ICD-11 Codes for Diabetes Mellitus: Complete Guide with Examples
Accurate ICD-11 coding for diabetes mellitus is essential for clinical documentation, insurance processing, and healthcare data integrity. ICD-11 offers precise, modular codes that capture the complexities of diabetes types, stages, and complications. Proper medical coding enables providers to tailor treatments, supports justified insurance claims, and feeds data into global health systems for research and policy-making. Incorrect coding can result in claim denials, delayed care, and compromised patient outcomes. ICD-11's enhanced specificity addresses these challenges, providing a robust framework for accurate, detailed documentation.
For healthcare coders and billing professionals, mastering these codes is critical. Accurate ICD-11 diabetes coding reflects provider credibility and ensures financial stability in a highly regulated environment. This guide delivers a concise yet comprehensive breakdown of diabetes mellitus ICD-11 codes, focusing on real-world application and compliance with global standards. From understanding classification categories to detailed case-based examples, we cover the essentials coders need. The ICD-11 diabetes coding course we offer equips learners with hands-on expertise, ensuring proficiency in this complex coding system. Mastering ICD-11 coding for diabetes mellitus is not an option—it’s a professional imperative.
What is ICD-11? An Overview
Evolution from ICD-10 to ICD-11
ICD-11 represents a major leap from ICD-10, offering more precise, modular, and globally aligned coding standards. The transition was driven by a need to accommodate advances in medical science, digital health integration, and nuanced clinical documentation. ICD-11 introduces unique alphanumeric codes and includes extensions to capture complications, severity, and temporal factors—enhancing the specificity of diabetes mellitus coding.
Key differences include updated terminology, flexible combination codes, and the inclusion of emerging diseases and conditions. For diabetes, ICD-11 moves beyond generic categories to incorporate granular details like subtypes, complications (nephropathy, neuropathy, retinopathy), and treatment factors. Unlike ICD-10’s limited scope, ICD-11’s design reflects evolving care standards, enabling more tailored patient management and resource allocation.
Global adoption has been underway since its 2019 release, with regulatory bodies like the WHO advocating its implementation. National health authorities are gradually shifting to ICD-11, mandating updates for billing systems, electronic health records (EHRs), and clinical protocols. The transition supports better interoperability, streamlined reporting, and improved public health tracking. For healthcare professionals, adapting to ICD-11 is critical for maintaining compliance and ensuring accurate, future-ready documentation.
Relevance of ICD-11 in Diabetes Care
ICD-11’s structure improves diabetes care by enabling comprehensive, accurate documentation. Its modular approach captures comorbidities, complications, and treatment nuances, essential for chronic conditions like diabetes. Enhanced coding specificity supports tailored care plans and resource planning.
Globally, ICD-11 aligns with updated clinical guidelines and health policies, ensuring consistent care across regions. The integration of detailed diabetes codes into EHRs streamlines workflows, reduces errors, and facilitates data-driven decision-making. Accurate ICD-11 diabetes coding strengthens clinical accountability and enhances patient outcomes by ensuring precise, actionable information flows through the healthcare system.
| Characteristic/Advantage | Details |
|---|---|
| Precision and Modularity | Enables detailed coding with modular extensions. |
| Updated Terminology | Modern medical language and flexible codes. |
| Detailed Diabetes Coding | Captures subtypes, complications, treatments. |
| Global Alignment | Consistent standards across countries. |
| Digital Health Integration | Compatible with EHR systems. |
| Enhanced Specificity | Comprehensive and tailored documentation. |
| Supports Tailored Care | Facilitates personalized care plans. |
| Regulatory Compliance | Adheres to updated billing and clinical protocols. |
| Improved Interoperability | Ensures system compatibility and data sharing. |
| Facilitates Public Health Tracking | Enables detailed reporting and health trend tracking. |
Classification of Diabetes Mellitus in ICD-11
Main Categories and Codes
ICD-11 provides a refined classification of diabetes mellitus, ensuring precise coding for each subtype and its complications. Diabetes is primarily categorized into Type 1, Type 2, gestational diabetes, and other specific types (e.g., monogenic, secondary). Each category carries distinct codes that reflect the underlying etiology and management nuances.
