Choosing the Right Medical Billing and Coding Job Training Program
The healthcare industry is one of the fastest-growing sectors in the United States, and as a result, medical billing and coding professionals are in high demand. If you're looking to start a rewarding career in this field, selecting the right medical billing and coding training program is essential. With numerous options available, it can be overwhelming to decide which program aligns best with your goals. This blog will guide you through the factors to consider when choosing a training program, focusing on accreditation, training options, curriculum quality, cost, and job placement support.
Why Accreditation Matters
When it comes to choosing the best medical billing and coding training program, one of the most important factors to consider is whether the program is accredited. Accreditation serves as a mark of quality assurance, ensuring that the program meets specific standards required by the healthcare industry.
What is Accreditation?
Accreditation is a process by which a recognized accrediting body evaluates the quality of an educational program. For medical billing and coding programs, the American Health Information Management Association (AHIMA) and the American Academy of Professional Coders (AAPC) are two of the primary accrediting organizations.
Why is Accreditation Important?
Industry Recognition: Accredited programs are more likely to be recognized by employers and professional organizations. Completing an accredited program ensures that you have received the training that meets industry standards.
Certification Eligibility: Many certifications require completion of an accredited program as a prerequisite. For example, to sit for the Certified Professional Coder (CPC) exam through AAPC, you must have completed an accredited training program.
Quality Education: Accreditation ensures that the curriculum is up-to-date and comprehensive. It also indicates that instructors are qualified and the program is committed to preparing students for successful careers in medical billing and coding.
How to Verify Accreditation
Before enrolling in any program, confirm that it is accredited by a recognized accrediting body. You can typically find accreditation information on the school’s website, or you can contact the accrediting organization directly.
Online vs. In-Person Programs
One of the biggest decisions when selecting a medical billing and coding training program is whether to pursue online or in-person training. Both options offer their own set of advantages and challenges, and the right choice depends on your personal preferences, schedule, and learning style.
Online Medical Billing Training
Online medical billing and coding programs are becoming increasingly popular due to their flexibility and accessibility. Here are the pros and cons:
Pros of Online Training:
Flexibility: You can complete coursework from anywhere, at your own pace, and on your own schedule. This is especially beneficial for working professionals or individuals with other commitments.
Cost-Effective: Online programs are often less expensive than traditional in-person programs. You’ll save money on commuting, and many online schools offer more affordable tuition rates.
Access to a Wide Range of Programs: Online programs offer a greater variety of options, including specialized courses and certifications. This allows you to find a program that fits your career goals perfectly.
Cons of Online Training:
Self-Motivation Required: Without the structure of in-person classes, online students must be highly motivated to stay on track and complete assignments on time.
Limited Interaction: Online programs may lack the face-to-face interaction that some students thrive on. While many programs offer online forums or virtual study groups, it can be challenging for some students to stay engaged without in-person guidance.
Hands-on Learning Limitations: Some aspects of medical billing and coding, such as practical experience with coding software, may be harder to learn remotely. However, many online programs try to offset this with interactive modules or virtual labs.
In-Person Medical Billing Training
In-person training is the traditional method of learning medical billing and coding, and it has its own unique benefits.
Pros of In-Person Training:
Structured Environment: In-person classes offer more structure and direct oversight from instructors. If you thrive in a classroom setting and prefer face-to-face interaction, this may be the right choice for you.
Immediate Feedback: If you have questions or need clarification, you can get immediate feedback from instructors and fellow students.
Networking Opportunities: Being on-campus allows you to interact with classmates, which can create valuable professional connections in the healthcare industry.
Cons of In-Person Training:
Less Flexibility: You are required to attend classes at scheduled times, which may not be convenient for individuals with other obligations, such as work or family commitments.
Higher Costs: In-person training often requires commuting, which can lead to additional costs, such as transportation or parking. Additionally, tuition for in-person programs may be higher due to overhead costs for the institution.
