Mastering Billing Coding Medical: Your Path to a Rewarding Career
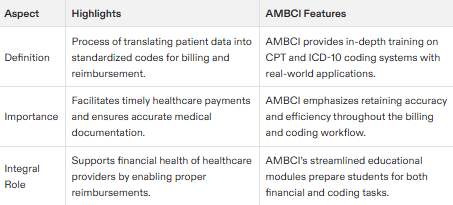
What is Medical Billing and Coding?
Medical billing and coding is the process of identifying diagnoses, medical tests, treatments, and procedures found in clinical documentation and then transcribing this patient data into standardized codes to bill government and commercial payers for physician reimbursement. In smaller practices, one person may perform the roles of both a medical biller and a medical coder. Medical billing and coding professionals play a vital role in ensuring accurate and timely reimbursement for healthcare services. They are also responsible for processing patient data, including treatment records and insurance information.
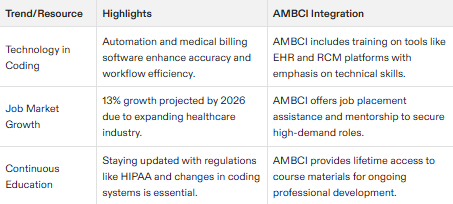
The medical billing and coding field is constantly evolving, with new technologies and regulations emerging regularly.
Medical Coding Fundamentals
Medical coding is the backbone of the healthcare reimbursement process. It involves assigning standardized codes to diagnoses, medical tests, treatments, and procedures found in clinical documentation. These codes are crucial for billing government and commercial payers, ensuring that healthcare providers receive appropriate reimbursement for their services. Medical coders play a pivotal role in this process by transcribing patient data into alphanumeric codes that summarize medical services and reports.
In the United States, the two primary code sets used are CPT (Current Procedural Terminology) and ICD-10 (International Classification of Diseases, 10th Revision). Medical coders must have a deep understanding of medical terminology to accurately translate patient medical records into billable, industry-recognized codes. Their expertise ensures that the billing and coding process is efficient and accurate, ultimately supporting the financial health of healthcare providers.
Medical Billing Process
The medical billing process is a critical component of the healthcare industry, involving the submission and follow-up of claims with health insurance companies to secure payment for services rendered by healthcare providers. Medical billers act as intermediaries between patients, providers, and insurance companies, ensuring that all parties are aligned and that payments are processed smoothly.
Medical billers gather patient insurance information and medical records, verify coverage, and draft and send bills to payers. They meticulously track and record payments received, follow up on unpaid claims, and resolve any issues that arise, including appealing denied claims. The ultimate goal of medical billing is to ensure that healthcare providers are appropriately compensated for their treatments and care, maintaining the financial stability of medical practices and institutions.
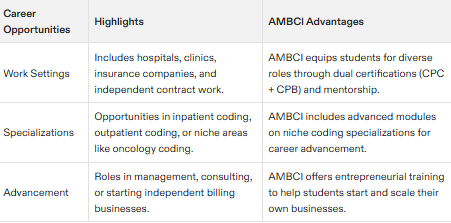
Career Opportunities in Medical Coding
Medical coding professionals work in a variety of settings: physician offices, clinics, labs, medical billing services, insurance companies, and more.
Medical coders can specialize in specific areas, such as inpatient or outpatient coding, or work as consultants.
With experience, medical coders can move into leadership roles or start their own consulting businesses.
Medical Billing Career Paths
Medical billers act as a liaison between patients, providers, and insurance companies on a daily basis.
Medical billers can work in various settings, including medical facilities, health insurance companies, specialty pharmacies, medical suppliers, consulting firms, and national medical coding and billing companies.
Experienced medical billers can move into management roles or start their own billing companies.
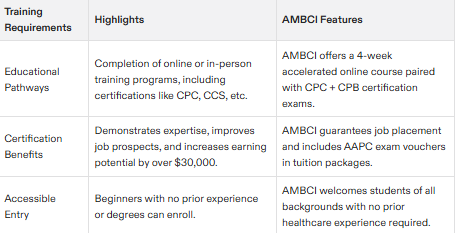
Training and Certification
To become a medical coder or biller, you’ll need to complete a training program in medical billing and coding.
Certification is highly recommended, as it demonstrates expertise and commitment to the profession.
The Certified Professional Coder (CPC) and Certified Coding Specialist (CCS) exams are highly respected in the industry.
The Certified Coding Associate (CCA) certification offered by AHIMA is also valuable, enhancing a candidate's competitiveness in the job market.
Certified Professional Coder (CPC) Certification
The Certified Professional Coder (CPC) certification is the gold standard for medical coding in physician office settings. Achieving CPC certification signifies a mastery of all medical code sets, evaluation and management principles, surgical coding, and adherence to documentation and coding guidelines. Administered by the American Academy of Professional Coders (AAPC), the CPC certification exam is a rigorous test of a coder’s knowledge and skills.