For example, Type 1 diabetes, marked by autoimmune β-cell destruction, is coded under 5A10, with extensions for complications like nephropathy (5A10.1), neuropathy (5A10.2), and ketoacidosis (5A10.0). Type 2 diabetes, reflecting insulin resistance and β-cell dysfunction, is captured under 5A11, with its own extensions for retinopathy (5A11.3), nephropathy (5A11.1), and foot ulcer (5A11.6). Gestational diabetes, unique to pregnancy, is identified under 5A14, with options to code severity and management (e.g., insulin use).
Real-world coding example: A patient with Type 2 diabetes presenting with nephropathy and neuropathy would be coded as 5A11.1 and 5A11.2, ensuring both complications are documented. This modular approach captures the full clinical picture, essential for tailored care and accurate reimbursement.
Coding for Complications and Comorbidities
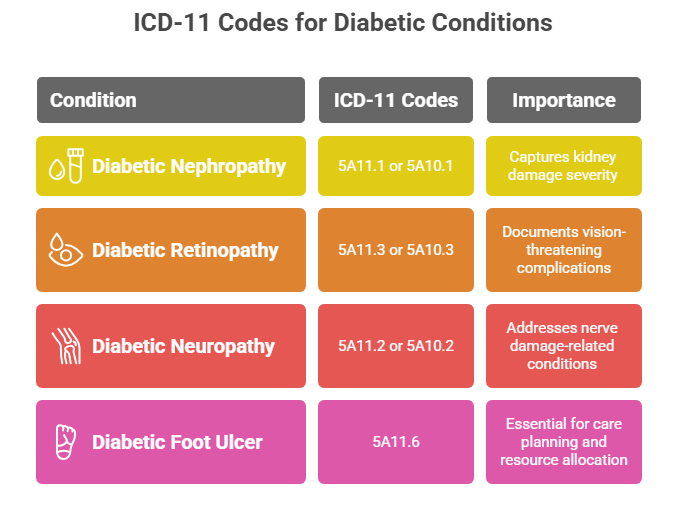
ICD-11 allows for detailed documentation of complications linked to diabetes, ensuring proper care coordination and financial compliance. Key codes cover:
Diabetic nephropathy (5A11.1 or 5A10.1) – capturing kidney damage severity.
Diabetic retinopathy (5A11.3 or 5A10.3) – documenting vision-threatening complications.
Diabetic neuropathy (5A11.2 or 5A10.2) – addressing nerve damage-related conditions.
Diabetic foot ulcer (5A11.6) – essential for care planning and resource allocation.
In complex cases, ICD-11’s modular system allows coders to combine primary diabetes codes with complication codes, ensuring precise and compliant billing. For example, a patient with Type 2 diabetes and multiple complications would have each aspect clearly coded—reflecting the patient’s full clinical profile.
Detailed ICD-11 Coding Guidelines for Diabetes
Step-by-Step Approach
Accurate ICD-11 coding for diabetes demands a methodical approach grounded in clinical documentation. Start by identifying the diabetes type—Type 1, Type 2, gestational, or other specified. Confirm the presence of complications such as nephropathy, retinopathy, neuropathy, or ketoacidosis. Note any comorbid conditions like hypertension or hyperlipidemia. Determine treatment specifics—whether insulin, oral medications, or lifestyle changes are prescribed.
Once identified, select the appropriate primary code (e.g., 5A11 for Type 2). Then, apply modular extensions to specify complications (e.g., 5A11.1 for nephropathy, 5A11.2 for neuropathy). Combine codes as needed to fully reflect the patient’s condition. Always verify code accuracy with updated ICD-11 reference materials.
Case study: A patient with Type 1 diabetes and proliferative retinopathy managed with insulin should be coded as 5A10.3 (retinopathy) and further refined with treatment codes if necessary. This ensures both the disease and management approach are documented, supporting reimbursement and compliance.
