Understanding Quality Assurance in Medical Coding
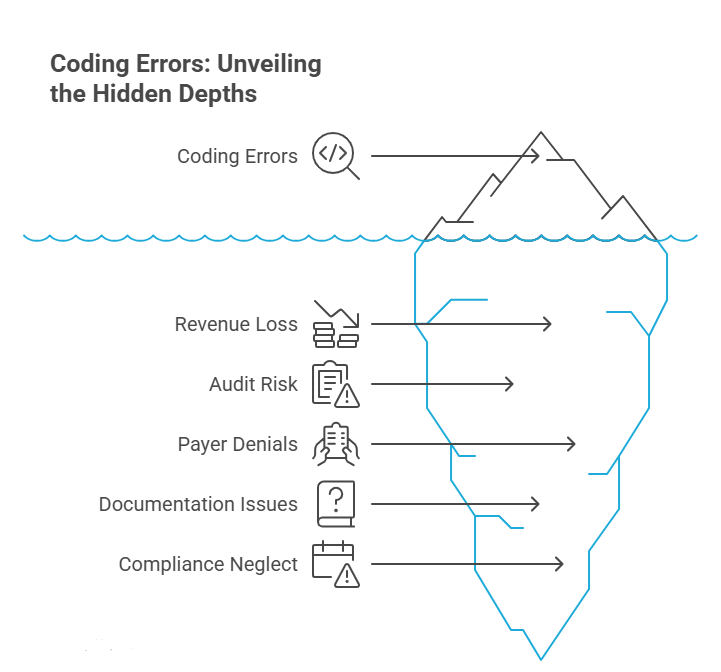
Medical coding accuracy isn’t just about CPT or ICD-10 lookup—it’s about maintaining compliance, safeguarding revenue, and avoiding audit flags. As healthcare organizations face rising scrutiny from CMS, OIG, and commercial payers, quality assurance in medical coding has evolved from a nice-to-have into a compliance-critical function. Every missed modifier, upcoded procedure, or vague clinical note creates costly downstream issues—from claim denials to overpayment investigations.
Quality assurance (QA) frameworks in coding help teams identify errors before payers do, resolve documentation gaps, and align with federal billing guidelines. QA doesn’t just prevent mistakes—it improves coder performance, drives reimbursement accuracy, and ensures audit readiness across inpatient and outpatient settings. With the complexity of today’s value-based care models, mastering QA has become essential for coders who want to move beyond data entry into roles that impact compliance, revenue integrity, and institutional trust.
What Is Quality Assurance in Medical Coding?
The Concept of QA in Medical Documentation
Quality assurance in medical coding is the systematic review of coded data to ensure accuracy, compliance, and integrity across patient records. It’s not a post-mistake fix—it’s a preemptive strategy woven into every phase of the medical documentation and coding lifecycle. QA involves verifying that each diagnosis (ICD-10), procedure (CPT/HCPCS), and modifier has been correctly applied based on the provider’s clinical narrative, ensuring documentation supports every coded entry.
At its core, QA acts as a bridge between clinical language and billing compliance. Reviewers audit whether coders have interpreted clinical documentation in accordance with CMS guidelines and payer-specific rules. This includes evaluating whether the medical necessity is clear, codes are specific, and nothing has been over- or under-coded. As coding rules evolve quarterly, QA ensures coders remain aligned with the most current updates—protecting organizations from denials, recoupments, or False Claims Act exposure.
How QA Differs from Quality Control in Coding
Although often used interchangeably, quality assurance and quality control serve distinct roles in the coding environment. Quality assurance is proactive—it’s a continuous monitoring system built to prevent errors before they occur. It includes coder education, real-time audits, documentation feedback loops, and policy refinement. QA sets the standard, then reinforces it.
Quality control (QC), by contrast, is reactive. It identifies and fixes errors after submission or during retrospective audits. QC flags issues, but QA prevents them. For instance, a QC activity might catch repeated modifier 25 misuse; a QA program would identify the root cause, update SOPs, and retrain staff before more claims are affected. In modern RCM operations, QA is the strategic layer that sustains compliance, audit readiness, and reimbursement accuracy, while QC acts as the safety net for operational leakage. Both are essential, but QA is the backbone of scalable, compliant coding practices.
Why QA Matters: Real Impact on Compliance and Revenue
Compliance with CMS, OIG, and HIPAA Standards
Medical coding QA directly impacts compliance with CMS billing rules, OIG audit frameworks, and HIPAA privacy mandates. Every coding decision ties into federal regulations, and QA ensures those decisions align with current law. The Office of Inspector General routinely investigates improper payments triggered by coding inaccuracies—especially overuse of high-level E/M codes, duplicate billing, or unsupported diagnoses.
