20 Best Medical Biller Interview Questions and Answers for 2025
Preparing for a medical biller interview? Look no more. As we have gathered the crucial interview questions and answers for medical billers that will assist you in excelling. Learn to demonstrate your expertise in coding, mastery of relevant software, and comprehension of healthcare regulations effectively with our guide designed to help you leave an outstanding impression. Additionally, showcasing your problem-solving skills through specific examples of past experiences, such as identifying problems, implementing solutions, and learning from those situations, will be crucial.
Key Takeaways
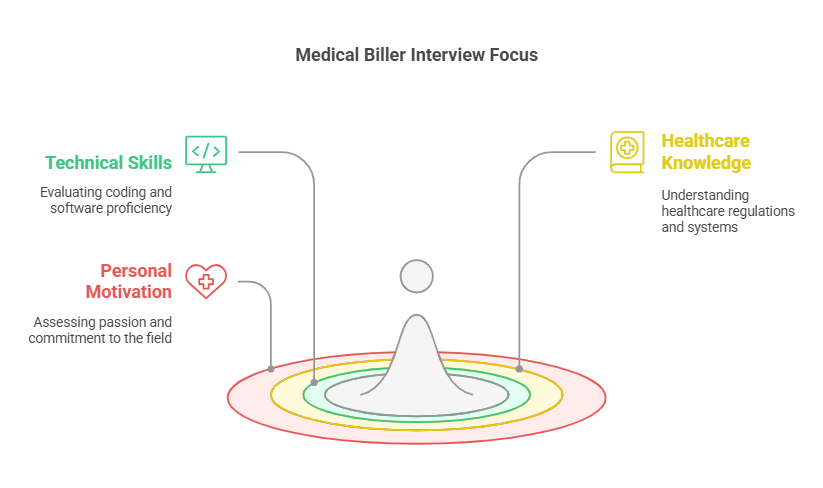
Medical biller interviews assess technical skills, knowledge of healthcare regulations, and proficiency in coding systems, emphasizing the need for attention to detail and problem-solving skills.
Candidates should demonstrate their experience with patient registration, handling claim denials, and ensuring compliance with HIPAA guidelines to illustrate their competence in managing complex billing scenarios.
Continuous professional development, including staying updated on coding changes and participating in industry associations, is essential for success and growth in the medical billing profession.
Introduction to Medical Billing
Medical billing is a critical process in the healthcare industry that involves submitting and following up on claims with health insurance companies to receive payment for healthcare services rendered by a provider. It is a complex process that requires a deep understanding of medical coding, billing regulations, and healthcare practices. Medical billing ensures that healthcare providers are compensated for their services, enabling them to maintain a steady cash flow and continue delivering quality care to patients.
What is Medical Billing?
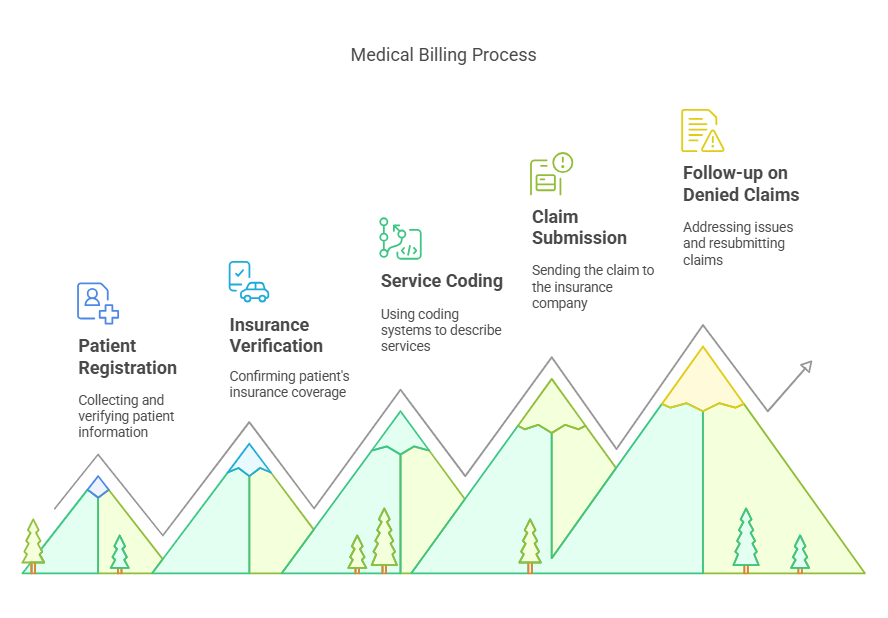
Medical billing is the process of translating healthcare services rendered by a provider into a billing claim. The claim is then submitted to insurance companies for payment. The process involves several steps, including patient registration, verification of insurance, coding of services, claim submission, and follow-up on any denied claims. Obtaining a medical billing certification from reputable institutions like AMBCI ensures that professionals are well-equipped to handle the complexities of the billing process. Medical billing is a crucial aspect of the healthcare industry, as it enables healthcare providers to receive payment for their services and maintain a steady cash flow.
