Mastering Behavioral Health Billing and Coding Training
Behavioral health billing and coding is a critical aspect of ensuring that mental health services are properly reimbursed and compliant with legal standards. With an increasing focus on integrating mental health care into primary care settings, mastering the intricacies of behavioral health billing and coding is crucial for healthcare providers. This training not only helps in minimizing claim denials but also improves reimbursement rates and ensures adherence to legal requirements. In this article, we will explore the essential components of this training, its benefits, and how it contributes to the financial stability of mental health services.
The Importance of Behavioral Health Billing and Coding
Behavioral health services are projected to experience a significant economic impact, with the cost of untreated mental health conditions estimated at $300 billion. Effective billing and coding practices are vital to ensuring that healthcare providers receive fair compensation for the services they offer. Pursuing a medical billing and coding certification from organizations like AMBCI can help professionals stay current with industry standards and best practices. Accurate billing also supports the continuity of mental health services, which in turn allows providers to offer top-quality care. Behavioral health integration, which involves combining mental health treatment with primary care, has become increasingly important. It impacts billing practices, requiring healthcare providers to use correct codes for integrated services to ensure proper reimbursement.
Behavioral health claims often face higher denial rates compared to general medical claims, which underscores the need for meticulous coding practices. By adhering to the correct billing standards, healthcare providers can avoid legal repercussions, such as fines, and ensure that they are paid appropriately for the services they deliver. This training is essential for understanding the complexities of behavioral health coding and the integration of mental health and physical health services.
Key Components of Behavioral Health Coding Training
Behavioral health coding training focuses on providing professionals with the tools they need to accurately code mental health services. This includes training on ICD-10-CM (International Classification of Diseases) and CPT (Current Procedural Terminology) codes, which are specific to mental health diagnoses and services. Understanding these codes is vital for ensuring that mental health services are billed correctly, whether for individual therapy sessions, psychiatric evaluations, or behavioral health integration with primary care.
Training programs also emphasize the importance of documentation and the role it plays in the coding process. Detailed documentation ensures that each service is recorded accurately and supports the reimbursement process. Professionals in behavioral health coding are taught to understand the nuances of various mental health services, including therapies, medications, and interventions, to ensure precise billing.
Certification and Continuing Education
Certification in behavioral health coding is crucial for demonstrating expertise and ensuring that professionals stay up-to-date with industry standards. Certification programs, such as the Certified Professional Coder (CPC) or Certified Billing and Coding Specialist (CBCS), validate the skills of professionals and are often required to practice in the field. Continuing education is also essential, as it ensures that professionals are aware of any changes in billing procedures, new codes, and evolving healthcare regulations.
For social workers and other mental health professionals, continuing education is often required to maintain their professional credentials. By participating in ongoing training, individuals ensure that they remain compliant with current standards and enhance their knowledge of coding and billing practices.
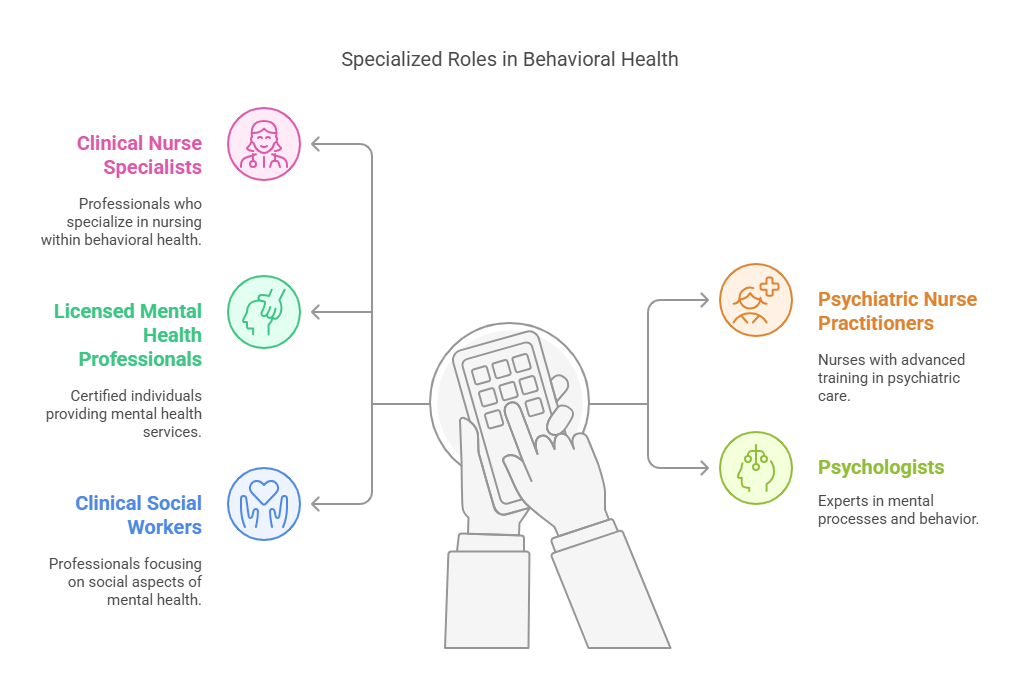
Specialized Roles in Behavioral Health Coding
Within the realm of behavioral health, specialized roles such as clinical nurse specialists, psychiatric nurse practitioners, licensed mental health professionals, and psychologists require specific coding knowledge. Each of these professionals must apply unique CPT and ICD-10 codes that reflect the various therapeutic services and diagnoses associated with their practice. The integration of mental and physical health services further complicates the coding process, requiring an understanding of how to properly code for these integrated services.
