Understanding What is an Encounter in Medical Billing: A Simple Guide
In medical billing, a patient encounter is defined as any interaction between a patient and a healthcare provider where medical services are rendered. This could include office visits, surgeries, diagnostic procedures, or virtual consultations. The medical billing process begins with this initial encounter, forming the basis for documentation, coding, claims submission, and eventual reimbursement.

Each encounter is assigned a unique identifier and is recorded in the medical billing software. This system allows healthcare providers to capture all the necessary details, including the nature of the service, time spent, diagnosis, procedures conducted, and any follow-up instructions. With the increasing use of electronic health records (EHRs), automated billing tools, and industry-recognized training such as the medical billing and coding certification from AMBCI, the efficiency and accuracy of this process have significantly improved as of 2025.
Types of Patient Encounters in Medical Billing
There are multiple types of encounters in medical billing, and understanding each is crucial for correct coding and reimbursement.
Office Visits
These are routine visits where a patient consults a healthcare provider for non-emergency issues such as annual check-ups or mild health concerns. Office visits are coded using Current Procedural Terminology (CPT) codes based on the visit's complexity.
Emergency Room Visits
Emergency visits occur when a patient seeks urgent medical care. These encounters require detailed documentation and coding that reflects the severity and immediacy of the condition. The higher the complexity, the higher the reimbursement potential.
Inpatient Hospital Visits
When a patient is admitted to a hospital, the encounter becomes more complex. The billing process includes the use of Diagnosis-Related Group (DRG) codes which take into account the duration of stay, diagnoses, and treatment.
Outpatient Surgery
These are same-day surgical procedures where the patient does not require an overnight stay. These encounters are coded using CPT codes based on the procedure's complexity and anesthesia level.
Telehealth Visits
With the rise of digital health, telehealth has become a common form of patient encounter. In 2025, these encounters are widely accepted by insurance providers and are coded similarly to in-person visits, with modifiers to account for the virtual nature of care.
Procedure-Based Encounters
These encounters focus solely on specific procedures, such as a colonoscopy or biopsy. Accurate CPT coding is essential here, as even minor discrepancies can result in claim denials.
Diagnosis-Based Encounters
When a patient is diagnosed with a specific illness (e.g., diabetes or hypertension), that interaction is a diagnosis-based encounter. These use ICD-10-CM codes to reflect the condition being treated or managed.
Follow-Up Encounters
These involve revisiting a provider for post-treatment check-ins or continued care. Accurate tracking ensures continuity of care and correct billing.