Accurate patient registration is the first step in the medical billing process, ensuring that all necessary patient information is collected and verified. This is followed by the coding of services using standardized coding systems such as ICD-10, CPT, and HCPCS. These codes are essential for accurately describing the services provided and ensuring proper reimbursement. Once the claim is prepared, it is submitted to the insurance company for review and payment. Medical billers must then follow up on any denied claims, addressing any issues and resubmitting the claims as necessary.
Key Medical Biller Interview Questions
Within the domain of medical billing, interview sessions aim to gauge an applicant’s expertise in technical aspects, grasp of healthcare frameworks, and their compliance with billing standards. Primary inquiries are aimed at determining competency in medical coding tasks, knowledge level regarding usage of billing software systems, and understanding pertinent to healthcare regulations.
Submitting claims accurately and efficiently is a key responsibility in medical billing, ensuring proper payment for healthcare services and maximizing reimbursement by following up on unpaid claims.
Grasping the complex nature of the billing cycle is essential for ensuring precision in charges rendered and adherence to regulatory practices. To gear up thoroughly for your upcoming medical billing interview session, consider these important questions that can serve as a robust preparation guide.
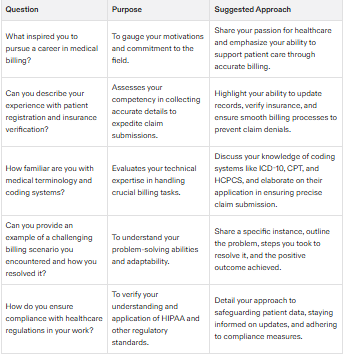
What inspired you to pursue a career in medical billing?
Many individuals are drawn to medical billing due to a passion for the medical field and a desire to support patient care. The stability offered by the profession and the continuous learning opportunities also make it an attractive career choice.
Employers often look to understand your motivations and personal connection to the field. Expressing your passion for healthcare and your commitment to the efficiency of healthcare services can distinguish you as a dedicated candidate.
Can you describe your experience with patient registration and insurance verification?
The collection of vital patient information during the initial phase of patient registration is a pivotal element in the medical billing cycle, as it facilitates precise billing and expedites claim submissions. Ensuring that both patient registration details and insurance verification are current and correct is key to preventing postponements and rejections of claims. Accurate patient registration and insurance verification play a crucial role in efficiently submitting claims to insurance companies.
Applicants should emphasize their proficiency in keeping accurate records updated for both patients’ personal information and insurer data, along with their capability to tackle frequent issues like misdirected claims due to erroneous addresses.
How familiar are you with medical terminology and coding systems?
Understanding medical terminology is essential for medical billers, as it allows them to correctly understand clinical records, a key component in efficient billing practices. Being well-versed in predominant coding systems such as ICD-10, CPT, and HCPCS is vital for the precise filing of claims and securing appropriate compensation for provided services.
The proficiency of medical billers in both medical terminology and various coding systems plays a significant role in reducing mistakes and speeding up the payment process during claim submissions.
Handling Complex Billing Scenarios
Navigating the intricacies involved in medical billing is a fundamental part of the job for those working in this field. It is vital to possess keen attention to detail when managing claims and swiftly resolving any issues related to insurance payments. Strong problem-solving skills are essential in navigating complex billing scenarios and resolving issues related to insurance payments.
