Difference Between Medical Biller and Medical Coder: Key Insights
Recognizing the distinction between a medical coder and a medical biller is critical for those pursuing a profession in healthcare administration. Medical coders are tasked with converting medical procedures into universal codes, which plays an instrumental role in streamlining billing processes and facilitating insurance claims. Conversely, medical billers manage fiscal transactions to secure that healthcare providers receive payment for their services rendered. This exposition delves into these positions, delineating their respective duties and the competencies requisite for both roles, thereby elucidating the difference between a medical coder and a certified professional biller, highlighting the importance of certification and professional qualifications in the field.
Key Takeaways
Medical billers and coders have distinct roles; billers handle medical claim submissions and patient invoicing, while coders translate medical procedures into standardized codes.
Both medical billing and coding require strong attention to detail, organizational skills, and effective communication to ensure accurate billing and reimbursement processes.
Educational requirements typically include a high school diploma or an associate degree, with certifications enhancing career prospects and potential earnings in the healthcare field.
Understanding Medical Billing and Coding
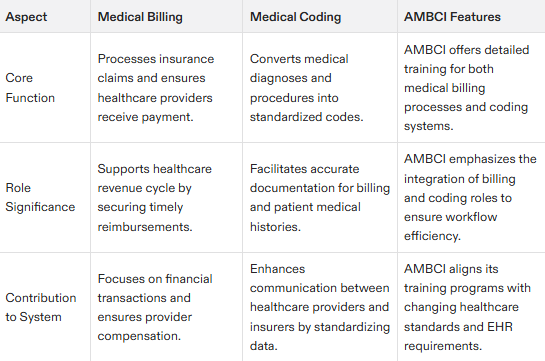
Medical billing and coding serve distinct yet interconnected functions in the healthcare system. The process of medical coding converts various diagnoses, treatments, and procedures into universal codes. Conversely, medical billing is focused on submitting insurance claims and ensuring follow-ups are conducted to guarantee that healthcare providers receive appropriate compensation.
Each practice plays a vital role in keeping precise documentation and controlling expenses as part of the revenue cycle within the health sector. Medical coders translate services provided into codes while those engaged in medical billing utilize these specific codes to invoice patients or insurers for payment.
Collectively, they constitute an essential infrastructure supporting a healthcare organization’s financial stability by facilitating accurate charging practices and streamlining reimbursement processes within the intricate architecture of our modern healthcare system.
What is Medical Billing?
Medical billing procedures involve submitting and following up on claims to insurance companies to ensure payment for healthcare services. This process begins with gathering insurance information and verifying patient eligibility before services are provided.
Medical billers create a medical claim using information from medical coders, send these claims to insurance providers, and follow up on unpaid claims. They also invoice patients for any remaining balances after insurance payouts.
Accurate billing by medical billers aids the healthcare revenue cycle and supports the financial health of healthcare organizations.
What is Medical Coding?
Medical coding involves converting diagnoses, treatments, and procedures into standardized codes, translating medical practices and medical terminology into a universal language for billing and record-keeping. Assigning specific codes ensures accurate documentation and communication of patient care.
Codes like ICD-10 and CPT are crucial for billing, processing insurance claims, and tracking patient history. Accurate coding optimizes revenue for healthcare providers and ensures payment for services rendered.
Medical coders convert raw patient data into valuable information that supports the healthcare system.
Key Responsibilities
Medical billers and coders have distinct but complementary roles within the healthcare revenue cycle. Billers act as intermediaries between patients, providers, and insurers, ensuring timely and accurate claim submission. Coders convert medical procedures and diagnoses into standardized codes for billing and record-keeping.
These roles are vital for accurate billing and reimbursement in healthcare. Technological advancements like automation and AI have enhanced the efficiency of billing and coding, reducing errors and expediting reimbursements.
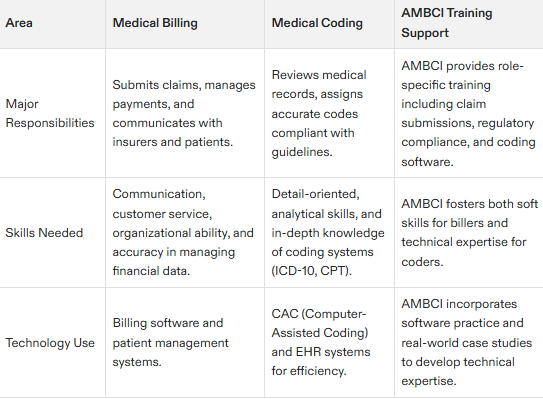
Responsibilities of a Medical Biller
Medical billers are responsible for confirming if a patient is eligible for insurance, collecting the necessary insurance details, and accurately filling out claims to enhance reimbursement. They manage appeals related to claims, devise payment plans for patients, and aid in processing payments via phone.
