Mastering Revenue Cycle Management: Complete Guide
Effective Revenue Cycle Management (RCM) is the backbone of every successful healthcare operation. Without it, even the best clinical care risks being undermined by delayed payments, denied claims, and broken cash flow. In 2025’s rapidly evolving healthcare economy, mastering the full spectrum of RCM—from patient intake to final payment—is not just a priority, it’s a survival strategy.
Medical billing workflows are becoming increasingly complex, yet the demand for speed, accuracy, and compliance has never been higher. This guide breaks down the essential components, systems, and strategies behind RCM best practices, giving you the clarity to optimize revenue and avoid costly pitfalls. Whether you're managing a small clinic or overseeing an enterprise-level operation, this roadmap delivers actionable, real-world value.
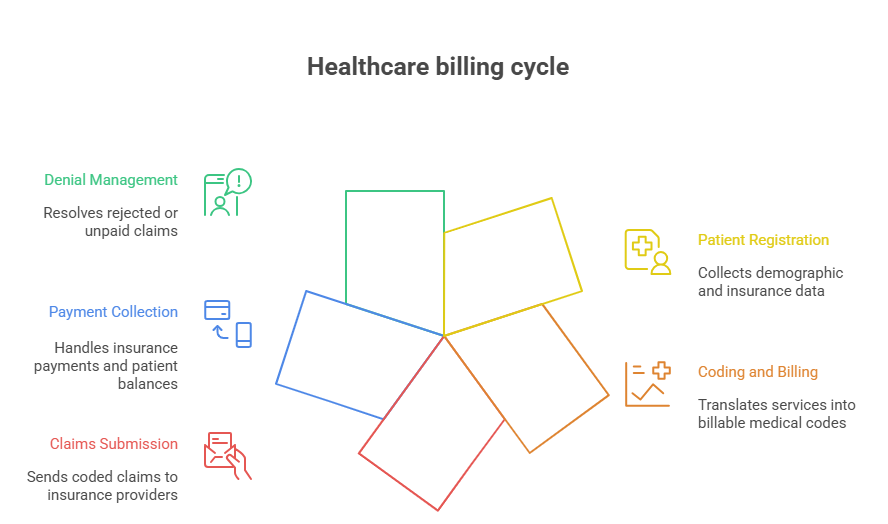
Understanding the Key Components of RCM
An optimized Revenue Cycle Management (RCM) system depends on each stage of the revenue journey functioning with precision. From the moment a patient schedules an appointment to the final balance payment, every step must be aligned with both compliance and efficiency goals.
Patient Registration
This is where clean data begins. Accurate patient demographics, insurance details, and referral documentation reduce errors downstream. Verification upfront prevents claim denials later. Many providers still lose thousands annually due to missing or incorrect information collected at intake.
Coding and Billing
After services are rendered, CPT and ICD-10 codes must accurately reflect the patient’s treatment. Errors here trigger audits, denials, or delayed payments. Efficient billing departments use coding software and internal audits to catch mistakes early and ensure claims are clean and compliant before submission.
Payment Collection and Denial Management
Once claims are sent, tracking and follow-up begin. Payment posting must be timely, and denial trends should be analyzed to find root causes. A robust denial management process includes prompt appeal filing, staff retraining, and system audits. Preventive action is more valuable than reactive cleanup.
