Top Benefits of Being a Billing Coder Today
Billing coders play a crucial role in the healthcare industry by translating patient care into standardized codes for accurate billing and insurance claims. This career offers diverse opportunities in medical offices, hospitals, and insurance companies. With proper training and certification, professionals in this field enjoy stable job prospects, flexible work environments, and competitive salaries. Here, we explore the key benefits of being a billing coder, essential skills required, career opportunities, and industry trends in 2025.

The Role and Importance of Billing Coders
Billing coders ensure that healthcare providers receive accurate and timely reimbursements. Their job involves converting medical diagnoses, procedures, and services into standardized codes, which insurance companies use to process claims. A meticulous understanding of industry codes such as ICD-10, CPT, and HCPCS, along with medical billing and coding certification from AMBCI, is essential for accurate billing and compliance with healthcare regulations.
Beyond financial accuracy, billing coders also help maintain organized patient records. Their work ensures that medical histories are well-documented, which is crucial for future treatments and insurance verifications. With the growing complexity of insurance policies and electronic health records (EHRs), the demand for skilled billing coders continues to rise.

Why Medical Billing and Coding Matter in Healthcare
Medical billing and coding are fundamental to the financial health of healthcare institutions. Without accurate coding, providers risk claim denials and financial losses. Efficient billing practices also contribute to smoother patient experiences by reducing delays in insurance approvals and clarifying patient responsibilities for medical expenses.
A well-functioning billing system supports healthcare providers in delivering high-quality care without administrative burdens. With technological advancements, automation and AI-driven coding software are streamlining processes, yet human expertise remains essential to managing complex cases and resolving discrepancies.
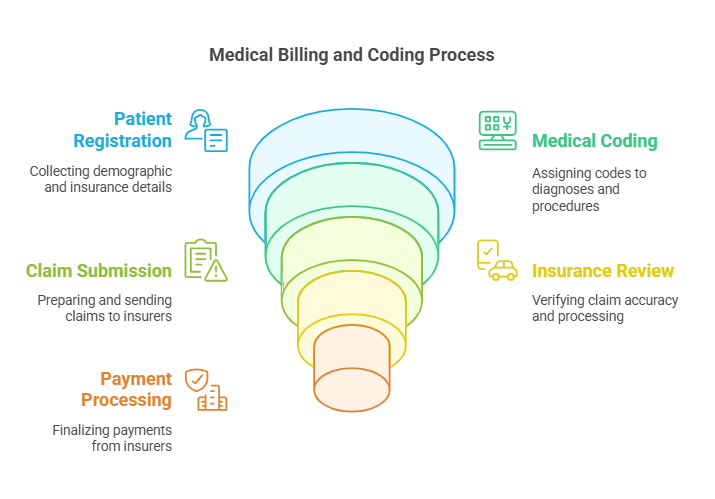
The Medical Billing and Coding Process
The billing and coding workflow consists of several key steps:
Patient Registration: Collecting demographic and insurance details to initiate the billing process.
Medical Coding: Assigning accurate codes to diagnoses, treatments, and procedures.
Claim Submission: Preparing and sending claims to insurance companies for review.
Insurance Review and Payment Processing: Verifying claim accuracy before payment approval.
Patient Billing and Follow-Up: Managing unpaid balances and addressing claim denials.
This structured approach ensures that healthcare providers receive due payments while maintaining compliance with industry regulations.
Key Differences Between Medical Billing and Coding
Although closely related, billing and coding serve different functions:
Medical Coding: Focuses on translating healthcare services into standardized codes used in documentation and insurance claims.
Medical Billing: Deals with processing payments, submitting claims, and ensuring timely reimbursements from insurance providers.
In large healthcare facilities, these roles are often handled by separate professionals, while in smaller offices, one person may perform both tasks.
Essential Skills for Billing Coders
To excel as a billing coder, professionals must possess a combination of technical knowledge and soft skills:
Medical Terminology Mastery: Understanding medical procedures, diagnoses, and treatments.
Attention to Detail: Ensuring coding accuracy to prevent claim rejections.
Analytical Skills: Reviewing patient records to resolve discrepancies.
Time Management: Handling multiple tasks within strict deadlines.
Communication Skills: Collaborating with healthcare providers and insurance representatives.
As regulations and technology evolve, continuous learning is crucial for success in this field.
Certification and Training Requirements
Certification enhances career prospects for billing coders. Many employers prefer candidates with credentials such as:
Certified Professional Coder (CPC)
Certified Coding Associate (CCA)
Certified Billing and Coding Specialist (CBCS)
Training programs, available both online and in-person, typically last between four and eight months. These courses prepare candidates for certification exams and provide essential hands-on experience.