QA teams enforce internal checks that mirror external payer audits. They verify whether documentation justifies code selection, whether modifiers meet policy requirements, and whether encounter notes are complete and compliant. Without QA, providers risk violating HIPAA minimum necessary standards, particularly when sensitive codes (like behavioral health or HIV status) are misused or miscoded. QA also strengthens compliance by reinforcing coder accountability and providing corrective action pathways to address repeat errors. In short, it's a frontline defense against fines, repayment demands, and federal investigations.
Revenue Cycle Efficiency and Denial Reduction
Coding QA isn’t just a compliance safeguard—it’s a revenue accelerator. When coders apply inaccurate CPT, ICD-10, or HCPCS codes, claims are denied, delayed, or underpaid. QA helps identify denial trends before they scale. By reviewing patterns—like improper use of modifier 59, overuse of unspecified diagnosis codes, or mismatches between CPT and ICD-10—QA teams can implement corrections across entire service lines.
This has tangible financial impact. Facilities with structured QA programs report up to 35% fewer claim rejections and a 20–25% increase in clean claim rates. Coders who receive QA-driven feedback submit more accurate claims the first time, reducing AR days and improving cash flow. QA also minimizes payer disputes by ensuring documentation supports code selection, which is critical in high-dollar procedures and risk-adjusted coding. The result: fewer denials, faster payments, and better payer relationships—driven by compliance-informed coding.
QA Workflow: How It’s Implemented in Medical Coding Operations
Step-by-Step QA Process Flow
A well-structured QA process in medical coding follows a defined, cyclical flow that ensures continuous improvement. It begins at the coding stage but integrates seamlessly into the revenue cycle management (RCM) pipeline.
Code Selection Review
QA auditors begin by selecting a randomized or risk-based sample of coded encounters. These may be inpatient charts, surgical cases, or outpatient visits based on audit goals.Documentation Validation
Each code is matched against the clinical documentation to verify medical necessity, specificity, and modifier accuracy. This step ensures that provider intent aligns with code output.Error Categorization
Errors are categorized (e.g., under-coding, unbundling, upcoding), and severity is assessed. Patterns are flagged for systemic review.Feedback to Coders
QA teams provide coders with annotated reports or one-on-one feedback to correct logic errors, documentation misinterpretations, or payer-specific policy violations.Corrective Action Planning
When error rates exceed thresholds, QA leads coordinate retraining, update internal coding guidelines, or escalate for process revision.Re-Auditing and Monitoring
QA isn’t a one-time fix. Re-audits track coder improvement and monitor compliance with updated regulatory guidance and internal SOPs.
This process ensures that errors are caught early, feedback is tracked, and compliance risk is reduced over time.
Tools and Technologies Used in QA Review
QA in coding has moved beyond spreadsheets and manual logs. Today’s teams use audit software platforms that integrate with EHRs, coding dashboards, and billing systems. Key tools include:
3M™ CodeFinder & EncoderPro: Used to validate code combinations and catch unbundling or sequencing errors.
AI-assisted audit platforms: Flag discrepancies between provider notes and coded data using natural language processing.
Internal QA dashboards: Monitor coder error rates, feedback history, and compliance trend lines across departments.
These tools enable QA reviewers to detect errors at scale, track coder performance, and provide data-driven feedback that reinforces accuracy and regulatory alignment.
| QA Step | Purpose in Workflow |
|---|---|
| Code Selection Review | Selects random or targeted coded encounters for review based on risk or volume |
| Documentation Validation | Ensures codes match clinical notes, modifiers are accurate, and medical necessity is met |
| Error Categorization | Labels errors (under-coding, unbundling, etc.) and flags trends for systemic action |
| Feedback to Coders | Provides annotated reports or meetings to explain logic, policy violations, or errors |
| Corrective Action Planning | Triggers retraining, SOP updates, or escalations when error thresholds are exceeded |
| Re-Auditing and Monitoring | Measures improvement, tracks progress, and ensures sustained compliance |
Common QA Errors Found in ICD-10/CPT Coding Audits
Under-coding, Over-coding, and Modifier Misuse
The most frequent QA issues in coding audits stem from under-coding, over-coding, and modifier misuse—each of which compromises both compliance and reimbursement accuracy.
Under-coding occurs when coders fail to report all billable services or select codes of lower complexity than warranted. This leads to lost revenue, inaccurate patient risk stratification, and diminished case mix index.
Over-coding involves reporting more complex or additional codes than supported by documentation. This is a major red flag for payers and can trigger fraud investigations under the False Claims Act.
Modifier misuse—such as applying modifier 25 or 59 inappropriately—can distort procedure bundling and misrepresent services as separately billable. It’s one of the top causes of commercial payer denials and post-payment audits.