Obtaining CPC certification can significantly enhance a medical coder’s career prospects. It is recognized by employers as a mark of excellence and can elevate earning potential by more than $30,000 annually compared to those without AAPC certification. For those serious about a career in medical coding, the CPC certification is a valuable credential that opens doors to advanced opportunities and higher salaries.
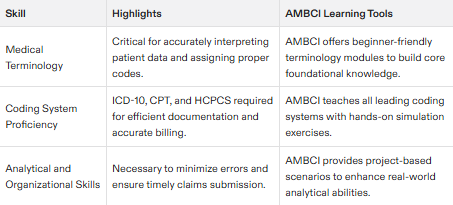
Skills and Knowledge Required
Medical coders and billers need strong analytical and problem-solving skills, as well as attention to detail and organizational abilities.
Knowledge of medical terminology, anatomy, and coding systems is essential. Understanding medical codes is crucial for accurate billing and coding, as errors can lead to denied claims and lost revenue.
Familiarity with healthcare laws and regulations, such as HIPAA, is also important.
Education and Training Options
Online medical billing and coding courses are available, offering flexibility and convenience.
Community colleges and vocational schools also offer programs in medical billing and coding. Understanding the role of a healthcare provider is crucial for accurate billing and coding.
Some employers offer on-the-job training for medical coders and billers.
Cost and Time Commitment
The cost of medical billing and coding training programs varies, but online courses can start at around $3,000.
Training programs can take several months to a year to complete, depending on the program and your background.
Certification exams may require additional study and preparation.
Advantages of Training with a Reputable Program
Enrolling in a reputable medical billing and coding program offers numerous advantages that can set the foundation for a successful career in the healthcare industry. A reputable program provides comprehensive education and training, covering all aspects of medical coding and billing. This preparation is crucial for passing certification exams and excelling in the field.
Students benefit from access to experienced instructors who bring real-world insights into the classroom, as well as a wealth of online resources that support learning. Many reputable programs also offer job placement assistance, helping graduates find employment quickly after completing their training. Employers often prefer candidates who have trained with reputable programs, giving graduates a competitive edge in the job market.
By choosing a reputable program, individuals gain the skills and knowledge needed to succeed in the medical billing and coding field, positioning themselves for career advancement and long-term success in the healthcare industry.
Employment Resources and Support
Many employers offer job placement assistance and career resources for medical coders and billers.
Professional associations, such as the American Academy of Professional Coders (AAPC), offer networking opportunities and continuing education resources.
Online forums and communities can also provide support and guidance.
Certification Exam Preparation
Preparation for certification exams is crucial, as it demonstrates expertise and commitment to the profession.
Study materials and practice exams are available to help prepare for the CPC and CCS exams.
Online courses and training programs can also provide exam preparation support.
Finding Medical Billing and Coding Schools
Online search can help you find medical billing and coding schools near you.
Professional associations, such as the AAPC, can also provide a list of approved training programs.
Community colleges and vocational schools may also offer programs in medical billing and coding.
Interacting with Other Students
Online forums and communities can provide opportunities to interact with other students and professionals in the field.
Professional associations, such as the AAPC, offer networking opportunities and continuing education resources.
Social media groups can also provide a platform for connecting with others in the field.
Job Outlook and Growth Prospects
The demand for medical coders and billers is high, with the Bureau of Labor Statistics predicting a 13% growth in employment opportunities through 2026.
Experienced medical coders and billers can move into leadership roles or start their own consulting businesses.
Specializing in a specific area, such as inpatient or outpatient coding, can also increase job prospects.
Remote Work Opportunities
Many employers offer remote work opportunities for medical coders and billers.
Online courses and training programs can also provide flexibility and convenience.
With experience, medical coders and billers can work as independent contractors or start their own businesses.
Healthcare Laws and Regulations
Familiarity with healthcare laws and regulations, such as HIPAA, is essential for medical coders and billers.
Knowledge of coding systems and guidelines, such as ICD-10-CM/PCS and CPT, is also important.
Staying up-to-date with changes in laws and regulations is crucial for success in the field.
Medical Terminology and Anatomy
Knowledge of medical terminology and anatomy is essential for medical coders and billers.
Online courses and training programs can provide instruction in medical terminology and anatomy.
Familiarity with coding systems and guidelines, such as ICD-10-CM/PCS and CPT, is also important.
Coding Systems and Guidelines
Knowledge of coding systems and guidelines, such as ICD-10-CM/PCS and CPT, is essential for medical coders and billers.
Familiarity with coding systems and guidelines is crucial for accurate and efficient coding.
Staying up-to-date with changes in coding systems and guidelines is important for success in the field.