Career Opportunities and Growth
Medical billing and coding offer diverse career paths, including:
Hospital and Clinic Billing Departments
Insurance Companies
Outpatient Care Facilities
Telemedicine and Remote Coding Jobs
Freelance Medical Billing
As demand for healthcare services increases, job opportunities in this field are expected to expand significantly. Specializing in areas such as oncology, cardiology, or emergency medicine can lead to higher salaries and career advancement.
Work Environment and Flexibility
Billing coders enjoy flexible work arrangements, including:
On-Site Employment: Hospitals, clinics, and insurance offices.
Remote Work: Many coding jobs can be done from home, offering better work-life balance.
Freelancing: Independent coders can set their own schedules and choose clients.
With technological advancements, remote and freelance opportunities have grown, allowing professionals to work from anywhere while maintaining compliance with HIPAA regulations.
Salary Expectations for Billing Coders in 2025
The earning potential for billing coders varies based on experience, location, and certifications:
Entry-Level Salary: $45,000 per year.
Mid-Level Professionals: $58,000 to $65,000 annually.
Experienced Coders with Specializations: Over $75,000 per year.
Certified professionals earn significantly more than non-certified counterparts, making certification a worthwhile investment.
Future Outlook for Billing Coders
The demand for billing coders is projected to grow by 10% by 2030, fueled by:
The increasing adoption of electronic health records (EHRs).
A growing aging population requiring frequent medical care.
The expansion of telehealth services, requiring specialized coding expertise.
With healthcare regulations becoming more complex, billing coders will remain in high demand, ensuring job security and career stability.
6 Lesser-Known Facts About Medical Billing and Coding
Coders Can Work Internationally – Medical coding standards like ICD-10 are used globally, allowing coders to work in different countries.
The International Classification of Diseases (ICD) is a globally used medical classification maintained by the World Health Organization (WHO). ICD-10, the 10th revision, is used in 117 countries for cause of death reporting and statistics.
en.wikipedia.orgIt’s Not Just a Desk Job – Some billing coders consult with healthcare providers and audit records for compliance.
Medical coding involves not only assigning codes to diagnoses and procedures but also ensuring compliance with healthcare regulations. Coders may consult with healthcare providers and audit records to maintain accuracy and compliance.
en.wikipedia.orgAI is Changing the Industry – Automation helps with routine coding, but human oversight is still necessary for accuracy.
Artificial intelligence (AI) and automation are increasingly used in medical coding to handle routine tasks. However, human oversight remains crucial to ensure accuracy and address complex coding scenarios.Billing Coders Help Prevent Fraud – By ensuring accurate coding, they reduce billing fraud and insurance fraud risks.
Accurate medical coding is essential in preventing billing and insurance fraud. Billing coders play a key role in ensuring that codes are applied correctly, thereby reducing the risk of fraudulent claims.
en.wikipedia.orgNot All Medical Coders Have a Healthcare Background – Many professionals transition from IT, finance, or administration.
Medical coding is a field accessible to professionals from various backgrounds. Many coders transition from areas such as information technology, finance, or administration, bringing diverse skills to the role.You Can Become a Coding Instructor – Experienced coders can train new professionals, opening doors to teaching careers.
Experienced medical coders have the opportunity to become instructors, training new professionals entering the field. This career path allows seasoned coders to share their knowledge and expertise.
FAQs About Billing Coders
-
To become a billing coder, you typically need a high school diploma and certification from an accredited program. Common certifications include CPC, CCA, and CBCS.
-
While the job requires precision and attention to detail, it offers flexible work options and a structured workflow that can reduce stress compared to other healthcare roles.
-
Yes, many medical coders work remotely, particularly those with certification and experience. Healthcare facilities and insurance companies often hire remote coding professionals.
-
Most training programs take between 4 to 8 months, followed by certification exams. Some programs offer accelerated courses that can be completed in a shorter timeframe.
-
Common challenges include keeping up with changing healthcare regulations, maintaining accuracy to avoid claim rejections, and handling complex insurance policies.
Final Thoughts
Medical billing and coding offer a rewarding career with excellent job prospects, competitive salaries, and flexible work options. As the healthcare industry continues to grow, skilled billing coders will play an essential role in ensuring accurate record-keeping and financial stability. Whether you're looking for a stable career, remote work opportunities, or a pathway into the healthcare industry, becoming a billing coder is a smart choice in 2025.