QA teams must understand not only the CPT/HCPCS codebook but also payer-specific bundling rules and NCCI edits to accurately assess these risks.
Lack of Clinical Justification and Missed Guidelines
Even with correct code selection, many audits reveal that documentation lacks sufficient clinical justification. This includes:
Vague or copy-pasted diagnosis descriptions
Missing time elements for E/M level selection
No rationale for the use of high-complexity modifiers
Equally common are missed guideline updates—especially when quarterly CPT or ICD-10 changes are not reflected in internal coding practices. QA serves to close these gaps by retraining coders and flagging provider documentation issues that require clarification or revision.
Roles and Responsibilities of QA Specialists in Coding Teams
Required Skills and Daily Activities
QA specialists in medical coding are not just seasoned coders—they are compliance strategists with deep knowledge of regulatory frameworks, coding guidelines, and payer behavior. Their day-to-day responsibilities go far beyond reviewing codes; they conduct clinical documentation audits, identify training gaps, and standardize feedback for both coders and providers.
Core skills include:
ICD-10-CM, CPT, and HCPCS mastery
Familiarity with NCCI edits, CMS guidelines, and payer-specific protocols
Ability to identify patterns in denials, coding variance, and documentation gaps
Daily, they audit selected claims, meet with coding teams to review findings, provide annotated reports, and lead internal QA calibration sessions. They also stay updated with quarterly code updates, assess coder proficiency metrics, and generate QA dashboards that help leadership make informed RCM decisions. In short, they optimize coding integrity at scale—not just by fixing errors, but by building systems that prevent them.
Collaboration with Medical Coders and Billing Staff
QA specialists don’t operate in silos—they are embedded in the coding, billing, and compliance ecosystem. Their value multiplies when they actively collaborate with coders, billers, and physicians. During coder onboarding, QA leads play a central role in setting accuracy benchmarks and compliance expectations. When issues arise, they provide focused retraining rather than blanket feedback.
With billing teams, QA specialists help validate that coding matches reimbursement criteria, especially for high-dollar claims or specialty services. When denials occur, they assist in root-cause analysis—was it coding, billing, or documentation? Their insights reduce rework, improve first-pass acceptance rates, and enhance interdepartmental trust. Through structured workflows and open communication, QA teams ensure that every stakeholder contributes to coding compliance and revenue protection.
How to Build a Career in Coding QA
Required Background and Training Pathways
Becoming a QA specialist in medical coding requires more than just coding credentials—it demands clinical insight, regulatory fluency, and analytical rigor. Most QA professionals begin as certified coders with 2–5 years of experience across inpatient, outpatient, or specialty settings. During this time, they develop a sharp eye for coding logic, payer guidelines, and documentation gaps.
Key foundational credentials include:
CPC (Certified Professional Coder)
CPB (Certified Professional Biller)
CCS or CCS-P (Certified Coding Specialist)
To transition into QA, coders must deepen their expertise in audit protocols, NCCI edit logic, and payer policy updates. Training in data analysis, EHR audit tools, and documentation improvement is equally important. Strong candidates also pursue training in compliance workflows and denial management, giving them a cross-functional lens that spans clinical operations and revenue cycle.
Medical Billing and Coding Certification by AMBCI.
For coders aiming to lead in QA, the most comprehensive path combines coding certification with advanced audit and billing proficiency. The best way to gain this edge is by enrolling in high-level dual training programs that teach both CPT/ICD-10 coding and billing strategy.
One of the most effective programs currently available is the
Advanced CPC + CPB Medical Billing and Coding Certification by AMBCI.
This certification goes beyond code sets to cover revenue cycle mechanics, denial prevention, audit readiness, and QA workflows. Graduates gain:
Expertise in coding accuracy and billing integration
Tools to navigate payer disputes and compliance pitfalls
A credential that aligns with real-world QA job functions
Whether your goal is to move into audit leadership or become a QA lead for a multi-specialty practice, this course offers the deep training and regulatory alignment required for today’s coding QA demands.
Frequently Asked Questions
-
A QA specialist in medical coding reviews coded records to ensure accuracy, compliance, and adherence to regulatory guidelines. They verify that CPT, ICD-10, and HCPCS codes reflect the documented medical services and align with payer rules. Their role includes auditing coded charts, identifying patterns of error, and providing targeted coder feedback. QA specialists also monitor denial trends, suggest process improvements, and update coding protocols to meet changing CMS or insurer policies. Their goal is to prevent revenue loss, ensure regulatory compliance, and enhance coder performance. In many healthcare settings, they also lead training sessions and contribute to internal policy refinement—making them critical to risk mitigation and billing accuracy.