Common Coding Pitfalls
Errors in diabetes coding are common. These include using generic codes that fail to capture complications, omitting combination codes for multiple conditions, and misclassifying diabetes types. Coders must stay vigilant to avoid misinterpretation, as errors can delay claims or compromise care quality. Always reference the latest ICD-11 updates and double-check documentation.
Tips for Accurate Coding
Review clinical documentation thoroughly before assigning codes.
Use modular extensions in ICD-11 to specify all complications and treatments.
Stay updated with coding changes through webinars and guidelines.
Validate codes using official ICD-11 coding resources or internal auditing systems.
Communicate with providers when documentation is unclear to avoid assumptions.
Proficient ICD-11 diabetes coding is a cornerstone of accurate reimbursement and patient safety. Coders must commit to continuous learning and proactive quality checks.
Practical Examples of ICD-11 Diabetes Codes
Example 1: Type 1 Diabetes with Nephropathy
A patient with longstanding Type 1 diabetes presents with early-stage nephropathy and insulin dependence. The primary code is 5A10 (Type 1 diabetes mellitus). The nephropathy is captured with 5A10.1. Insulin treatment can be documented through extensions if required.
Clinical rationale: The coder combines the primary and modular codes to reflect both the disease and complication. This precision ensures accurate billing and care planning.
Example 2: Type 2 Diabetes with Multiple Complications
Consider a patient with Type 2 diabetes experiencing both retinopathy and neuropathy. The primary code is 5A11 (Type 2 diabetes mellitus). Retinopathy is captured with 5A11.3, and neuropathy with 5A11.2. If the patient also presents with a diabetic foot ulcer, code 5A11.6 applies.
Clinical rationale: Each complication code enhances clarity in documentation, supporting comprehensive care and compliance.
Example 3: Gestational Diabetes
A pregnant patient is diagnosed with gestational diabetes, managed with dietary changes and insulin. The primary code is 5A14 (Gestational diabetes mellitus). Modular codes specify the management strategy if needed.
Clinical rationale: Correct coding ensures accurate monitoring of both maternal and fetal health, while supporting claim processing.
| Scenario | Primary Code | Complication Codes | Management Codes |
|---|---|---|---|
| Type 1 Diabetes with Nephropathy | 5A10 | 5A10.1 | Insulin extension codes if applicable |
| Type 2 Diabetes with Retinopathy and Neuropathy | 5A11 | 5A11.3, 5A11.2 | Oral agents/insulin extensions if applicable |
| Gestational Diabetes Managed with Diet and Insulin | 5A14 | None | Diet and insulin extension codes |
How AMBCI’s Certification Prepares You to Code Diabetes Accurately in ICD-11
Comprehensive Training for Medical Coders
Our Medical coding course delivers hands-on, in-depth training for coders, billing specialists, and clinical documentation experts. It’s designed to translate complex coding frameworks into practical, real-world skills. Through instructor-led modules, participants learn how to navigate the detailed structure of ICD-11, with a focus on diabetes mellitus coding. Real-life case studies, coding simulations, and interactive exercises help learners confidently master primary codes, complications, and modular extensions.
The course isn’t just about memorizing codes—it’s about understanding the logic behind ICD-11’s architecture. By completing our program, coders will gain the competence to document complex diabetes cases with accuracy and compliance, directly supporting providers’ revenue cycles and patient care quality.
Access to Updated ICD-11 Resources
The training program includes access to an updated suite of coding resources—ranging from comprehensive ICD-11 code libraries, practical reference charts, to official guideline updates. Participants can stay ahead of evolving standards, ensuring long-term proficiency.
Additionally, the course offers mentorship from experienced instructors who provide insights into common pitfalls, documentation nuances, and coding optimization strategies. This combination of resources and expert guidance equips coders with a competitive edge in mastering ICD-11 diabetes coding.
