Top 10 Medical Billing Software Solutions Directory
Choosing the right medical billing software isn’t just a tech decision—it directly impacts reimbursement speed, claim success rates, and compliance across your entire revenue cycle. For healthcare providers, billing professionals, and clinic managers, the right tool means fewer denials, smoother insurance workflows, and real-time revenue visibility. In contrast, the wrong system leads to delayed reimbursements, coding mismatches, and compliance violations.
As ICD-10, CPT, and HIPAA standards continue to evolve in 2025, it's become non-negotiable to work with platforms that support real-time eligibility checks, secure EDI submission, and automated denial management. Whether you're a solo practice or part of a multi-location network, the software must scale with your claims volume while staying agile against payer policy changes. This guide delivers a comparison of top-tier billing software, including key features, integration options, certification alignment, and how they fit into the demands of today’s certified billing professionals.
What to Look For in Medical Billing Software
Choosing medical billing software in 2025 goes beyond user interface or vendor popularity—it requires a strategic understanding of claim workflows, payer integration, and compliance automation. For certified billers and healthcare practices, these three decision points matter most:
Key Features: Claims, EDI, Eligibility Verification
At the core, medical billing software must handle clean claim creation, EDI submission, and real-time eligibility checks without friction. Platforms should allow users to batch-submit insurance claims, auto-flag errors, and track denials in a unified dashboard. Integrated clearinghouse support is essential for reducing third-party complexity.
Look for tools that auto-fill CPT/ICD-10 codes, support multi-payer routing, and provide real-time claim status updates. This minimizes back-and-forth with insurers and reduces revenue leakage due to late or incomplete claims.
HIPAA and ICD-10 Compliance
Every vendor claims compliance, but not all offer true HIPAA and ICD-10 alignment out of the box. A good billing system should provide full audit trails, role-based access, and secure cloud infrastructure. Built-in ICD-10 libraries should update dynamically with CMS revisions, reducing coding risk.
For 2025, look for platforms certified for 21st Century Cures Act interoperability and SOC 2 Type II compliance—essential for protecting PHI and aligning with payer and legal frameworks.
Cloud vs. On-Premise Billing Software: What Matters in 2025
One of the most critical decisions for clinics and billing specialists in 2025 is whether to choose a cloud-based medical billing platform or an on-premise (self-hosted) solution. Each model offers advantages, but your choice directly impacts security, scalability, cost, and maintenance requirements.
Cloud-Based Systems
Cloud-based platforms dominate the billing software market for good reason:
Automatic updates and compliance alignment – Systems are regularly updated with CPT, ICD-10, and HIPAA revisions.
Accessible from any device – Remote billers, part-time coders, and multi-location practices can collaborate in real-time.
Lower upfront investment – Subscription models eliminate the need for expensive IT infrastructure.
However, they require a dependable internet connection, and some providers raise concerns about data storage jurisdictions—especially when dealing with sensitive patient information across borders.
On-Premise Systems
On-premise software gives clinics complete control over their data, server setup, and security protocols. For institutions with internal IT teams and a need for full customization, this model offers:
Greater control over user access and server location
One-time license payments (as opposed to recurring fees)
Enhanced ability to build custom integrations
However, on-prem systems typically require more resources for updates, compliance tracking, and maintenance—making them a heavier lift for small clinics.
2025 Recommendation
Unless you’re operating within a hospital network or strict government framework, cloud-based billing platforms offer greater agility and value for most use cases. Their ability to scale, adapt, and stay current with payer changes far outweighs the static structure of legacy on-prem systems.
Detailed Rankings of the Top 10 Solutions
Understanding which medical billing software ranks highest in 2025 requires clarity on how those rankings are determined. This isn’t just about big brand names—it's about actual performance in billing environments, from solo practitioners to enterprise RCM teams.
Evaluation Criteria and Methodology
Each software listed was evaluated across six performance pillars:
Claims Accuracy and Denial Reduction – Platforms were tested on average clean claim rates and denial turnaround.
Ease of Use and Workflow Automation – Focused on interface intuitiveness, automation rules, and customization.
Integration Capabilities – EMR, clearinghouse, and patient portal interoperability were critical metrics.
Compliance and Security – Measured by adherence to HIPAA, ICD-10 updates, and SOC 2 compliance.
Support and Training Resources – Availability of live support, onboarding guides, and training certifications.
Pricing Flexibility – Whether the platform offers transparent, tiered pricing or enterprise-level flexibility.