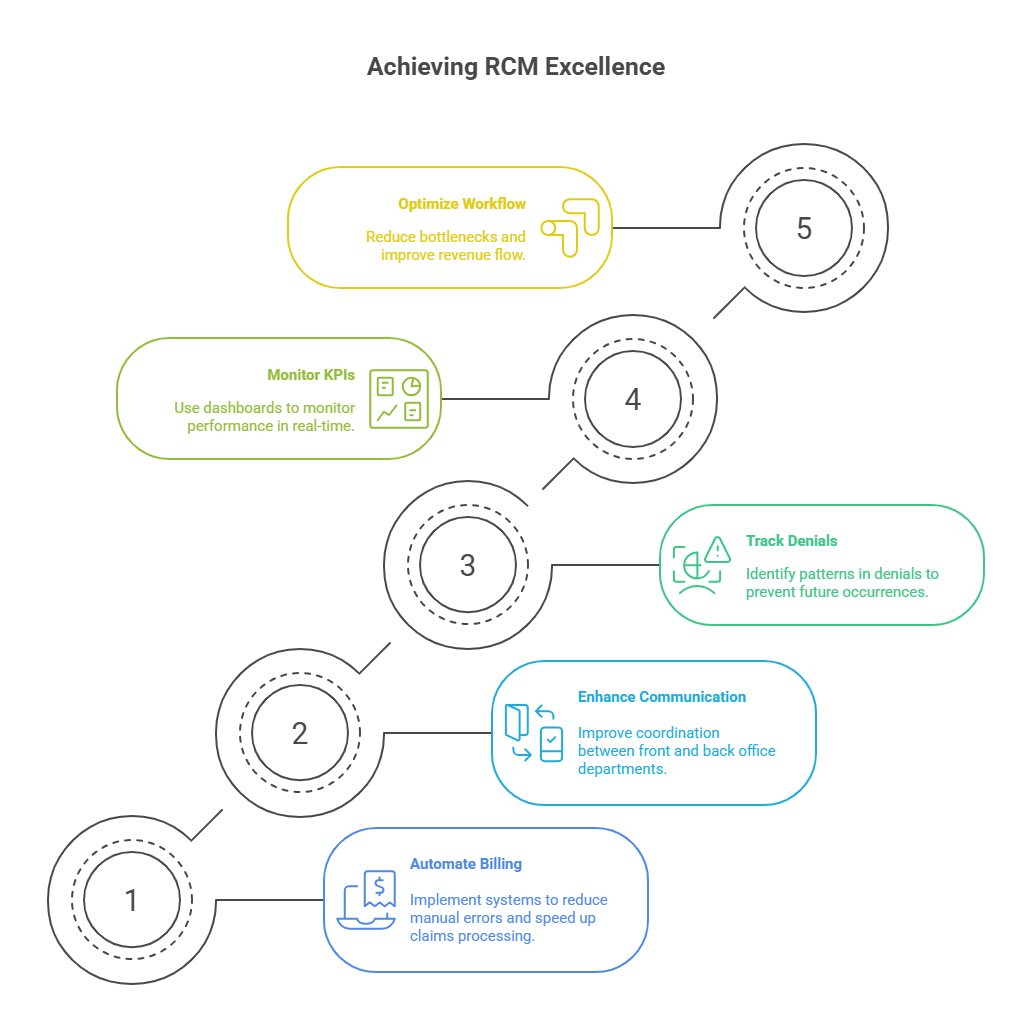
Streamlining RCM Processes
A streamlined Revenue Cycle Management (RCM) process increases both revenue capture and patient satisfaction. Reducing inefficiencies and improving accuracy at each phase leads to faster reimbursements and fewer denials. Strategic adjustments can yield exponential improvements.
Automating Billing and Claims
Automation tools can eliminate human error in repetitive tasks. From claim scrubbing software to automated eligibility checks, technology reduces friction. When properly implemented, automation cuts claim submission time, minimizes rework, and improves cash flow predictability.
Improving Communication Between Departments
Revenue leakage often stems from poor internal coordination. Aligning front desk, clinical, and billing teams ensures accurate handoffs and unified data. Clear workflows supported by shared documentation and system visibility reduce duplicate tasks and prevent billing delays due to miscommunication.
Reducing Denials
Preventing denials requires upstream attention. Regular audits should target recurring errors in coding, eligibility, and documentation. Addressing these at the root through training and process tweaks saves thousands. Successful RCM departments build dashboards that flag trends before they spiral into major revenue loss.
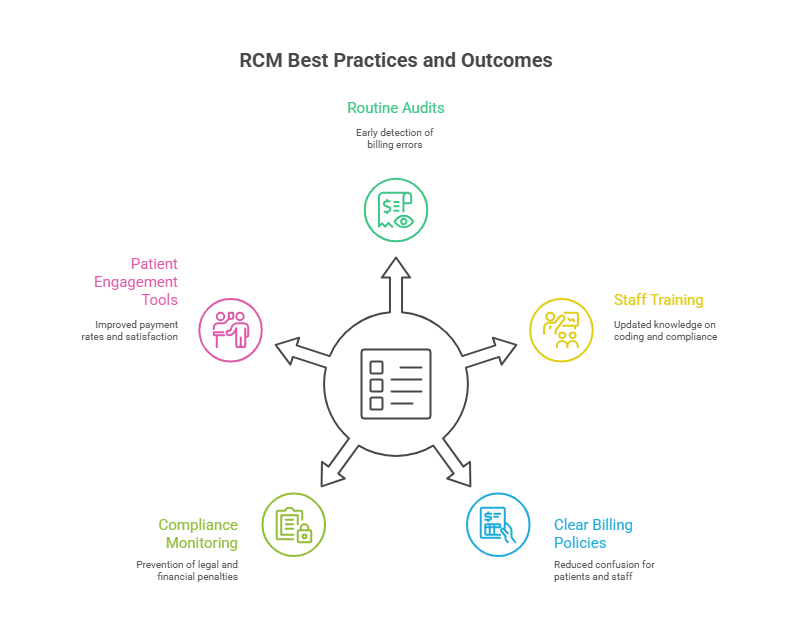
Implementing Best Practices for RCM
Strong Revenue Cycle Management is built on consistent adherence to proven operational standards. The best-performing organizations don’t just react to billing problems — they proactively prevent them through robust systems and a well-trained workforce.
