Top-Rated CPC Coding Class for Aspiring Medical Coders
A Certified Professional Coder (CPC) coding class is an intensive training program that prepares individuals for a career in medical coding. This course teaches students how to accurately assign diagnosis and procedure codes for healthcare services, ensuring proper documentation, billing, and reimbursement. Medical coders play a crucial role in the healthcare industry by maintaining accurate patient records and facilitating insurance claims processing.
With the growing demand for skilled coders, enrolling in a CPC coding class can open doors to stable job opportunities and competitive salaries. The course covers medical terminology, coding guidelines, and various classification systems such as ICD-10-CM, CPT, and HCPCS. Additionally, obtaining a medical billing and coding certification from AMBCI can further enhance your qualifications, making you a sought-after professional in the healthcare industry.
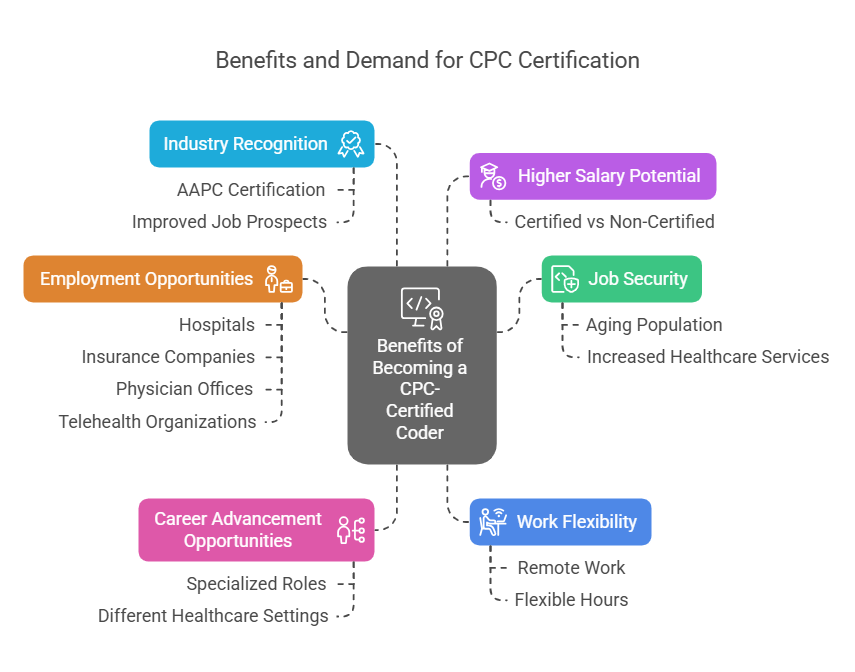
Benefits of Becoming a Certified Professional Coder
Becoming a CPC-certified coder offers several advantages, including:
Job Security – The demand for medical coders is rising due to an aging population and an increase in healthcare services.
Higher Salary Potential – CPC-certified coders typically earn more than non-certified coders.
Career Advancement Opportunities – Certification opens doors to specialized coding roles in different healthcare settings.
Work Flexibility – Many medical coding jobs offer remote work options.
Industry Recognition – Certification from the AAPC is widely respected and improves job prospects.
Employment Opportunities – Medical coders are needed in hospitals, insurance companies, physician offices, and telehealth organizations.
The U.S. Bureau of Labor Statistics projects that the demand for medical records and health information technicians, including medical coders, will grow by 9% through 2032, faster than the average for all occupations.
Key Components of a CPC Coding Class
A CPC coding class covers several essential topics, including:
Medical Terminology & Anatomy – Understanding medical language is crucial for accurate coding.
ICD-10-CM, CPT, and HCPCS Level II Coding – Learning how to classify diseases, procedures, and medical supplies.
Billing and Reimbursement Processes – Knowledge of insurance claims and payment policies.
HIPAA Compliance – Understanding patient confidentiality and security regulations.
Hands-on Coding Practice – Real-world coding scenarios to develop proficiency.
The class format can vary, with options for online learning, in-person training, or hybrid models to accommodate different learning styles.