During interviews, questions are geared toward evaluating an applicant’s ability to solve problems effectively and their aptitude for dealing with difficult situations that arise within medical billing. The following suggestions aim at addressing typical complex billing scenarios encountered in this role.
Can you provide an example of a challenging billing scenario you encountered and how you resolved it?
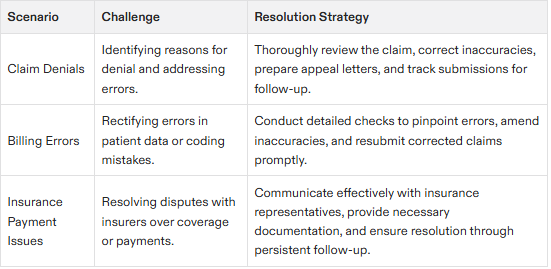
Handling a claim rejection caused by an administrative mistake often poses difficulties. Demonstrating problem-solving skills through specific examples of past experiences, such as identifying the error, implementing corrective measures, and learning from the situation, is essential to overcome such hurdles. Rectifying the error and providing the necessary supporting documents are crucial steps towards ensuring claims can be resubmitted effectively.
The significance of meticulousness and determination when tackling billing problems is underscored through this process. Cutting-edge billing strategies play a pivotal role in surmounting particular obstacles encountered during invoicing for items like medical apparatuses and services that monitor patients remotely.
How do you handle claim denials and appeals?
Dealing with claim denials requires analyzing the reasons provided for the denial, addressing any mistakes, and composing letters of appeal. It’s important to monitor appeals closely and resubmit claims promptly to reduce potential losses in revenue.
To manage claim denials successfully, it is crucial to pinpoint why a claim was denied and guarantee that the corrected claims are submitted without delay. This necessitates a systematic strategy as well as proficient communication with insurance companies.
Describe a situation where you had to correct a billing error.
Addressing billing mistakes showcases an individual’s meticulousness and dedication to quality assurance. By rectifying inaccuracies in patient data or coding mishaps, one upholds precise billing and adherence to regulations.
Recounting instances in which you pinpointed and amended errors can highlight your devotion to maintaining elevated norms within the realm of billing procedures.
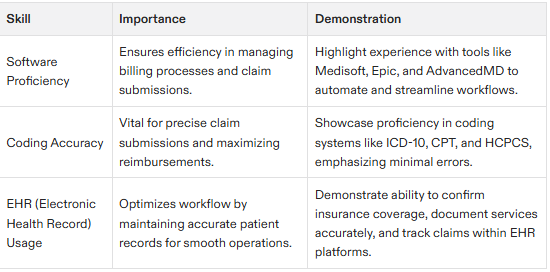
Technical Proficiency in Medical Billing
Effective medical billing hinges on technical expertise. During a medical billing interview, inquiries typically address crucial competencies such as coding knowledge, adeptness with software, and comprehension of regulatory standards. Proficiency in the use of medical billing software and electronic health records (EHR) systems is key to streamlining the accuracy and efficiency of the billing process. Accurately submitting claims using medical billing software is essential to ensure efficient payment processes and maximize reimbursement.
Below are some pivotal technical questions for consideration.
What medical billing software have you used, and how proficient are you with it?
Numerous medical billers rely on programs such as Medisoft, Epic, and AdvancedMD to streamline the billing procedures with efficiency. Mastery of these software applications is vital for optimizing workflow and maintaining precise billing operations.
Highlighting your adeptness in utilizing these systems by detailing your ability to maneuver through different modules and exhibiting your specialized knowledge reflects your technical proficiency within the field.
How do you ensure accuracy when entering patient information and codes into the system?
Attention to detail is critical in medical billing to ensure accurate coding and billing practices. Reviewing all details, using billing software, and staying updated with coding changes are effective methods to maintain accuracy.
Double-checking data, using automated tools, and staying updated with billing codes are key practices to ensure accuracy.
Can you explain the use of Electronic Health Records (EHR) in your role?