For example, clinical social workers often utilize time-oriented codes to reflect the duration of therapy sessions. Accurate billing for these services is essential to ensure proper reimbursement. Additionally, with the rise of telehealth services in behavioral health, new coding practices have emerged to account for virtual sessions. These services require their own set of codes and documentation requirements, ensuring that providers are paid correctly for remote care.
Behavioral Health Coding for Telemedicine Services
As telemedicine continues to grow, billing for telehealth services in behavioral health has become more complex. New CPT codes and guidelines have been introduced to accommodate virtual behavioral health services. Healthcare providers must stay informed about these changes to ensure that telehealth consultations are billed correctly. This includes understanding the specific codes for telebehavioral health and the place-of-service (POS) requirements that distinguish remote consultations from in-person visits.
Telemedicine billing also requires attention to state regulations and insurer policies, which may vary. Therefore, understanding the legal and procedural nuances of telemedicine coding is critical to secure appropriate reimbursement.
Professional Organizations and Resources
Professional organizations play a vital role in supporting behavioral health coding professionals. Groups such as the American Medical Association (AMA), the American Academy of Professional Coders (AAPC), and the Behavioral Health Integration (BHI) Collaborative provide resources, training, and certification opportunities for coders. These organizations offer ongoing educational programs to help professionals stay current with the latest coding practices and industry trends. They also emphasize the importance of behavioral health integration and offer guidance on proper coding and billing practices.
Lesser-Known Facts About Behavioral Health Billing and Coding
Behavioral health claims are typically denied at a higher rate (5-10%) than medical claims, making accurate coding essential for financial stability:
With the rise of telehealth, specific CPT codes for telebehavioral health services have been introduced to capture remote consultations and ensure proper reimbursement:
Telehealth CPT Codes
The integration of mental health services into primary care settings has led to new coding challenges, as providers must accurately document and bill for services that span both physical and mental health care:
Continuing education is mandatory for certain roles, such as clinical social workers, to maintain certification and remain compliant with industry standards:
Proper documentation plays a critical role in the billing process, as it ensures that all services are adequately captured and substantiated for reimbursement:
Billing and Documentation in Healthcare
The adoption of integrated care models in behavioral health can reduce healthcare costs by 12% while improving patient outcomes:
Frequently Asked Questions (FAQs)
-
Accurate billing and coding are crucial for ensuring that healthcare providers receive appropriate reimbursement for their services. It also ensures compliance with legal standards, which is necessary for maintaining the financial stability of behavioral health practices.
-
Behavioral health coding training includes learning about ICD-10-CM and CPT codes specific to mental health, understanding the importance of detailed documentation, and mastering coding for behavioral health integration with primary care services.
-
Certifications such as the Certified Professional Coder (CPC), Certified Billing and Coding Specialist (CBCS), and Certified Coding Associate (CCA) are available to validate the expertise of professionals in behavioral health coding.
-
Professional organizations such as the AMA, AAPC, and BHI Collaborative offer resources, training, and certification opportunities to help professionals stay current with industry trends and maintain their credentials.
-
Accurate documentation and adherence to legal billing standards are essential to ensure compliance and avoid legal issues. These considerations also help ensure that providers receive fair reimbursement for the services they offer.
Conclusion
Mastering behavioral health billing and coding is crucial for ensuring that mental health services are accurately billed and reimbursed. Training in this field provides professionals with the knowledge and skills needed to navigate the complexities of coding for mental health services, including those related to behavioral health integration. By obtaining certifications and continuing education, professionals can stay current with industry standards and legal requirements, ultimately enhancing the financial health and sustainability of behavioral health practices.
This training is essential for healthcare providers who wish to optimize their billing processes, reduce claim denials, and maintain compliance with legal and regulatory standards. By mastering behavioral health billing and coding, providers can ensure that they are compensated appropriately for the critical services they offer.