Final Thoughts
Mastering ICD-11 coding for diabetes mellitus is no longer optional—it’s a necessity for healthcare providers, coders, and billing specialists navigating today’s complex clinical landscape. ICD-11’s modular structure, enhanced specificity, and real-world adaptability make it an essential tool for accurately documenting diabetes cases, from simple diagnoses to those complicated by comorbidities and complications. Precise coding ensures timely, justified reimbursement and fosters continuity of care by communicating critical patient details across clinical teams.
Our ICD-11 diabetes coding course equips professionals with the expertise to apply this system effectively. By learning through real-life cases, updated code libraries, and hands-on simulations, coders gain the proficiency to excel in a competitive field. As ICD-11 evolves, staying updated and continually refining coding skills will be vital. Mastering this system isn’t just about compliance; it’s about empowering patient care, ensuring operational efficiency, and future-proofing your career in healthcare coding.
Frequently Asked Questions
-
ICD-11 is the 11th revision of the International Classification of Diseases, developed by the World Health Organization (WHO) to provide a modern, digital-friendly coding system for healthcare conditions. It classifies Diabetes Mellitus with detailed modular codes that specify disease types, severity, and complications. Type 1 diabetes is identified under 5A10, Type 2 under 5A11, and gestational diabetes under 5A14, with additional extensions for complications like nephropathy or neuropathy. ICD-11’s structure improves precision in documenting diabetes, ensuring accurate clinical records, data reporting, and billing processes. Its design supports a global, standardized approach to diabetes care, essential for providers, payers, and policymakers worldwide.
-
ICD-11 offers a more modular and detailed approach compared to ICD-10. While ICD-10 provided a limited set of codes for diabetes, ICD-11 introduces extensions that capture the specific type, complications, and severity in one system. For example, ICD-11’s codes like 5A11.1 (Type 2 diabetes with nephropathy) are more specific than ICD-10’s broad E11.21 category. Additionally, ICD-11 integrates digital compatibility, improved terminology, and alignment with global clinical guidelines, offering healthcare professionals a comprehensive framework. This upgrade enhances accuracy in coding and supports better decision-making, reimbursement, and global health monitoring for diabetes management.
-
ICD-11 classifies diabetes into specific categories: 5A10 for Type 1 diabetes mellitus, with extensions like 5A10.1 for nephropathy and 5A10.3 for retinopathy; 5A11 for Type 2 diabetes mellitus, with codes such as 5A11.1 for nephropathy and 5A11.2 for neuropathy; and 5A14 for gestational diabetes mellitus, which captures pregnancy-related cases. ICD-11 also includes codes for other diabetes forms like monogenic or secondary diabetes under broader categories, using detailed extensions to document complications. These codes enable precise documentation, tailored treatment plans, and justified reimbursement, which are critical in today’s data-driven healthcare systems.
-
ICD-11 introduces a modular system where complications of diabetes are coded as extensions to the primary diabetes code. For example, nephropathy is coded as 5A11.1 (for Type 2) or 5A10.1 (for Type 1), retinopathy as 5A11.3/5A10.3, and neuropathy as 5A11.2/5A10.2. This modularity allows coders to document multiple complications precisely, ensuring the full clinical picture is reflected. Additionally, ICD-11 supports combination coding, where a patient with multiple complications (e.g., nephropathy and retinopathy) can have all conditions accurately coded. This precision is essential for comprehensive diabetes care documentation, streamlined reimbursement, and proactive treatment planning.
-
Precise ICD-11 coding ensures diabetes is properly classified, reflecting its type, severity, and complications. Accurate coding informs clinical decisions, supports tailored treatment plans, and facilitates care continuity between providers. It ensures healthcare organizations submit valid claims, minimizing reimbursement denials and audit risks. From a public health perspective, correct ICD-11 coding feeds into global data systems, enabling epidemiological studies, resource allocation, and policy development. In complex cases involving comorbidities, ICD-11’s detailed coding ensures no aspect of a patient’s condition is overlooked, ultimately improving outcomes, enhancing patient safety, and supporting financial stability in healthcare delivery.