-
Internal quality assurance is a proactive, routine process designed to maintain coding accuracy over time, whereas external audits are retrospective reviews conducted by payers or regulators to verify claim validity. QA focuses on early error detection, coder education, and process improvement before claims are submitted. External audits, such as those from the OIG or RAC, happen after submission and often involve penalties for noncompliance. While both identify coding discrepancies, QA allows healthcare organizations to address issues internally, reducing audit exposure. Building a strong QA program can significantly minimize the frequency and severity of external audit findings and related financial penalties.
-
The most common QA coding errors include under-coding, over-coding, and modifier misuse. Under-coding leads to lost revenue, while over-coding may raise red flags for fraud investigations. Modifier misuse—especially of modifiers 25, 59, and 51—is a frequent source of payer denials. Additional errors involve selecting outdated codes, lack of medical necessity, and misalignment between documentation and selected codes. QA audits also catch coding that doesn’t follow National Correct Coding Initiative (NCCI) edits or payer-specific policies. Identifying these issues early ensures clean claim submission and reduces denial rates across both outpatient and inpatient claims.
-
The frequency of QA reviews depends on coding volume, specialty, and risk level, but monthly or bi-weekly audits are standard in most healthcare settings. High-volume coders or new team members may undergo more frequent QA checks, while experienced coders may follow random sampling protocols. In high-risk specialties such as cardiology or neurosurgery, weekly audits are often recommended. Some organizations use rolling audits—targeting a small percentage of claims continuously to catch issues in real time. Consistent QA frequency helps coders stay aligned with updated guidelines, reduce recurring errors, and maintain payer trust by ensuring audit readiness.
-
Yes, a well-structured QA program significantly reduces claim denials by identifying and correcting coding issues before claims are submitted. QA teams review for documentation gaps, improper use of modifiers, and non-compliant code selection. They also flag mismatches between diagnosis and procedure codes, which are common reasons for claim rejections. By analyzing patterns—like frequent denials tied to a specific CPT code—QA specialists help coders adjust practices proactively. Facilities that implement real-time QA feedback loops report up to 35% fewer denials and faster reimbursement cycles. Ultimately, QA helps coders submit claims that are payer-ready on the first attempt.
-
The best credentials for QA coding specialists include CPC (Certified Professional Coder), CPB (Certified Professional Biller), and CCS/CCS-P from recognized bodies like AAPC or AHIMA. However, QA roles often require more than certification—they demand real-world coding experience, regulatory knowledge, and analytical skills. Professionals aiming for QA roles should also pursue advanced certifications or dual credentials that cover both billing and compliance. Programs like the Advanced CPC + CPB Medical Billing and Coding Certification by AMBCI provide deep training in audit workflows, denial analysis, and payer communication—key competencies for success in QA leadership roles.
-
Quality assurance offers coders a path to higher-level roles by deepening their understanding of regulatory standards, documentation quality, and revenue cycle strategy. Coders involved in QA develop critical thinking skills, learn to analyze patterns, and gain exposure to payer expectations. These competencies position them for roles in audit, compliance, and coding leadership. Many QA specialists eventually become coding educators, compliance officers, or revenue integrity analysts. Participating in QA reviews also improves individual coder performance, as real-time feedback helps eliminate recurring mistakes and encourages ongoing professional development. QA isn’t just oversight—it’s a fast track to senior roles.
-
Software plays a pivotal role in modern QA by automating audit processes, tracking coder performance, and flagging high-risk claims. Tools like 3M™ CodeFinder, TruCode, and AI-driven QA platforms use NLP (Natural Language Processing) to detect inconsistencies between documentation and codes. These platforms also monitor denial trends, highlight coding variance, and produce dashboards for compliance tracking. By integrating with EHR and billing systems, QA software ensures audits are faster, more consistent, and scalable across departments. For organizations dealing with high volumes or multi-specialty coding, software is essential for sustaining accuracy, reducing manual workload, and improving QA response time.
Final Thoughts
In today’s regulatory landscape, mastering quality assurance in medical coding is not a luxury—it’s a competitive necessity. Healthcare organizations are under constant pressure to demonstrate compliance, minimize denials, and maintain accurate reimbursement. Coders who understand QA workflows, coding audit protocols, and payer expectations bring immense value to their teams and employers.
Whether you're just entering the field or advancing into audit leadership, investing in QA knowledge prepares you to be audit-proof, future-ready, and strategically indispensable. It’s more than catching mistakes—it’s about preventing them, improving processes, and protecting revenue integrity at scale. In an era where value-based care models demand transparency and precision, QA-trained coders are the professionals that healthcare organizations trust to get it right the first time—every code, every claim, every chart.