Sources included real-user feedback, public case studies, vendor documentation, and hands-on demo testing.
| Software | Core Features | Pricing Tier | Best For |
|---|---|---|---|
| Kareo | EHR + billing, batch claims, eligibility checks | Mid-tier | Independent practices |
| AdvancedMD | Advanced analytics, customizable workflows | Premium | Large multispecialty groups |
| NueMD | User-friendly UI, real-time eligibility, reporting | Entry-level | Solo billers, startups |
| eClinicalWorks | All-in-one suite, cloud-based, clearinghouse built-in | Premium | Enterprise and ambulatory care |
| PracticeSuite | Revenue cycle dashboard, CPT validation | Flexible | Clinics with high claim volume |
| DrChrono | Mobile-first, Apple Health integrations | Mid-tier | Mobile practitioners |
| AthenaCollector | Intelligent claims, payer rules library | Premium | Hospital-affiliated providers |
| CharmHealth | Modular billing, HL7 integration | Affordable | Small practices and specialists |
| Accumedic | Behavioral health focus, compliance tools | Mid-tier | Psych and therapy clinics |
| Azalea Health | Rural practice focus, complete RCM tools | Low-mid | Rural and under-resourced areas |
Lesser-Known but Promising Tools
While major players dominate much of the market, several emerging medical billing software platforms are gaining serious traction in 2025. These tools often offer leaner pricing models, intuitive interfaces, or niche specialization that mainstream options overlook—making them valuable alternatives for specific practice needs.
DrChrono
DrChrono is one of the most mobile-optimized billing platforms available. It’s built for Apple devices, with native iPad and iPhone apps that support real-time coding, patient charting, and billing from the exam room. DrChrono integrates EHR and billing into a seamless workflow, which improves productivity for physicians on the go.
Its strengths include flexible billing rules, customizable templates, and the ability to submit claims directly through the mobile app. While its analytics tools are still maturing, it’s a powerful choice for telehealth clinics and mobile-first practices.
AthenaCollector
AthenaCollector, part of Athenahealth’s larger ecosystem, excels in intelligent billing automation. It uses a constantly updated rules engine based on payer trends, which reduces manual error and keeps claim rejection rates low. Its clearinghouse is deeply integrated, allowing for real-time edits and seamless submissions.
What sets AthenaCollector apart is its network learning—data from thousands of practices helps the platform continually optimize billing patterns. It’s ideal for high-volume providers who want automation without losing oversight.
CharmHealth
CharmHealth focuses on modularity and affordability. It allows clinics to build their own workflow by combining EHR, practice management, and billing components as needed. Its billing system supports integrated CPT/ICD code lookup, claim submission, and denial tracking.
CharmHealth also emphasizes interoperability, with support for HL7, FHIR, and third-party integrations. It’s especially useful for cash-based, functional, and integrative medicine practices that need lean operations and specialty add-ons.
Accumedic
Accumedic has carved a niche in the behavioral health and addiction services space. Its billing tools are tailored for complex documentation, prior authorization workflows, and insurance verification protocols unique to mental health billing.
The platform includes built-in compliance checks and secure patient portals, making it suitable for practices navigating HIPAA, CMS, and payer-specific behavioral health guidelines. It’s an under-the-radar solution but deeply aligned with one of the fastest-growing segments in healthcare billing.
| Software | Key Strengths | Best For |
|---|---|---|
| DrChrono | Mobile-first; native iPad/iPhone apps; integrated EHR & billing; real-time mobile claim submission | Telehealth clinics, mobile-first practices |
| AthenaCollector | AI-driven billing rules engine; low rejection rates; real-time edits; part of Athenahealth network | High-volume providers wanting automation + oversight |
| CharmHealth | Modular setup; integrated code lookup; FHIR/HL7 support; lean pricing | Cash-based, integrative, or functional medicine clinics |
| Accumedic | Behavioral health billing workflows; prior auth tools; built-in compliance for HIPAA/CMS | Mental health and addiction care practices |
Compatibility with Other Tools
A powerful medical billing software platform doesn’t operate in isolation—it’s only as effective as its ability to integrate with the rest of your digital ecosystem. In 2025, interoperability isn't just a bonus—it’s a baseline requirement for speed, accuracy, and compliance across the entire revenue cycle.