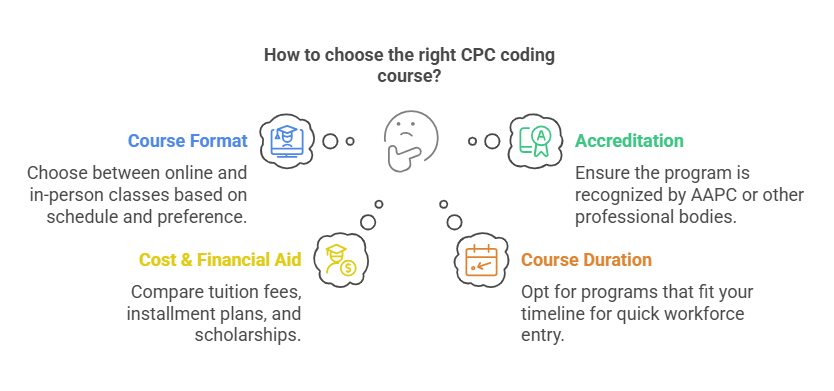
Choosing the Right CPC Coding Course
When selecting a CPC coding course, consider the following factors:
Course Format – Online vs. in-person classes depending on your schedule and preference.
Accreditation – Ensure the program is recognized by AAPC or other professional bodies.
Cost & Financial Aid – Compare tuition fees, installment plans, and available scholarships.
Course Duration – Some programs can be completed in 3–6 months, allowing quick entry into the workforce.
Exam Preparation Support – Look for courses that offer practice exams and study guides.
AAPC membership can also provide additional resources, such as networking opportunities, discounts on certification exams, and access to continuing education programs.
Exam Preparation Strategies
Passing the CPC exam requires proper preparation and time management. Here are some key strategies:
Develop a Study Plan – Allocate time for different sections of the syllabus and review them systematically.
Use Official Coding Books – Familiarize yourself with the ICD-10-CM, CPT, and HCPCS Level II manuals.
Take Practice Exams – Simulate real exam conditions to improve accuracy and speed.
Attend Review Sessions – Join study groups or take part in structured exam prep programs.
Understand Exam Format – The CPC exam consists of 100 multiple-choice questions that assess coding proficiency.
In 2025, the CPC exam is available both in-person and online, making it more accessible for students worldwide.
Cost and Payment Options
The cost of a CPC certification exam in 2025 is:
Single attempt: $399 for non-students, $375 for students.
Two attempts package: $499 for non-students, $475 for students.
Most institutions offer payment plans and financial aid, including state-sponsored scholarships, to help students manage tuition costs.
Career Opportunities for CPC-Certified Coders
Certified medical coders can pursue various job roles, such as:
Medical Coder – Assigns diagnosis and procedure codes for billing.
Medical Auditor – Reviews coding accuracy for compliance.
Coding Educator – Trains new coders and healthcare staff.
Revenue Cycle Analyst – Manages billing efficiency in healthcare organizations.
Medical Billing Specialist – Ensures proper claim submission and payment processing.
With the shift to telehealth services and remote medical coding, professionals now have more opportunities to work from home.
6 Less-Known Facts About CPC Certification
Certification is Not Required but Highly Preferred – While some employers hire non-certified coders, CPC certification significantly improves job prospects and salary potential.
AAPC Members Get Exam Discounts – AAPC members receive discounts on CPC exam fees, study materials, and continuing education.
CPC Certification Can Lead to Specialized Coding Roles – Additional certifications, like Certified Inpatient Coder (CIC) or Certified Risk Adjustment Coder (CRC), can lead to niche career paths.
Continuing Education is Required to Maintain Certification – CPC-certified coders must earn 36 CEUs (Continuing Education Units) every two years to keep their certification active.
Medical Coding Can Be a Remote Career – Many healthcare organizations allow certified coders to work from home.
AI is Changing Medical Coding – Artificial intelligence is assisting with coding tasks, but certified professionals are still needed to validate accuracy and compliance.
Frequently Asked Questions (FAQs)
-
A CPC coding class is a specialized training program that teaches students how to correctly assign medical codes to procedures and diagnoses for healthcare billing and documentation.
-
CPC certification increases job opportunities, improves earning potential, and provides job security in the growing healthcare industry.
-
Look for accredited programs that match your learning style (online or in-person), budget, and career goals. Ensure the course includes exam preparation materials.
-
CPC certification increases job opportunities, improves earning potential, and provides job security in the growing healthcare industry.
-
A CPC coding class is a specialized training program that teaches students how to correctly assign medical codes to procedures and diagnoses for healthcare billing and documentation.
Conclusion
A CPC coding class is a valuable investment for those looking to enter the healthcare industry. With the rising demand for skilled medical coders, certification provides job security, career growth, and competitive salaries. By choosing an accredited course, preparing strategically for the CPC exam, and taking advantage of financial aid options, aspiring coders can secure a promising future in this evolving field.
Medical coding continues to be a high-demand profession, and with advancements in healthcare technology, certified professionals remain essential in ensuring accurate documentation, billing, and compliance.