Regular Auditing and Compliance
Ongoing audits help catch inaccuracies in documentation, coding, and charge capture before claims are submitted. By auditing a sample of encounters weekly or monthly, organizations stay compliant with regulatory standards and avoid penalties. Audits also uncover bottlenecks that reduce reimbursement efficiency.
Staff Training and Education
Your team is your strongest asset in RCM. Regular training sessions improve accuracy, especially in ICD-10 coding, payer policies, and software updates. It also reduces dependency on a few “experts” by spreading institutional knowledge across the team. Upskilling also boosts employee retention and morale.
Enhancing Patient Experience and Engagement
RCM isn’t just about numbers — it’s also about clear communication and ease of access. Providing user-friendly patient portals, transparent cost estimates, and responsive billing support improves both collections and patient satisfaction. When patients understand their bills, they’re more likely to pay on time.
Key Technology Tools for RCM
Technology is no longer optional in modern revenue cycle management. To keep pace with rising patient volumes and evolving payer demands, medical practices must leverage tools that improve efficiency and accuracy.
Practice Management Systems (PMS)
A strong PMS integrates scheduling, billing, and claims into one platform. It reduces manual entry errors, tracks patient eligibility in real-time, and manages claims end-to-end. PMS platforms are central to streamlining front-end and back-end workflows.
Electronic Health Records (EHR) Integration
When your EHR syncs with billing, it minimizes the chances of miscommunication between clinical and financial departments. Proper documentation flows seamlessly into coding, ensuring fewer rejected claims and faster reimbursement.
Claims Management and Scrubbing Software
Claims scrubbing tools flag errors before submission. This reduces denials and increases first-pass resolution rates. These tools also allow revenue cycle teams to track claims status, identify patterns in payer rejections, and adjust proactively.
Patient Payment Portals and Automation
With more patients paying out of pocket, offering self-service portals that accept credit cards, payment plans, and insurance information is critical. Automating payment reminders and follow-ups boosts collections while reducing administrative workload.
| Tool Type | Function |
|---|---|
| EHR Systems | Integrate clinical and billing data |
| Claims Management Software | Tracks claim status and automates submissions |
| Billing Analytics Tools | Provides insights into payment trends |
| Eligibility Verification Tools | Confirms insurance before treatment |
| Payment Gateways | Facilitates online payments |
Overcoming Common RCM Challenges
Even with the best tools and workflows, revenue cycle management faces real-world friction. Addressing these obstacles is essential to maintain cash flow and patient satisfaction.
Staff Shortages
High turnover in billing departments can cause delays, errors, and knowledge gaps. The solution is to invest in cross-training staff, document all processes clearly, and implement automated systems to reduce dependency on manual labor. Lean teams can operate efficiently with the right tech stack.
Compliance Issues
Healthcare regulations change frequently — from HIPAA requirements to payer-specific rules. Staying compliant means continuously updating internal policies and using software that flags compliance gaps. Regular audits and certification training for billing staff ensure your team stays ahead.
Patient Payment Concerns
As more healthcare costs shift to patients, collecting payments has become harder. To overcome this, offer flexible payment plans, transparent upfront estimates, and automated reminders. Educating patients at check-in about their responsibilities boosts the chances of timely payment.
| Challenge | Solution |
|---|---|
| Staff Shortages | Cross-training and flexible staffing |
| Compliance Risks | Ongoing education and audits |
| Late Patient Payments | Automated reminders and online portals |
| Denial Volume | Root cause analysis and better documentation |
| Outdated Systems | Investing in cloud-based RCM tools |
How AMBCI’s Medical Billing and Coding Certification Equips You for RCM Success
To lead in revenue cycle management, formal training isn’t optional—it’s your edge. The Medical Billing and Coding Certification by AMBCI arms you with the precise skills needed to excel in today’s high-pressure medical admin environments.
You’ll master coding accuracy, payer policies, and compliance standards—all critical components of effective RCM. The curriculum also covers real-world scenarios around claims management, denial resolution, and billing workflows, giving you tactical experience.
Certification also signals credibility to employers. Clinics, hospitals, and third-party billing services prioritize certified professionals who understand the financial anatomy of healthcare. Whether you’re entering the field or aiming to level up, AMBCI’s certification bridges the gap between knowledge and execution.
