Top Medical Billing and Coding Programs in San Antonio
Are you searching for the best medical billing and coding programs in San Antonio? This guide provides insights into the top programs, accreditation, learning options, and career paths in this crucial field. Medical billing and coding specialists play an essential role in ensuring accurate reimbursement for healthcare providers. Whether you're looking for on-campus or online learning options, San Antonio offers various accredited programs designed to prepare you for a successful career in healthcare.
Key Takeaways for Medical Billing and Coding Success
Medical Billing and Coding Specialists: They convert medical records into standardized codes and manage billing processes to ensure healthcare providers are reimbursed accurately.
Accredited Programs in San Antonio: San Antonio offers several accredited programs with flexible learning options, including online, hybrid, and on-campus formats.
Certification: Certification in medical billing and coding, such as the CPC and CCA exams, is vital for career advancement and significantly improves job prospects.
Understanding Medical Billing and Coding
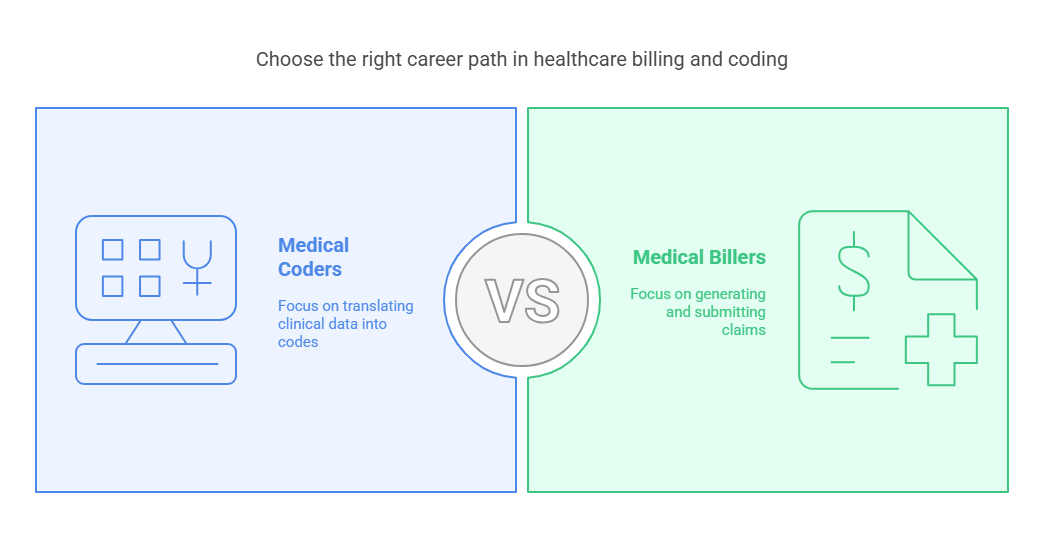
Medical billing and coding specialists ensure the proper handling of healthcare provider reimbursements by translating physician notes into standardized codes. Coders convert clinical data into codes, which are then used by medical billers to generate claims and insurance submissions. Their role ensures accuracy in billing, which is critical for the financial health of healthcare practices. As demand grows for professionals in this field, many are now looking into the Best Medical Billing and Coding Certification Programs in 2025 to gain the skills and credentials needed for success in the evolving healthcare industry.
While both roles are essential, medical coding requires a deep understanding of medical terminology, anatomy, and coding systems like ICD-10-CM and CPT. Billers, on the other hand, focus on creating and submitting claims based on the codes provided by the coders.
Educational and Training Requirements
To become a medical billing and coding specialist, completing a post-secondary program is essential. These programs typically range from a few months to two years and can be found at vocational schools, community colleges, and online institutions. Students typically earn a certificate or an associate’s degree.
Accredited programs by the American Academy of Professional Coders (AAPC) or American Health Information Management Association (AHIMA) are recommended for comprehensive education that meets industry standards.