EHR systems are vital in optimizing the medical billing workflow. They assist me regularly in confirming a patient’s insurance coverage, filing claims, and monitoring their progress. Proficiency with platforms such as Epic and Medisoft is imperative to preserve precise patient documentation and facilitate the efficiency of billing procedures.
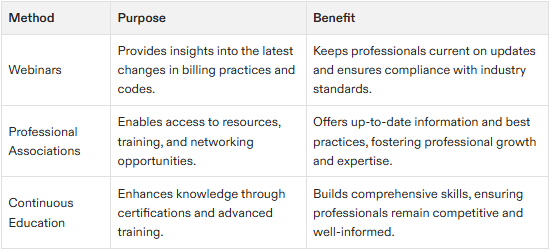
Staying Updated with Medical Billing Regulations
Keeping abreast of medical billing regulations is essential to dodge penalties and guarantee adherence. Engaging in ongoing learning via seminars, certification programs, and trade events helps maintain up-to-date knowledge on changing medical billing practices. Staying updated with regulations is also crucial for ensuring accurate submitting claims and compliance.
Here are methods to remain informed about modifications in medical billing codes and regulations.
How do you stay current with changes in medical billing codes and regulations?
It is imperative to keep abreast of the latest medical billing codes and regulations in order to adhere to compliance standards and guarantee precise billing. Engaging in webinars, attending seminars, subscribing to industry newsletters, and consulting trustworthy internet resources are valuable practices for remaining updated.
Such an endeavor necessitates a persistent commitment to staying informed about recent developments and shifts within the industry.
What professional associations or resources do you regularly participate in to enhance your knowledge?
Engaging in professional organizations and attending relevant workshops and seminars helps stay informed about the latest industry practices. Regular participation in professional associations provides valuable resources and updates on medical billing practices.
Continued skill development in medical billing is crucial to adapt to ongoing changes and improve job performance.
How do you ensure compliance with healthcare regulations in your work?
Maintaining adherence to healthcare regulations is essential for safeguarding the rights of patients and upholding the reliability of the medical system. This involves a holistic strategy that encompasses continuous education, comprehension of legal benchmarks, and interaction with expert resources.
Through engagement with professional entities, staying updated on the changing landscape of healthcare regulations can be ensured.
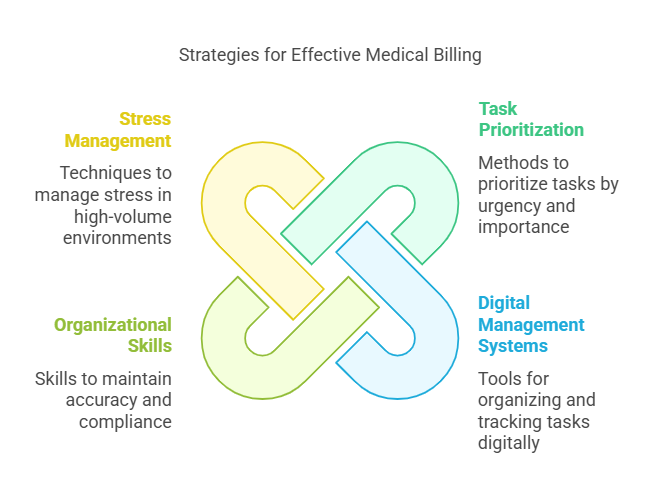
Managing Workload and Prioritizing Tasks
Effectively managing workload and prioritizing tasks are essential skills for medical billers. Prioritizing tasks by urgency and importance and using a digital task management system can enhance productivity and meet deadlines. Additionally, prioritizing tasks related to submitting claims is crucial to ensure timely payments and avoid delays.
Here are some strategies for managing workload and prioritizing tasks in medical billing.
How do you manage and prioritize your workload to meet deadlines?
A digital task management system aids in organizing tasks based on their urgency and significance. By formulating an intricate plan for each task that specifies its commencement and completion dates, focus and organization are preserved. Employing strategies such as the Eisenhower matrix along with the ABCDE Method assists in prioritizing tasks, guaranteeing that the most crucial ones are addressed first.
Can you describe a time when your organizational skills improved a process or efficiency?