Frequently Asked Questions
-
A medical biller plays a crucial role in ensuring smooth revenue flow for healthcare providers. Their primary responsibility is to translate healthcare services into billable claims, submit them to insurers, and track payments or denials. They verify insurance coverage, collect co-pays, and follow up on unpaid claims. Accuracy is key — errors in billing can lead to claim denials and delayed revenue. A certified biller, such as one holding the Medical Billing and Coding Certification by AMBCI, ensures compliance with regulatory standards, helping facilities maximize reimbursements and minimize financial risks. Billers serve as the financial backbone of any practice, making their role indispensable in the revenue cycle process.
-
Correct medical coding directly determines how much a healthcare provider gets paid. Coders assign ICD-10, CPT, and HCPCS codes to patient services, which insurers use to process claims. Inaccurate or outdated codes can lead to claim rejections, audits, or underpayment. To ensure maximum reimbursement, coders must stay updated with payer-specific rules and changing guidelines. A single miscoded procedure can cost thousands in lost revenue. That’s why many employers prefer professionals certified through the Medical Billing and Coding Certification by AMBCI, as they are trained in the most current standards and compliance protocols. Coding isn’t just administrative — it’s critical to the financial health of any practice.
-
The top causes of claim denials include incorrect patient information, missing codes, duplicate claims, lack of prior authorization, and timely filing issues. Even a typo in the patient’s name or policy number can halt payment. Payers also reject claims lacking medical necessity documentation. To reduce denials, practices must implement claim scrubbing tools and ensure all data is clean and complete before submission. Trained professionals, especially those certified by AMBCI, are taught to spot red flags and correct them proactively. Denial management is not about fixing mistakes—it’s about preventing them, which directly improves a practice’s bottom line and cash flow stability.
-
Modern RCM platforms automate the entire billing workflow, from patient registration to payment posting. These systems reduce manual entry, prevent errors, and accelerate the claim lifecycle. Built-in alerts flag missing data before submission, while dashboards allow real-time tracking of A/R aging and denials. Some tools also integrate AI-driven coding assistance and payer-specific rules. Practices that adopt these platforms often report 20–40% faster reimbursement cycles. RCM tools also make it easier to stay compliant with HIPAA and payer updates. Professionals trained through the Medical Billing and Coding Certification by AMBCI often get hands-on exposure to these tools, making them more job-ready.
-
Key performance indicators (KPIs) for RCM include Days in Accounts Receivable (A/R), First Pass Resolution Rate (FPRR), Clean Claim Rate, Denial Rate, and Net Collection Rate. For instance, a clean claim rate above 95% signals efficient front-end processes. A denial rate over 10% may point to issues in documentation or coding. Monitoring Days in A/R helps practices understand how long it takes to collect after service delivery — the lower, the better. Regularly analyzing these KPIs enables data-driven decisions to improve cash flow and reduce revenue leakage. Certification programs like AMBCI’s teach students how to track and interpret these metrics effectively.
-
Compliance is the foundation of sustainable revenue cycle management. Healthcare facilities must align with HIPAA, CMS, and payer-specific regulations, or risk fines, audits, and payment clawbacks. Audits—whether internal or external—examine claims for documentation, coding accuracy, and billing patterns. Non-compliance can cost millions and severely harm a facility’s reputation. Certified professionals are trained to create audit-ready documentation, follow correct coding protocols, and implement internal controls. The Medical Billing and Coding Certification by AMBCI includes in-depth training on legal and ethical standards, empowering professionals to build compliant, audit-resistant billing systems that protect revenue and reduce operational risks.
-
Getting certified boosts your credibility, employability, and income potential. Employers prefer certified candidates because they bring verified expertise, lower error rates, and better compliance awareness. Certification also ensures you're fluent in industry-standard coding systems, including ICD-10, CPT, and HCPCS. AMBCI’s Medical Billing and Coding Certification goes beyond theory — it includes practical training on real-world tools and payer workflows. It’s a signal to employers that you're serious about your career and prepared to handle the complexities of revenue cycle management. In a competitive job market, certification can be the difference between getting hired and getting passed over.
Conclusion
Mastering revenue cycle management (RCM) is no longer optional — it's essential for healthcare providers aiming for financial sustainability and growth. From patient intake to final payment posting, each step in the RCM chain impacts the cash flow, compliance, and patient satisfaction. Practices that fail to streamline these processes face mounting denials, delayed reimbursements, and avoidable revenue loss.
Integrating best practices, adopting smart RCM tools, and training staff with up-to-date knowledge is how high-performing organizations stay ahead. A certified billing professional — especially one with the Medical Billing and Coding Certification by AMBCI — brings the precision, compliance mindset, and operational insight needed to transform messy systems into revenue engines.