Medical billers monitor incoming payments and pursue any outstanding claims while addressing issues that come up. They oversee the preparation of bills directed at both patients and their insurers by making sure all essential patient data is compiled to facilitate clear communication about billing matters.
Responsibilities of a Medical Coder
Medical coders scrutinize medical records, assigning specific codes to diagnoses and procedures strictly following established coding guidelines and regulations. Their compliance is crucial for ensuring precise billing and proper reimbursement.
The conversion of raw data into valuable information that can be utilized by healthcare providers is accomplished through the assignment of standardized codes by these medical coders. Such accurate coding facilitates the billing process as well as guarantees comprehensive documentation and effective communication regarding patients’ medical histories.
Required Skills and Personality Traits
It’s essential that individuals engaged in medical billing and coding possess meticulous attention to detail along with robust organizational abilities. They are required to precisely decode medical records, ensuring adherence to stringent billing regulations and coding standards. Proficiency in communication is imperative for the seamless exchange of information among patients, healthcare providers, and insurance companies.
Those pursuing a career in medical billing should harbor a keen interest in the field of healthcare coupled with an earnest aspiration to assist patients through their work. Success within this domain can be achieved by those who exhibit both extroverted and introverted characteristics. These traits’ effectiveness varies according to specific job roles and workplace settings.
Skills Needed for Medical Billers
Medical billers must possess excellent communication and customer service abilities to engage successfully with both patients and insurance providers. A personable, outgoing manner is advantageous when interacting regularly with patients.
It’s essential for medical billers to have robust organizational capabilities and a solid grasp of coding protocols to streamline the billing cycle effectively. Ensuring accurate billing is imperative as they address conflicts with insurance firms and discuss payment arrangements.
Skills Needed for Medical Coders
To ensure precise billing and insurance claims, medical coders must be meticulous and well-organized in assigning codes to procedures and diagnoses. The correctness of these codes is essential as it directly affects the processing of insurance claims.
Individuals who have an analytical mindset, take pleasure in working with data sets, and favor technical work may find a career in medical coding particularly fitting. This field often appeals to introverts who excel when working independently on tasks that require focus.
Education and Certification
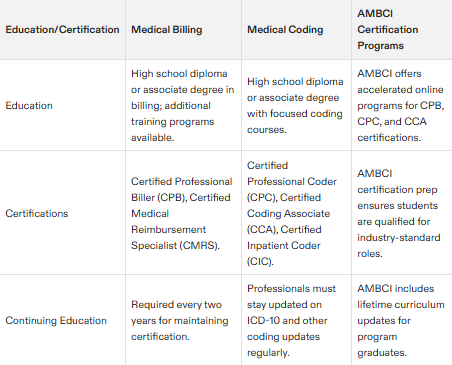
Educational requirements for medical billers and coders typically include a high school diploma or an associate degree in billing, coding, or both. Entry-level jobs often require completion of a certificate or associate degree program, which can be completed online in 8-20 months.
Employers usually prefer applicants certified in billing, coding, or both. Certifications can enhance hiring prospects, with CPB for billing and CPC or CCA for coding significantly boosting career potential and leading to higher responsibilities and pay.
Education for Medical Billers
Individuals aspiring to work in medical billing Require at least a high school diploma or an associate degree. There are specialized billing programs with durations of approximately seven months which equip students for various certification exams, such as CPB and CMRS, necessary to become certified professional billers.
These certification programs provide thorough training for prospective medical billers on comprehending insurance protocols and mastering the complexities of the billing procedures. To maintain their status as certified professionals, billers are required to update their certifications every two years by engaging in ongoing education to stay abreast of evolving industry regulations.
Education for Medical Coders
Medical coders must complete specific training programs to prepare for certification exams. These online programs typically take under 8 months and cover healthcare terminology, coding systems, and legal aspects, preparing students for exams like CPC or CIC.
Advanced certifications can greatly enhance a medical coder’s career, opening doors to specialized roles.