Organizational skills are crucial in medical billing for maintaining accuracy, compliance, and efficiency. For example, creating a systematic filing system for patient insurance claims reduced retrieval time by 30%, significantly speeding up the billing process.
Enhancing organizational processes improves individual billing efficiency and promotes better patient satisfaction and operational effectiveness.
How do you handle stress and pressure in a high-volume billing environment?
In a high-volume billing environment, it is essential to manage stress in order to preserve accuracy and efficiency. Techniques such as practicing mindfulness, adhering to scheduled breaks, and maintaining organization can significantly diminish stress.
Creating achievable deadlines and decomposing larger assignments into smaller, more manageable pieces helps maintain steady progress while avoiding excessive pressure. Effective stress management coupled with sustained productivity contributes to an improved and gratifying billing process.
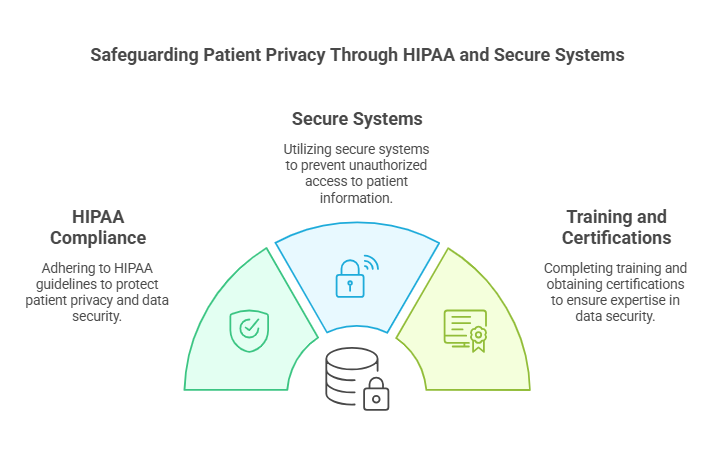
Ensuring Patient Confidentiality and Data Security
Safeguarding patient confidentiality and securing data is crucial within the realm of medical billing. Digitizing patient information through EHR systems has been instrumental in diminishing errors associated with manual data entry.
To preserve patient confidentiality and comply with data security standards, several measures are implemented.
What measures do you take to ensure patient confidentiality?
In the realm of medical billing, safeguarding patient confidentiality is a critical duty. By following HIPAA guidelines and employing secure systems while restricting access to patient information, one can effectively shield patient data. These strategies are essential for preserving confidence and upholding ethical standards in the healthcare sector.
A thorough understanding of HIPAA is crucial since it provides the framework for protecting patient data along with the consequences that arise from failing to comply. Enhancing patient confidentiality involves holding conversations in private settings and implementing strong security measures throughout all protocols.
How do you adhere to HIPAA guidelines in your daily tasks?
It is imperative to comply with HIPAA standards in the management of patient information, safeguarding against unauthorized disclosure and preserving their privacy. Routine procedures involve securely accessing systems, vigilantly preventing exposure of any patient details, and frequently reassessing adherence measures.
Adherence to HIPAA norms plays a vital role in upholding the discretion and safety of patient data within the healthcare sector. By following these guidelines, medical billing practitioners fortify patient rights and bolster professional ethical standards.
Can you discuss any training or certifications you have completed related to data security?
Engaging in training programs enables professionals to acquire essential certifications related to information security. These accreditations confirm expertise in safeguarding patient information and adherence to regulations concerning data protection.
It is imperative for professionals to remain updated on the latest best practices within the realm of information security. Emphasizing particular certifications underscores one’s dedication to maintaining stringent data security measures.
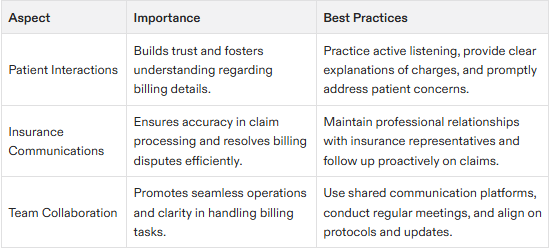
Effective Communication in Medical Billing
In the realm of medical billing, establishing clear communication is paramount as it influences both patient rapport and the precision of billing practices. By showcasing empathy and engaging in active listening with patients, one can enhance relationships and effectively address any disputes related to billing. Clear communication is also crucial when submitting claims to insurance companies and resolving any issues that arise.