How Encounters Impact the Medical Billing Process
Patient encounters form the foundation of medical billing. From a billing standpoint, each encounter provides essential information such as the services rendered, time spent, procedures performed, and diagnosis details. Proper documentation and coding are critical to prevent claim denials, ensure compliance with insurance policies, and optimize revenue cycle management.
Inaccurate or incomplete encounter records can result in financial losses, delays in reimbursement, and compliance issues. Insurance companies assess claims based on this documentation, determining payments based on coverage policies and submitted codes. Thus, understanding encounter types and coding standards is crucial for healthcare providers.
Encounter Documentation and Claims Submission
The Role of Encounter Forms
Encounter forms document every aspect of a patient visit, from procedures and diagnoses to the date of service. These forms form the backbone of accurate medical billing. They not only ensure services are billed correctly but also create a comprehensive medical record that supports both treatment planning and audit processes.
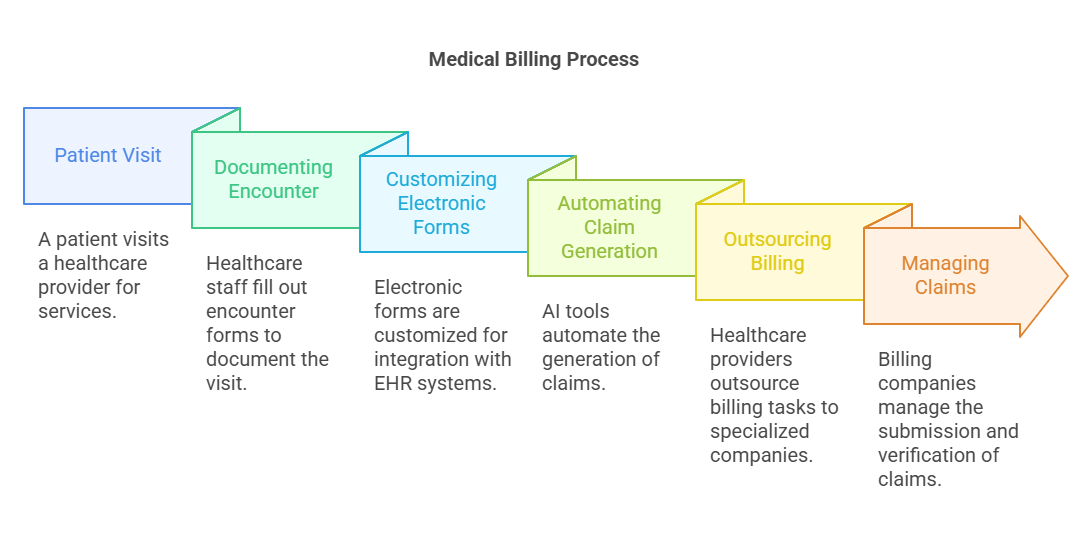
Electronic encounter forms can be customized for different healthcare providers, allowing for better integration with EHR systems and improved billing workflows. As of 2025, cloud-based systems and AI tools are increasingly used to automate claim generation and reduce manual entry errors.
Outsourcing and Automation
Given the complexity of billing, many healthcare providers outsource to medical billing companies. These organizations manage claim submissions, denials, verifications, credentialing, and patient statements. Their expertise ensures accuracy, reduces administrative burdens, and enhances reimbursement rates.
Benefits of Accurate Encounter Documentation
Enhanced Revenue Cycle: Accurate documentation ensures that healthcare providers are reimbursed fairly and timely for all services rendered.
Reduced Claim Denials: Clear and consistent documentation reduces coding errors, improving the rate of accepted claims.
Efficient Practice Management: Automated and electronic documentation tools streamline administrative tasks, allowing providers to focus on patient care.
Improved Patient Outcomes: Thorough documentation helps in continuity of care and better health tracking.
Legal Protection: Proper records serve as legal proof in case of audits or disputes.
Compliance Assurance: Meets regulatory requirements from CMS, HIPAA, and private insurers.

6 Lesser-Known Facts About Patient Encounters in Medical Billing
Encounter data is used in AI healthcare analytics to predict patient outcomes and recommend treatment paths.
SourceCMS mandates encounter data submission for Medicare Advantage plans, making accuracy critical.
SourceIncorrect coding in just 3% of encounters can reduce revenue by up to 20%.
Some EHRs use voice-to-text technology to generate encounter documentation in real-time.
Telehealth encounters must document patient location and provider license compliance across state lines.
SourceIn 2025, many billing software platforms use blockchain for secure and traceable encounter data storage.
Source
Frequently Asked Questions (FAQs)
-
A visit is the physical occurrence, while an encounter is the documented interaction used for billing and record-keeping.
-
It ensures correct billing, minimizes denials, and helps providers get fully reimbursed for services.
-
Yes. A patient might have separate encounters for diagnostics, consultations, and treatments on the same day.
-
Yes, but with additional documentation requirements like technology use and patient consent.
-
It can lead to claim rejections, financial loss, compliance issues, and poor continuity of care.
Key Trends in Encounter-Based Billing
As of 2025, the healthcare industry has made several advances:
AI-driven coding tools are helping reduce human error and speed up documentation.
Blockchain adoption is increasing in billing platforms for enhanced security.
CMS regulations now demand real-time encounter submissions for some insurance plans.
Telehealth reimbursement parity laws are in effect in over 40 states.
EHR integrations now allow direct voice inputs and NLP processing for smoother documentation.