Work Environment and Job Outlook
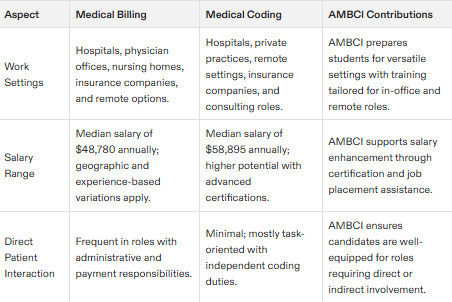
In the healthcare industry, individuals specializing in medical billing and coding occupy crucial positions within diverse settings such as hospitals, clinics, and insurance companies. There is an anticipated higher-than-average growth rate for jobs in these areas reflecting a robust demand.
Opting for a professional path in medical billing and coding might pave the way to opportunities like becoming a medical claims processor or assuming the role of health services manager. As of May 2023, specialists handling medical records, which cover both billers and coders, earn an average wage of around $48,780.
Work Environments for Medical Billers
Medical billers are typically employed in environments like hospitals and substantial healthcare facilities where direct interaction with patients is a part of the job. Their duties include collecting payments, inputting patient data, overseeing insurance claims, and managing the billing procedures.
These professionals fulfill administrative responsibilities aimed at maintaining precise invoicing and ensuring reimbursements as part of the healthcare revenue cycle. In contrast to coders, medical billers frequently engage directly with patients during their routine tasks.
Work Environments for Medical Coders
Often employed in hospitals or doctors’ offices, medical coders also have the option to work remotely. Flexibility is a common feature of many coding jobs, especially for those with experience.
With minimal direct engagement with patients, medical coders concentrate on independent tasks behind the scenes. Coding suits individuals well who prefer working independently and are task-oriented.
Salary Expectations
The average salaries for medical billers and coders vary across the United States. Factors such as experience, certification, and geographic location significantly impact earnings.
Career outcomes and earnings in medical billing and coding are influenced by experience, age, geography, market, and degree field. BLS estimates do not represent entry-level wages.
Average Salaries for Medical Billers
According to national data, medical billers can expect a median annual salary of about $48,780 in 2023. Previously, the estimated average income for this profession was around $42,000.
Geographical differences affect salaries. Regions such as New Jersey and the District of Columbia provide superior pay rates for those working as medical billers.
Average Salaries for Medical Coders
According to a 2023 survey, medical coders holding CPC certification earn a median annual income of around $58,895. This amount is indicative of the salary for certified medical coders as of the year 2023.
It should be noted that the salary for medical coders can differ significantly depending on their level of experience and certifications they possess. This highlights how crucial obtaining advanced certifications is in order to improve career opportunities and increase potential earnings.
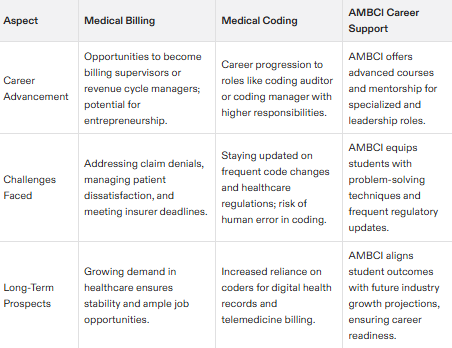
Career Pathways and Advancement
Career options in medical billing and coding include separate roles for billing and coding or combined roles. Many students pursue either field but also have the option to become specialists.
Certification as a medical biller or coder boosts career prospects and opens more opportunities. Potential career paths include health information management, with the job market projected to grow significantly faster than average.
Advancing as a Medical Biller
Individuals in medical billing can transition into management positions, overseeing billing departments or medical offices. With experience and further education, billers can become billing supervisors or revenue cycle managers.
Starting a business in medical billing is an option for those seeking entrepreneurial opportunities. Entrepreneurial billers may start their own companies, combining billing expertise with business management skills.
Advancing as a Medical Coder
Opportunities for career progression enable medical coders to experience professional development and assume roles that require specialization. These advanced positions include becoming a coding auditor or coding manager, which come with increased responsibilities and higher pay.
Common Challenges
In their respective roles, medical billers and coders encounter a variety of distinct challenges. Issues such as human error, the mishandling of claim submission deadlines, and dealing with rejected claims are prevalent in the realm of medical billing. The implementation of automated alerts and structured to-do lists can provide significant aid in navigating these difficulties more effectively.
The obligation for medical coders to stay abreast with modifications to coding protocols and shifts in healthcare regulations is crucial for adherence to compliance standards. Mistakes made by humans during the coding process may result in incorrect code allocations that lead insurers to refuse claims, underscoring the critical nature of precision within the coding procedure.