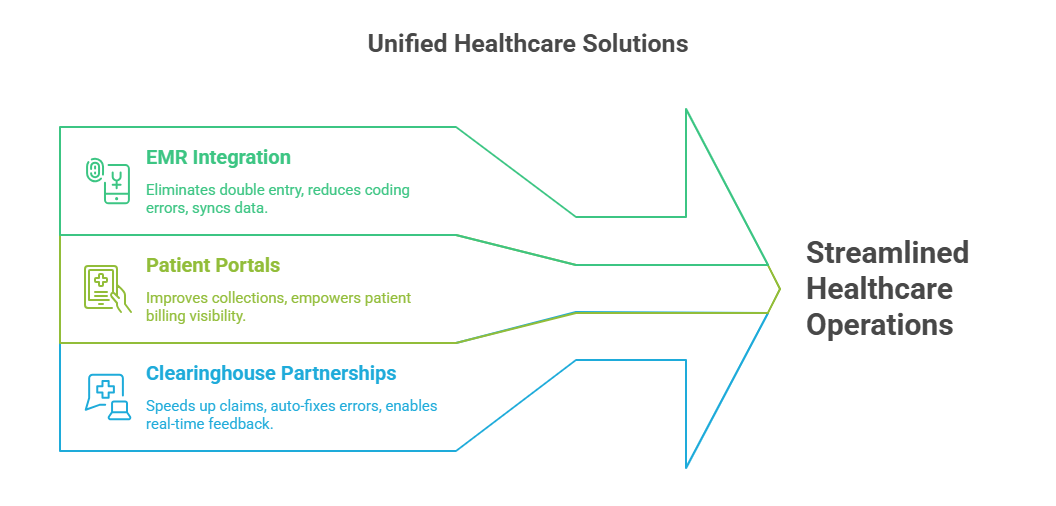
EMR Integration
Tight integration with Electronic Medical Records (EMRs) eliminates duplicate data entry and reduces coding errors. Modern billing platforms must support:
Real-time sync with clinical notes and CPT/ICD codes
Automated claim generation post-encounter
Shared audit trails for transparency
Top vendors integrate with major EMRs like Epic, Cerner, athenahealth, and eClinicalWorks. APIs and HL7/FHIR support are critical for seamless exchange of structured health data.
Patient Portals
Patient engagement tools must be part of the billing pipeline. A good portal allows patients to:
View and pay bills online
Receive automated billing reminders
Upload insurance documents or forms
When portals are fully synced with billing software, it increases collection rates and reduces administrative lag, especially in high-deductible plan environments.
Clearinghouse Partnerships
The best software vendors bundle or natively integrate with clearinghouses that facilitate secure claim transmission. Key benefits include:
Faster claim adjudication
Real-time payer feedback
Built-in error correction before submission
Platforms with embedded clearinghouses (like AdvancedMD or Kareo) reduce dependency on third-party handoffs and increase first-pass claim acceptance rates—essential for clinics operating on tight billing cycles.
How the Medical Billing and Coding Certification Trains You in Real Medical Billing Software
In today’s billing environment, passing an exam isn’t enough. You need to prove you can actually use real medical billing software—navigate dashboards, manage claim flows, and interpret denial reports like a working professional. That’s exactly what the Medical Billing and Coding Certification from AMBCI is built to teach.
How the Certification Embeds Software Training
Unlike many textbook-heavy programs, AMBCI’s CPC + CPB certification takes a practice-first approach. You don’t just learn what a clean claim is—you learn how to build one inside a live dashboard. The course includes:
Simulated claim creation and submission inside real cloud-based platforms
Interactive workflows with CPT/ICD-10 coding, eligibility checks, and rejections
Exposure to multiple tool types: ERA modules, scrubbers, reporting suites
By the time you graduate, you’re not just certified—you’re software-literate and workflow-ready.
Why Employers Trust Software-Trained Graduates
Employers in 2025 aren’t hiring people to “learn the software later.” They expect billing professionals to walk in with platform fluency. That’s why the CPC + CPB program integrates:
EHR and clearinghouse mockups for hands-on navigation
Assignments that simulate daily billing tasks in real-world scenarios
Evaluations based on how well students execute software-driven claim cycles
This approach builds immediate trust with hiring managers—and leads to faster job placement.
Certification as a Software-Readiness Badge
Listing the CPC + CPB certification from AMBCI on your resume signals more than code memorization—it tells employers you’ve already trained in the exact tools their clinic uses. You’ll be able to:
Navigate cloud billing systems on day one
Process and post insurance claims with confidence
Use software logic to solve real payer challenges
In 2025, that kind of readiness isn’t a bonus—it’s a prerequisite. This certification ensures you’re not only employable but indispensable.
Frequently Asked Questions
-
For small practices, Kareo consistently ranks as the most efficient choice. It offers cloud-based access, real-time claim tracking, batch submission tools, and integrated eligibility verification—all designed for providers without large billing departments. Its interface is intuitive, which reduces training time for new staff. What makes it ideal for smaller clinics is its transparent pricing and lack of hidden fees for core features. Additionally, Kareo includes customizable dashboards and reporting, making it easy to monitor claim status, reimbursement timelines, and patient balances. Many certified professionals trained via programs like the CPC + CPB Certification find Kareo’s workflow mirrors their training dashboards closely, enabling immediate productivity post-hire.