Outlined below are strategies for managing disagreements with patients, interacting with insurance companies, and maintaining transparent communication among your team members.
How do you handle disputes with patients regarding their bills?
It is essential to pay close attention to the issues patients raise in order to resolve billing disputes efficiently. Make certain that all services for which charges have been levied were actually delivered and properly coded by conducting a thorough verification. Should any discrepancies be identified through this process, it’s imperative that swift measures are taken to amend them.
Providing a clear breakdown of costs enables patients to grasp the details of their bills, thus diminishing the likelihood of subsequent disagreements. Maintaining openness and forthrightness in interactions fosters trust and minimizes confusion with patients.
Can you describe your experience in communicating with insurance companies?
It is crucial to engage in a clear and concise dialogue with insurance companies to ensure that claims are processed promptly and any billing disagreements are settled efficiently. I adopt a strategy of proactive claim follow-ups while being thoroughly acquainted with the intricacies of diverse insurance policies.
Establishing professional relationships with representatives from insurance companies helps in tackling issues more effectively and cooperatively. My comprehensive background dealing with multiple insurers endows me with insight into their unique demands and operational procedures.
How do you ensure clear and effective communication within your team?
Clear communication plays a pivotal role in the realm of medical billing, as it significantly influences collaboration and the ability to work cohesively within a team. By utilizing shared platforms for communication and conducting frequent meetings among staff members, coordination is improved, leading to enhanced clarity across the board.
When addressing disputes involving patients, it’s crucial that clear communication strategies are employed to settle any concerns swiftly and preserve unity within the team. Likewise, maintaining effective lines of communication with insurance companies bolsters teamwork by guaranteeing that all members are knowledgeable about and in agreement on established billing procedures.
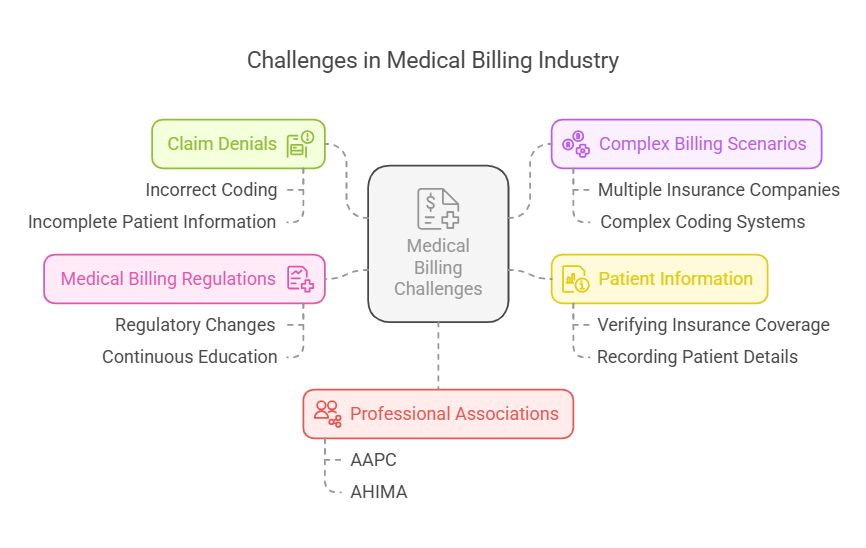
Industry-Specific Challenges
The medical billing industry is not without its challenges. Medical billers and coders face a range of issues that can impact their ability to submit accurate and timely claims. Understanding these challenges is essential for medical billers to navigate the complexities of the billing process and ensure successful claim submissions.
Common Challenges in Medical Billing
Some common challenges in medical billing include:
Claim Denials: Claim denials are a common challenge in medical billing. They can occur due to a range of reasons, including incorrect coding, incomplete patient information, or failure to meet billing regulations. Addressing claim denials requires a thorough understanding of the reasons for denial and the ability to correct and resubmit claims promptly.