Challenges in Medical Billing
Navigating the complexities of medical billing, one notable obstacle is contending with human mistakes and overlooked deadlines for claim submissions. Such missteps result in rejected claims and delayed reimbursements, causing exasperation for both healthcare providers and their patients. To combat this issue, utilizing automated notifications and structured checklists can bolster the efficiency of medical billers in handling denied claims as well as guaranteeing punctual filing of claims.
Another obstacle comes from the escalated demands for information by insurance companies, which tend to decelerate the billing cycle and introduce challenges with adherence to regulations. The surging number of new cases coupled with disparate deadlines set by different insurers can contribute to payments being missed inadvertently – a scenario that often culminates in patient dissatisfaction.
Challenges in Medical Coding
Medical coders are required to keep abreast of the most recent updates and modifications in healthcare regulations, as this adherence is crucial for maintaining compliance. The relentless pace at which these changes occur demands their ongoing commitment to education and staying informed.
Coding inaccuracies often result from human errors, leading to claim rejections that can negatively impact the financial stability of healthcare providers. Insurance companies may refuse claims if incorrect medical codes are assigned, underscoring the critical need for precision within the coding process.
To circumvent such complications, it’s imperative for medical coders to meticulously ensure they allocate accurate diagnostic and procedure codes when documenting diagnoses according to current procedural terminology standards. This accuracy is essential in assigning procedure codes correctly and avoiding mishaps with insurance claims.
The Role of Technology
Innovations in technology have greatly improved the effectiveness of medical billing and coding. The introduction of automation and artificial intelligence has heightened precision while accelerating these operations, thereby diminishing mistakes and hastening payment cycles. This technological integration isn’t uniformly embraced as an industry norm. Its acceptance fluctuates among various healthcare organizations.
Ongoing progress in technological capabilities remains crucial for forthcoming enhancements within the realm of medical billing and coding. Incorporating tech solutions into these functions is not only about boosting operational efficiency, but also pertains to upholding adherence to intricate billing regulations and meticulous coding guidelines.
Technology in Medical Billing
Robotic Process Automation (RPA) has transformed the medical billing landscape, streamlining claim preparation and information collection while enhancing precision. These automated systems validate claims in real-time against insurer standards, reducing denials and elevating the efficiency of the billing workflow.
The merger of electronic health records with medical billing systems bolsters data precision and smooths out the entire billing cycle. Through this integration, essential patient details are meticulously recorded and incorporated into the billing routine, guaranteeing accuracy in billable information.
Technology in Medical Coding
The utilization of natural language processing in computer-assisted coding (CAC) has markedly transformed the practices of medical coding. Employing CAC streamlines the process, heightening both efficiency and precision, which minimizes potential errors.
Even though CAC boosts efficiency within medical coding operations, it necessitates a certain level of expertise to manage effectively and can be quite lengthy to integrate completely. This technology signifies an important advancement within the industry by guaranteeing precise adherence to established coding guidelines.
Summary
Medical billing and coding serve as fundamental components in the healthcare industry, each carrying out unique yet interrelated duties that are pivotal for precise billing and securing appropriate reimbursements. Medical coders have the task of converting medical procedures into uniform codes, whereas medical billers concentrate on processing and tracking insurance claims. These positions demand particular expertise, educational background, and certifications while providing multiple avenues for professional growth. Innovations in technology continue to bolster both efficiency and accuracy within these roles—addressing several typical hurdles encountered by those employed in this sphere. Recognizing how medical billing intersects with coding is key to appreciating their indispensable contributions to maintaining a robust healthcare revenue cycle.
Frequently Asked Questions
What is the main difference between medical billing and medical coding?
The main difference is that medical billing focuses on processing insurance claims for reimbursement, while medical coding involves converting medical procedures and diagnoses into standardized codes for billing purposes.
What skills are essential for a medical biller?
Essential skills for a medical biller include excellent communication and customer service abilities, strong organizational skills, and a solid understanding of coding conventions to ensure accurate billing management.
What certifications are available for medical coders?
Medical coders can pursue certifications like the Certified Professional Coder (CPC) and Certified Coding Associate (CCA), which significantly bolster career opportunities and specialization.
Can medical billers and coders work remotely?
Yes, many medical billers and coders can work remotely, especially if they have experience. This flexibility enables them to perform their tasks from home or other locations.
What are the salary expectations for medical billers and coders?
Medical billers can expect a median salary of about $48,780, while certified medical coders typically earn a median of around $58,895.
These figures can fluctuate based on factors such as experience, certification, and location.