Is Penn Foster Medical Billing and Coding Accredited?
When considering an online program for medical billing and coding, one of the most important questions is whether the program is accredited. Accreditation ensures the quality and reliability of the education, which can influence career prospects and eligibility for financial aid. Penn Foster's Medical Billing and Coding program has garnered attention for its self-paced learning and comprehensive curriculum. But before enrolling, it’s important to understand how accreditation factors into this program.

What is Medical Billing and Coding?
Medical billing and coding are crucial parts of the healthcare industry. These roles ensure that medical providers are paid accurately and promptly for their services. Medical billing involves submitting claims to insurance companies and government programs, ensuring that healthcare providers receive reimbursement. Medical coding, on the other hand, involves translating diagnoses, procedures, and services into standardized codes. These codes are essential for insurance purposes, patient records, and billing. Obtaining a medical billing and coding certification from AMBCI can help professionals gain the necessary expertise in coding systems such as ICD-10 (International Classification of Diseases) and CPT (Current Procedural Terminology), improving career opportunities in the field.
Importance of Accreditation
Accreditation is vital for any medical billing and coding program because it signifies that the program meets industry standards and prepares students for certification exams. Leading accrediting bodies in this field include the American Health Information Management Association (AHIMA), the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM), and the American Academy of Professional Coders (AAPC). Programs that are accredited by these bodies ensure that students receive a high-quality education that aligns with the skills and knowledge needed to succeed in the workforce. Furthermore, accreditation often enables students to qualify for financial aid and is favored by potential employers.
Penn Foster Medical Billing and Coding Program Overview
Penn Foster offers a Medical Billing and Coding Career Diploma Program that aims to prepare students for a career in this growing field. This program is designed to be self-paced, allowing students to study and complete coursework at their convenience. The curriculum covers vital topics such as medical terminology, anatomy, physiology, and coding systems like ICD-10 and CPT. Penn Foster's program is designed to give students the knowledge and skills they need to pass certification exams and secure entry-level positions in the field.

Benefits of Enrolling in an Accredited Program
Enrolling in an accredited medical billing and coding program offers several advantages. First, it ensures that students receive a high-quality education that meets industry standards. Additionally, employers tend to favor graduates from accredited programs because these programs better prepare students for the challenges of the job. Accreditation also opens the door to financial aid options, as many funding opportunities require students to be enrolled in accredited programs. Moreover, students graduating from accredited programs are better positioned to succeed in certification exams, which can lead to higher salaries and career advancement.
Career Opportunities in Medical Billing and Coding
Graduates of medical billing and coding programs can pursue a variety of career opportunities across healthcare settings such as hospitals, clinics, private practices, and even insurance companies. Positions available include certified medical billers, certified medical coders, medical coding specialists, and billing consultants. Many professionals also choose to start their own medical billing and coding businesses. The demand for skilled professionals in this field is high, and the job outlook for medical billers and coders remains positive.
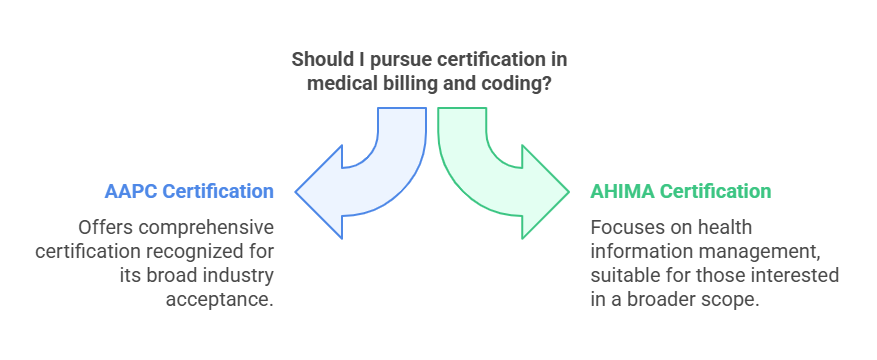
Medical Billing and Coding Certification Exams
Certification exams are an important step for aspiring medical billers and coders. These exams assess the knowledge and expertise needed to succeed in the field. Professional organizations like AAPC and AHIMA offer certification exams that can help individuals demonstrate their proficiency. Earning certification not only enhances job prospects but can also lead to higher earning potential. Moreover, most employers prefer or require certification, making it a key component of a successful career in medical billing and coding.
Continuing Education and Professional Development
After obtaining certification, medical billing and coding professionals are required to engage in continuing education to maintain their certification. Continuing education ensures that professionals stay up-to-date with the latest industry trends, regulations, and technologies. It can be completed through workshops, online courses, or conferences. By continually enhancing their skills, professionals can improve their career prospects and increase their earning potential.
Penn Foster Alumni Reviews and Testimonials
Penn Foster alumni have shared positive feedback about their experiences in the Medical Billing and Coding program. Many alumni appreciate the flexibility of the self-paced program, which allows them to balance their studies with other responsibilities. Others highlight the program's comprehensive curriculum, which prepares them for certification exams and real-world work in medical billing and coding. Additionally, alumni have noted that the program is affordable and offers a quality education, which provides a strong foundation for their careers.
Choosing the Right Medical Billing and Coding Program
When selecting a medical billing and coding program, it's essential to consider the program's accreditation status, as this ensures that the education meets industry standards. Additionally, the curriculum should cover essential topics such as medical terminology, anatomy, physiology, and coding systems. Prospective students should also evaluate the program's format, whether it’s self-paced or traditional, and determine whether it fits their lifestyle and learning preferences. Lastly, cost is an important consideration, and students should weigh the value of the program against its price.

Less Known Facts about Medical Billing and Coding
1. High Demand for Coders: The demand for medical records specialists, including medical coders, is projected to grow due to an aging population and evolving healthcare regulations. Bureau of Labor Statistics
2. Specialization Opportunities: Medical coders can obtain specialty certifications in areas such as cardiology and anesthesia, enhancing their expertise and potentially leading to higher pay and job security. Penn Foster
3. Medical Billing vs. Coding: Medical coding involves translating medical procedures into standardized codes, whereas medical billing focuses on submitting claims and obtaining payment for healthcare services. AAPC
4. Remote Work Opportunities: Numerous medical billing and coding positions offer remote work options, providing professionals the flexibility to work from home.
5. Certification Exam Prep: Organizations like AAPC provide study guides and practice exams to assist students in preparing for medical coding certification exams. Amazon+5AAPC+5AAPC+5
6. Technology’s Role: Automation and artificial intelligence are increasingly utilized in medical coding to enhance accuracy and efficiency. Healthcare IT News
FAQs
-
Medical billing involves submitting claims to insurance companies for reimbursement, while medical coding involves assigning standardized codes to diagnoses and procedures.
-
While certification is not always required, it is highly recommended and often preferred by employers.
-
Yes, many medical billing and coding professionals have the option to work remotely, depending on their employer.
-
Penn Foster’s program is self-paced, so the length of time to complete it depends on how quickly you can progress through the coursework. On average, students may complete the program in 9-12 months.
-
The job outlook for medical billing and coding professionals is strong, with a projected growth rate of 8% through 2031, according to the Bureau of Labor Statistics.
Conclusion
In conclusion, Penn Foster’s Medical Billing and Coding program offers a flexible, self-paced way to gain the knowledge and skills necessary for a successful career in this growing field. While the program is not currently accredited by major accrediting bodies, it can still provide a strong foundation for those looking to enter the workforce. However, students are encouraged to choose an accredited program for greater career advancement opportunities. Additionally, obtaining certification and engaging in continuing education are crucial steps for long-term success in this industry.
