucial for success.
5 Lesser-Known Facts:
AI and automation in medical coding:
CPC certification opening global opportunities:
Telemedicine billing codes evolution:
Continuous education requirement for CPC certification:
Medical coding can lead to higher-paying roles:
Final Thoughts on Mastering Medical Billing and Coding in 2025
To excel in the CPC exam, it is essential to:
Utilize certified revenue cycle specialist practice tests.
Stay updated with ICD-10, CPT®, and HCPCS coding changes.
Engage in practice medical billing and coding sessions regularly.
Develop a structured study plan and effective time management skills.
With the right preparation, medical coders in 2025 will continue to play a pivotal role in healthcare revenue management. Take advantage of practice tests, expert resources, and exam strategies to ensure success in your certification journey!
