Top Reasons to Pursue a CBCS Certification in Medical Billing and Coding
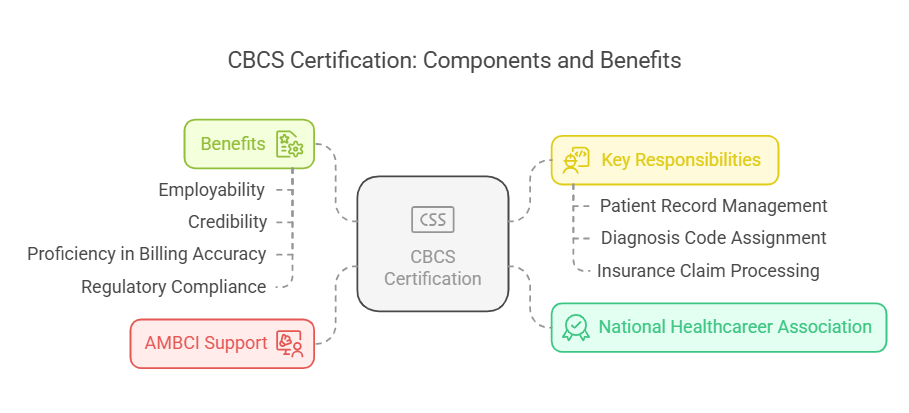
Medical billing and coding is a rapidly growing field, and obtaining a Certified Billing and Coding Specialist (CBCS) certification can significantly enhance your career prospects. Offered by the National Healthcareer Association (NHA), the CBCS certification validates your skills and opens doors to numerous job opportunities in the healthcare industry. This guide provides an updated overview of the CBCS certification, including its benefits, eligibility criteria, and career prospects in 2025.

What is CBCS Certification?
The Certified Billing and Coding Specialist (CBCS) certification is an industry-recognized credential provided by the National Healthcareer Association (NHA). It assesses the expertise required for entry-level professionals in medical billing and medical coding certification. This certification ensures that individuals can accurately manage patient records, assign diagnosis codes, and process insurance claims efficiently. AMBCI proudly supports this certification, helping professionals gain the skills and recognition they need to excel in the healthcare field.
As a medical coder, you are responsible for converting patient diagnoses and procedures into standardized codes that are essential for insurance reimbursement and financial stability in healthcare institutions. By obtaining a CBCS certification, professionals demonstrate their proficiency in billing accuracy, medical coding standards, and regulatory compliance.
With continuous growth in the healthcare sector, a CBCS certification increases your employability and credibility, proving your competence in handling crucial administrative tasks in medical billing.
Eligibility Criteria for CBCS Certification
To qualify for the CBCS exam, candidates must meet specific educational and experience requirements. As of 2025, the updated eligibility criteria include:
Minimum Age Requirement – Candidates must be at least 18 years old.
Educational Background – A high school diploma or equivalent (GED) is required.
Training or Work Experience – Candidates must have completed an accredited medical billing and coding training program within the past five years, or have at least one year of supervised work experience in medical billing and coding within the last three years.
Regulatory Compliance Knowledge – Familiarity with HIPAA regulations, medical billing procedures, and insurance coding standards is essential for the exam.
Meeting these requirements ensures that candidates are well-prepared to pass the CBCS certification test and uphold high professional standards in medical billing and coding.

Skills Assessed in the CBCS Exam
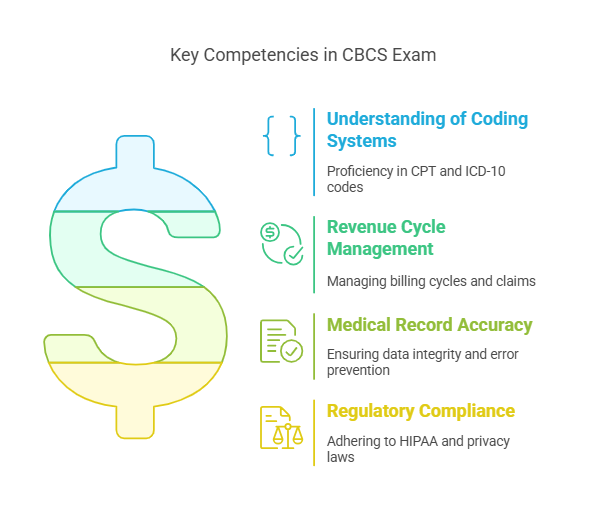
The CBCS exam evaluates candidates on various critical skills essential for success in medical billing and coding. These include:
Understanding of Coding Systems – Candidates must demonstrate proficiency in using the Current Procedural Terminology (CPT) and International Classification of Diseases (ICD-10) coding systems.
Revenue Cycle Management – This includes managing billing cycles, processing insurance claims, and ensuring compliance with payer regulations.
Medical Record Accuracy – The ability to verify insurance eligibility, maintain patient data integrity, and prevent billing errors.
Regulatory Compliance – Ensuring adherence to HIPAA laws, healthcare privacy regulations, and medical documentation standards.
These competencies ensure that CBCS-certified professionals can perform their duties efficiently, supporting both healthcare providers and patients.
Benefits of Becoming a Certified Billing and Coding Specialist
Earning a CBCS certification offers multiple career advantages, including:
Increased Job Opportunities – Certified specialists are in high demand in hospitals, private clinics, insurance firms, and telemedicine services.
Competitive Salary – Entry-level professionals earn between $40,000 and $60,000 per year, with experienced coders making over $70,000 annually.
Quick Career Entry – Many online medical billing training programs can be completed within a few weeks, allowing for rapid workforce entry.
Flexible Work Environments – CBCS professionals can work in remote, freelance, or in-office roles, providing greater work-life balance.
Career Growth and Specialization – Additional certifications or specializations (e.g., oncology or surgical coding) can lead to higher salaries and managerial roles.
Beyond financial benefits, certification ensures greater accuracy in billing practices, reduced claim denials, and enhanced patient trust in healthcare providers.