Limited Accessibility: Depending on your location, there may be limited options for in-person programs, especially if you live in a rural area.
What to Look For in a Training Program
When evaluating different medical billing and coding training programs, several factors should guide your decision-making process. Below are the key elements to consider:
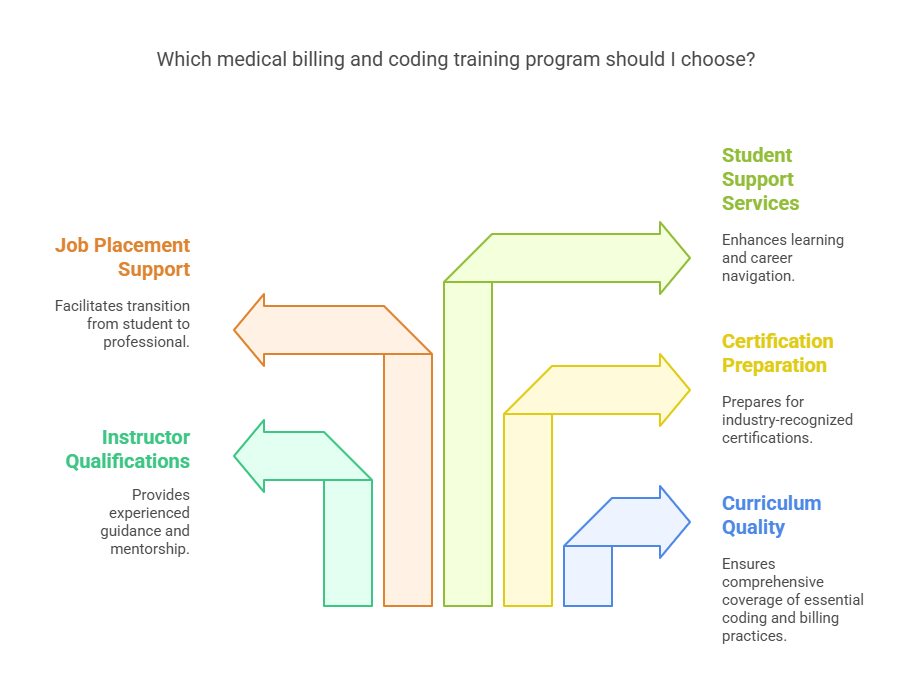
1. Curriculum Quality
The curriculum should cover all essential aspects of medical billing and coding, including:
ICD-10 Coding: Learning the International Classification of Diseases (ICD-10) system is fundamental for accurate coding.
CPT and HCPCS Codes: These codes are crucial for billing medical procedures.
Medical Terminology: Understanding medical language is essential for accurately interpreting physician notes and coding appropriately.
Insurance and Billing Practices: Knowledge of insurance policies, coding for reimbursements, and medical claims processes is vital.
2. Instructor Qualifications
Ensure that the instructors are certified professionals with real-world experience in the field. Experienced instructors will be able to offer valuable insights into the industry and provide mentorship as you advance in your career.
3. Certification Preparation
Certification is a critical step toward becoming a qualified medical billing and coding professional. A good training program should provide preparation for industry-recognized certifications, such as the Certified Professional Coder (CPC) and Certified Coding Specialist (CCS).
4. Job Placement Support
Some programs offer job placement assistance, which can be a significant advantage. Look for programs that have strong relationships with healthcare employers and offer internship or job placement programs that can help you transition from student to professional.
5. Student Support Services
Access to student support services, such as tutoring, academic advising, and technical support, can make a big difference in your success. Some schools also offer career counseling to help you navigate the job market after graduation.
Cost of Medical Billing and Coding Training Programs
The cost of medical billing and coding programs can vary widely depending on whether you choose an online or in-person program, the length of the course, and the level of certification provided.
Typical Costs
Online Programs: These programs typically range from $1,000 to $5,000. The price depends on the program's length, accreditation, and the credentials it provides.
In-Person Programs: Traditional in-person programs can cost between $2,500 and $7,500. Again, this varies based on the institution and program specifics.