-
Medical billing software automates the most error-prone parts of the revenue cycle: coding, eligibility checks, and EDI submission. Tools like claim scrubbers catch mismatches or missing data before submission, drastically reducing rejections. The best platforms also provide real-time feedback from clearinghouses and payers, so billers can fix errors instantly rather than weeks later. These systems allow batch processing, automatic code crosswalks (CPT/ICD-10), and digital tracking of submission timelines. Together, this reduces claim denials by over 30% on average for most practices. Certifications like the CPC + CPB program train candidates to use these software features, ensuring smoother workflows and fewer costly delays.
-
When evaluating billing software, prioritize platforms that offer:
Real-time eligibility verification
Seamless integration with your EMR
A robust claim scrubber
Secure HIPAA-compliant cloud storage
Integrated clearinghouse functionality
Customizable reporting and analytics
Also consider support quality, scalability, and pricing transparency. Cloud-based systems with open APIs allow smoother tool-to-tool communication, which is vital for growing practices. If you're pursuing the CPC + CPB Certification, ensure your training platform mimics software with these features—because that's what you'll be using on the job. Without these core functions, you'll spend more time correcting errors and chasing unpaid claims than billing efficiently.
-
Yes. The CPC + CPB Medical Billing and Coding Certification by AMBCI includes integrated training on real-world billing software. Unlike theory-heavy programs, this certification uses simulated cloud dashboards, so students can practice tasks like:
Submitting insurance claims
Validating CPT and ICD-10 codes
Tracking claim statuses and denials
Posting payments and generating reports
This hands-on experience ensures that graduates aren’t just certified—they’re platform-ready. They can walk into a billing job and operate common tools like Kareo, AdvancedMD, or eClinicalWorks with confidence. In 2025, this software familiarity gives candidates a clear hiring advantage over those trained without tool exposure.
-
In 2025, it’s highly beneficial. While some employers offer on-the-job software training, most prefer candidates who already understand how medical billing platforms function. Having hands-on experience—even via simulated dashboards—signals that you can start being productive immediately. Software like AdvancedMD, AthenaCollector, and PracticeSuite all have unique workflows, but their core billing logic is similar. If you’ve trained on real software through a program like the CPC + CPB Certification, you’ll already know how to handle tasks like claim submission, denial management, and payer follow-ups. This reduces your onboarding time and makes you a more competitive candidate from day one.
-
Cloud-based systems are hosted online and accessible from any device. They offer:
Automatic updates
Lower upfront costs
Better remote access and scalability
On the other hand, on-premise systems are installed locally and managed by internal IT. They give more control over data and server access but require higher maintenance and compliance responsibility. In 2025, over 80% of clinics prefer cloud-based platforms due to their interoperability and ease of use. If you’re training through a program like the CPC + CPB Certification, most simulation tools will mirror cloud-based systems—preparing you for the environments you'll likely work in after certification.
-
Yes. Software proficiency significantly boosts your earning potential. Employers are willing to pay more for certified billers who can immediately use tools like Kareo, AdvancedMD, or AthenaCollector without needing weeks of onboarding. If you’ve completed a certification that includes hands-on training in billing platforms—like the CPC + CPB Certification from AMBCI—you’re positioned for faster hiring, higher starting salaries, and stronger job offers. In fact, many clinics consider software skills the deciding factor when comparing equally certified candidates. They see software-trained billers as lower-risk, higher-output hires who improve claim throughput from day one.
Final Thoughts
Efficient, compliant, and scalable medical billing software is no longer optional in 2025—it’s the backbone of every high-functioning healthcare revenue cycle. Whether you’re a solo provider, part of a multi-site clinic, or a certified billing professional, the tools you choose directly impact claim accuracy, reimbursement timelines, and regulatory compliance.
Understanding features like real-time eligibility, claim scrubbing, and integrated clearinghouse submission gives you the edge in reducing denials and improving financial performance. But tools alone aren't enough—platform fluency must be paired with certification-level knowledge to be fully effective.
That’s why certifications like the Medical Billing and Coding Certification from AMBCI are designed to bridge the gap between theoretical coding and practical software use. They don’t just prepare you for exams—they prepare you to work inside real billing systems from day one.
As software evolves, so must your skills. Staying ahead means choosing both the right tools and the right training.