Complex Billing Scenarios: Medical billing can be complex, especially when dealing with multiple insurance companies, complex coding systems, and varying billing regulations. Medical billers must be adept at navigating these complexities to ensure accurate and timely claim submissions.
Patient Information: Medical billers and coders must ensure that patient information is accurate and up-to-date to avoid errors and delays in the billing process. This includes verifying insurance coverage and ensuring that all necessary patient details are correctly recorded.
Medical Billing Regulations: The medical billing industry is heavily regulated, and billers and coders must stay up-to-date with changing regulations and guidelines to avoid errors and penalties. Continuous education and professional development are essential for staying informed about the latest billing practices and regulatory changes.
Professional Associations: Medical billers and coders can benefit from joining professional associations, such as the American Academy of Professional Coders (AAPC) or the American Health Information Management Association (AHIMA), to stay current with industry developments and best practices. These associations provide valuable resources, training, and networking opportunities that can enhance a medical biller’s knowledge and skills.
By understanding these challenges, medical billers and coders can take steps to overcome them and ensure accurate and timely submission of claims. Continuous learning and professional development are key to navigating the complexities of medical billing and achieving success in this critical field.
Career Goals and Professional Development
Embarking on a career in medical billing opens up pathways for professional advancement and niche expertise. Addressing your aspirations and dedication to continual learning showcases your resolve to progress within the domain.
We should delve into the significance of setting career objectives and perpetuating skill enhancement in the realm of medical billing.
What are your short- and long-term goals in medical billing?
In the immediate future, my focus is on enhancing my proficiency in medical billing through participation in various workshops and training sessions. These educational experiences are vital to keep abreast of new developments in billing practices and advancements within the technology used in our field.
As I look ahead, I aim to ascend into leadership positions within the realm of medical billing. My goal is to play a significant role in reforming policies and refining the overall efficacy of our billing procedures. Establishing defined career objectives serves as a roadmap for ongoing professional growth, ensuring consistent advancement.
How do you plan to continue developing your skills in this field?
I diligently keep myself updated on the latest adjustments to medical billing codes and rules by perusing sector-specific journals and participating in webinars. Engaging consistently with professional associations is a crucial source for gaining insights and information about evolving medical billing practices.
To improve my abilities, I have pursued multiple training sessions and obtained certifications centered around data protection and medical billing procedures. Ongoing education along with acquiring Qualifications are critical components of career development, ensuring proficiency is sustained within the realm of medical billing.
Why do you want to work with our healthcare provider?
I am drawn to join your healthcare provider due to your dedication to maintaining high standards and upholding ethical practices. Your values resonate with mine, and I am excited about the prospect of enhancing the efficiency of your medical billing processes.
By pursuing continuous education and professional growth in the field of medical billing, I aim to Develop my expertise. Becoming a part of your team promises avenues for advancement while enabling me to support your objective in providing outstanding healthcare services.
Frequently Asked Questions
-
A passion for healthcare and a desire to support patient care often inspire individuals to pursue a career in medical billing, as it provides stability and ongoing learning opportunities.
-
To efficiently manage claim denials, it’s crucial to thoroughly scrutinize the reasons for denial, correct any inaccuracies, draft concise appeal letters with clarity, and diligently monitor the status of each appeal to ensure prompt resubmission.
Adopting this systematic method can markedly improve the probability of achieving a favorable outcome in resolving denied claims.
-
For enhancing your billing processes, it would be advisable to look into utilizing Medisoft, Epic, or AdvancedMD as they come equipped with extensive features tailored for medical billing.
Mastering these medical billing software platforms can greatly optimize the efficiency of your operations.
-
It is crucial to keep abreast of updates and changes in medical billing codes and regulations, which can be accomplished by participating in webinars, attending seminars, and subscribing to pertinent newsletters.
Involvement with professional associations offers additional valuable resources and current information in this field.
-
For enhancing your billing processes, it would be advisable to look into utilizing Medisoft, Epic, or AdvancedMD as they come equipped with extensive features tailored for medical billing.
Mastering these medical billing software platforms can greatly optimize the efficiency of your operations.
-
I am drawn to your healthcare provider because of your commitment to high standards and ethical practices.
I am eager to contribute to your billing processes while furthering my skills through continuous education and professional development.