How to Prepare for the CBCS Exam
To successfully pass the CBCS exam, candidates should:
Review the NHA's Official Study Guide – The National Healthcareer Association provides a detailed test plan outlining key exam topics.
Take Online Practice Tests – Practice exams help candidates become familiar with the exam format and question types.
Attend Formal Training Programs – Enrolling in an accredited billing and coding program improves understanding of industry standards and compliance requirements.
Gain Hands-on Experience – Working in a medical office or completing an externship can enhance practical skills.
By following a structured study plan, candidates can increase their chances of passing the exam on their first attempt.
Career Opportunities for CBCS-Certified Professionals
A CBCS certification can open doors to various healthcare administrative roles, including:
Medical Billing Specialist – Processes patient payments and insurance claims.
Medical Coder – Assigns standardized codes to medical diagnoses and procedures.
Insurance Claims Analyst – Reviews medical claims for compliance and accuracy.
Medical Records Technician – Manages patient data and ensures regulatory compliance.
According to 2025 industry projections, employment for medical billing and coding professionals is expected to grow by 8% from 2022 to 2032, adding approximately 15,000 new jobs per year.
Additionally, CBCS-certified individuals can advance into higher-paying roles such as medical records auditor or healthcare practice manager.
Salary Expectations for CBCS-Certified Professionals
Salaries for CBCS-certified professionals depend on factors like experience, location, and additional certifications. The latest figures indicate:
Entry-level salary: $40,000 – $50,000 per year.
Mid-level salary: $55,000 – $65,000 per year.
Experienced professionals: $70,000+ annually.
Specialized or management roles: $80,000+ annually.
Professionals in urban areas and those with advanced coding credentials tend to earn the highest salaries.
6 Lesser-Known Facts About CBCS Certification
Some states require additional certifications beyond CBCS to work in government healthcare programs.
State healthcare compliance requirements vary, with some states imposing specific regulations and standards beyond federal requirements.
medtrainer.com
Medical coders can work remotely, making it a great career for those seeking work-from-home opportunities.
The demand for remote medical coding positions is significant, offering flexibility for professionals seeking work-from-home opportunities.
medicalbillingtips.com
CBCS is different from CPC (Certified Professional Coder)—CPC focuses more on physician coding, while CBCS includes broader billing tasks.
The Certified Professional Coder (CPC) certification focuses on outpatient coding, including CPT, ICD-10-CM, and HCPCS Level II codes, while the CBCS encompasses a broader range of billing tasks.
medicalbillingtips.com
Advanced AI tools are integrating into medical coding, making it essential for professionals to stay updated on automation trends.
The integration of advanced AI tools in medical coding is transforming the industry, highlighting the importance for professionals to stay updated on automation trends.
medicalbillingtips.com
Some employers pay for certification fees as part of their employee development programs.
Many employers support employee development by covering certification costs; a survey found that 94% of employers pay for some or all expenses related to professional certifications.
hrdive.com
CBCS-certified professionals can freelance, allowing them to work for multiple healthcare providers at once.
The flexibility of CBCS certification enables professionals to engage in freelance work, offering services to multiple healthcare providers simultaneously.
medicalbillingtips.com
Frequently Asked Questions (FAQs)
-
A high school diploma or GED is required to enroll in a CBCS training program.
-
Most training programs take between 8 weeks and 6 months, depending on the institution and study format.
-
Yes, many medical billing and coding professionals work remotely or in flexible work environments.
-
Candidates can retake the exam, but they may have to pay a retest fee and wait for a designated period before attempting again.
-
Earning additional certifications, gaining experience, and specializing in high-demand areas like surgical coding can significantly increase earnings.
Conclusion
Obtaining a CBCS certification is a valuable step toward a successful career in medical billing and coding. With increasing demand for certified specialists, this credential not only enhances employability but also offers financial growth and job flexibility. By choosing the right training program and preparing effectively, you can secure a rewarding position in the healthcare industry.