Key Areas of Study in Medical Billing and Coding Programs
Medical Terminology and Anatomy: These are foundational to understanding the language used in healthcare and are vital for translating medical records accurately.
Coding Systems: Students learn about various coding systems like ICD-10, CPT, and HCPCS, which are used to classify diagnoses, procedures, and services.
Billing and Reimbursement Processes: Programs cover the financial aspects of healthcare, including insurance claims, and medical billing systems.
Healthcare Laws and Regulations: Knowledge of HIPAA, fraud, and compliance regulations is crucial for ensuring ethical and legal practices.
Technology in Healthcare: Training in Electronic Health Records (EHRs) and practice management software is integral to modern billing and coding tasks.
Top Medical Billing and Coding Programs in San Antonio
San Antonio offers several accredited programs designed to equip students with the skills needed for a career in medical billing and coding.
University of the Incarnate Word
Program Length: 38 weeks for on-campus or blended format; 48 weeks for online.
Certification Preparation: Includes a prep course for national certification exams.
Practical Experience: Offers externships to provide hands-on training.
Alamo Colleges
Program Length: One year for the Medical Coding and Billing Certificate.
Accreditation: Accredited by the Accrediting Bureau of Health Education Schools (ABHES).
Flexible Learning Options: Offers both online and on-campus learning options.
Southern Careers Institute (SCI)
Learning Options: Online and hybrid formats.
Career Assistance: Offers job placement services and financial aid options, including scholarships and grants.
Hands-On Training: Provides practical experience and career preparation.
Learning Options in San Antonio
San Antonio provides flexible learning options for medical billing and coding students:
On-Campus Learning: Traditional classroom settings where students engage with instructors and peers.
Online Courses: Flexibility for students to complete coursework at their own pace from anywhere.
Hybrid Programs: A combination of in-person and online learning to offer the best of both worlds.
Certification and Exam Preparation
After completing their training, students must take certification exams such as the Certified Professional Coder (CPC) or the Certified Coding Associate (CCA) exams to validate their skills. These certifications are essential for career advancement and are often required by employers.
Job Outlook and Career Opportunities
The job outlook for medical billing and coding professionals is strong, with the field projected to grow by 8% over the next decade. Demand for certified professionals is increasing as healthcare providers rely on accurate billing for proper reimbursement.
Average Salary in San Antonio:
Medical billing and coding specialists earn approximately $45,000 annually, with opportunities for salary increases as they gain experience and additional certifications.
Potential Employers:
Hospitals, private practices, insurance companies, and government agencies are all major employers in the medical billing and coding industry.
6 Lesser-Known Facts About Medical Billing and Coding
Growing Need Due to Aging Population:
Diverse Career Paths:
Work-from-Home Opportunities:
Technological Advancements in Coding:
Specializations in Coding:
Job Security:
FAQs About Medical Billing and Coding in San Antonio
-
The top programs in San Antonio include the University of the Incarnate Word, Alamo Colleges, and Southern Careers Institute, all offering accredited courses with flexible learning options.
-
Programs typically take anywhere from 9 months to 2 years, depending on whether you choose a certificate program or an associate’s degree.
-
The average salary for medical billing and coding specialists in San Antonio is approximately $45,000 per year. This can vary based on experience, certifications, and the employer.
-
The Certified Professional Coder (CPC) and Certified Coding Associate (CCA) certifications are highly recommended and may be required by employers.
-
Yes, students can apply for federal financial aid, including Pell Grants, scholarships, and other state or institutional grants and loans to help cover tuition costs.
Conclusion
Embarking on a career in medical billing and coding in San Antonio offers a rewarding path with opportunities for career growth and financial stability. With various accredited programs available, including options like AMBCI for medical billing and coding certification, students can benefit from flexible learning formats and industry-recognized credentials. Given the growing demand for skilled professionals, now is an excellent time to start your journey. Explore the programs that best fit your goals and take the next step towards a successful career in the healthcare industry.