Financial Aid Options
If you're considering a career in medical billing and coding, the Top Medical Billing and Coding Online Class with Financial Aid can be an excellent option for you. Many schools offer financial aid opportunities, including federal student loans, grants, and scholarships. If you're attending an accredited institution, you may be eligible for federal financial aid, which can help ease the financial burden. Be sure to thoroughly explore all available financial aid options to make an informed decision about your educational investment.
Return on Investment
While the upfront cost of training may seem high, it’s important to consider the long-term financial benefits. The average salary for a medical billing and coding professional is approximately $45,000 per year, with the potential to earn more with experience and certification. With the growing demand for these professionals, a medical billing and coding certification can offer a significant return on investment.
Frequently Asked Questions (FAQs)
-
While certification isn’t always required, it is highly recommended as it increases job prospects and potential salary.
-
The length of the program can vary. Online programs may take as little as 6 months, while in-person programs can take up to a year.
-
Yes! The healthcare industry is growing rapidly, and medical billing and coding professionals are in high demand.
-
Many medical billing and coding professionals work from home, especially after gaining some experience.
-
The most common certifications are the CPC (Certified Professional Coder) and CCS (Certified Coding Specialist), both of which are recognized by employers across the industry.
5 Less-Known Facts About Medical Billing and Coding
1. Medical Billing and Coding Can Be Done Remotely
Medical billing and coding professionals have the flexibility to work remotely. For instance, Indeed lists thousands of remote medical billing and coding job opportunities, offering roles such as Medical Biller, Coding Specialist, and Medical Coding Instructor with flexible schedules and benefits .Job Search | Indeed
2. Specialized Coding Exists
The field of medical coding encompasses various specialties. For example, The Coding Network provides coding services across numerous specialties, including orthopedics, dermatology, and pediatric surgery . Additionally, Penn Foster offers specialty certifications like Certified Professional Coder in Dermatology (CPCD) and Pediatrics (CPEDC), focusing on specific procedures and services within these field. The Coding NetworkPenn Foster
3. Continuous Learning Is Key
Staying updated with the latest coding practices is essential. The American Medical Association (AMA) regularly releases updates to the CPT® code set, with the 2025 edition introducing 270 new codes, 112 deletions, and 38 revisions . Furthermore, the Centers for Medicare & Medicaid Services (CMS) announced 50 new ICD-10-PCS codes effective April 1, 2025, emphasizing the importance of continuous education in the field .American Medical Association+2American Medical Association+2Allzone+2CMS
4. You Can Work in Various Settings
Medical coders are employed in diverse environments. According to Indeed, common workplaces include hospitals, physician's offices, outpatient surgery centers, clinics, insurance agencies, and government agencies . Similarly, CareCloud outlines that medical billing and coding professionals can work in settings such as physician offices, hospitals, clinics, nursing homes, home health agencies, insurance companies, government agencies, billing companies, consulting firms, and educational institutions .devry.edu+1Health Tech Academy+1Job Search | Indeed+1devry.edu+1CareCloud
5. High Job Satisfaction
Many professionals in medical billing and coding report high job satisfaction. Campus.edu highlights that the field offers a flexible schedule, opportunities for continuous learning, and a dynamic work environment, contributing to overall job satisfaction . Additionally, Northwest Career College notes that the career path provides stability, earning potential, and opportunities for advancement .Elite education for all.Northwest Career College
Conclusion
Choosing the right medical billing and coding job training program is crucial to your career success. Accreditation, curriculum quality, and whether the program prepares you for certification and job placement should be key factors in your decision. Online and in-person options each have their own set of benefits, so it’s important to assess your personal situation to determine which is best suited for you.
At AMBCI, we offer accredited medical billing and coding certification programs that will help you launch your career in this high-demand field. We’re committed to providing the best training and support to ensure you’re prepared to succeed in your professional journey. Reach out to us today and start your path toward certification!