Career Opportunities for CCS Certified Coders
Certified Coding Specialists (CCS) hold one of the most in-demand credentials in the medical coding industry. Issued by AHIMA, this certification validates expertise in hospital inpatient coding, including mastery of ICD-10-CM and ICD-10-PCS, plus strong knowledge of healthcare reimbursement methodologies. Unlike generalist certifications, CCS demonstrates coding specialization in acute care settings, which opens doors to high-responsibility roles and advanced career tracks.
Today’s healthcare employers—from academic hospitals to compliance contractors—prioritize CCS-certified professionals for their precision, speed, and command of DRG assignment logic. With the industry rapidly shifting toward data-driven reimbursement and tighter coding accuracy benchmarks, the CCS credential acts as both a career stabilizer and a salary booster. And with remote work and AI-assisted coding tools scaling across the U.S., CCS coders can now access nationwide opportunities without relocating. This blog breaks down the most valuable CCS career paths, salary expectations, specialized domains, and strategic ways to sharpen your edge—whether you're just starting out or ready to pivot into higher-paying coding roles.
What Is CCS Certification?
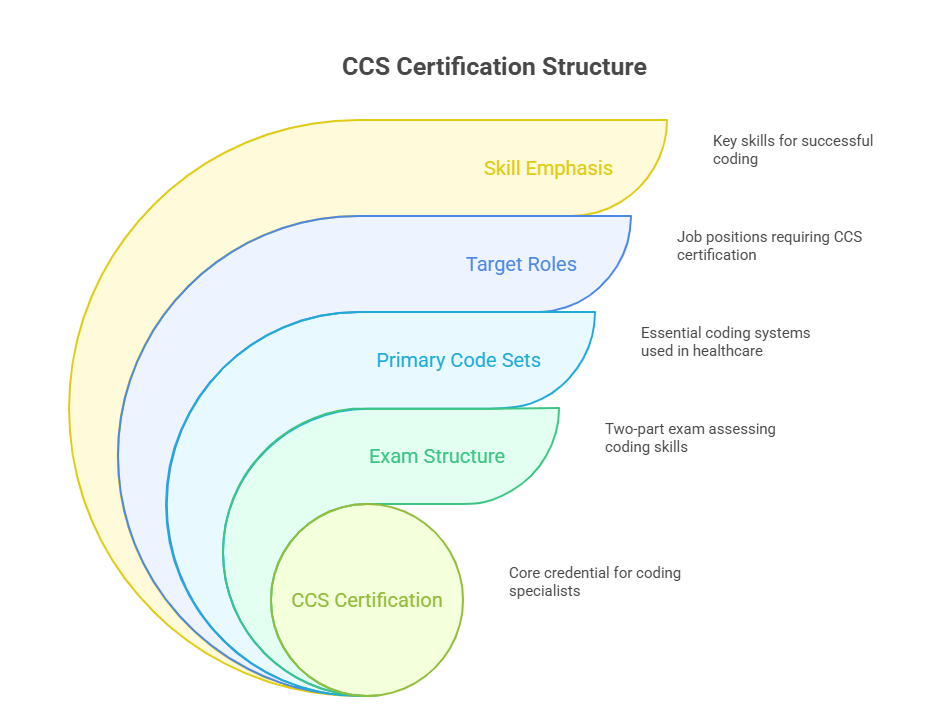
The Certified Coding Specialist (CCS) credential is issued by the American Health Information Management Association (AHIMA) and is recognized industry-wide as a benchmark for advanced coding competency. Unlike entry-level certifications, CCS validates your ability to code independently in inpatient hospital settings, using ICD-10-CM, ICD-10-PCS, and CPT when necessary. The certification is intended for coders who are already proficient and want to advance into acute care, compliance, or DRG-focused roles.
Earning the CCS credential demonstrates not just technical skill, but deep comprehension of reimbursement systems like MS-DRGs, case mix analysis, and compliance measures under CMS guidelines. This positions you as a highly specialized contributor within revenue cycle teams. CCS certification is often listed as a requirement—or strong preference—for positions like inpatient coder, DRG validator, coding auditor, and even clinical documentation improvement (CDI) analyst.
Employers favor CCS-certified candidates when stakes are high: think high-dollar hospital claims, audits, payer disputes, or Medicare compliance projects. It’s not just about coding speed; it’s about accuracy, integrity, and reimbursement impact. That’s why CCS-certified coders often command higher salaries and have more upward mobility within coding departments, particularly in hospital-based settings and federal projects.
Overview of AHIMA's Certified Coding Specialist Exam
The CCS exam is a four-hour computer-based test administered via Pearson VUE. It includes two sections: multiple choice and medical scenarios that require real-world coding. Candidates must demonstrate proficiency in assigning accurate ICD-10-CM, ICD-10-PCS, and CPT codes, as well as understanding complex reimbursement scenarios, privacy regulations (HIPAA), and official coding guidelines.
AHIMA recommends—but does not require—that applicants have at least two years of coding experience, ideally in a hospital or acute care environment. Formal education through an AHIMA-approved or CAHIIM-accredited program is advantageous but not mandatory. What matters most is hands-on coding knowledge and fluency with EHR systems.
The exam is rigorous: many test-takers fail on their first attempt due to poor preparation, especially around inpatient coding rules and scenario-based application. That’s why reputable CCS prep programs emphasize case-based simulations, audit-style exercises, and reimbursement scenario analysis rather than just rote memorization.
CCS vs CPC vs CCA Roles
While all three are recognized coding credentials, they target different segments of the healthcare system. The CCA (Certified Coding Associate) is AHIMA’s entry-level certification, suitable for recent grads or new coders. The CPC (Certified Professional Coder), offered by AAPC, is outpatient-focused and ideal for those coding for physician offices or ambulatory surgery centers.
In contrast, CCS is inpatient-heavy and diagnosis-intensive. It’s designed for coders who want to master ICD-10-PCS procedures and assign MS-DRGs—skills that directly impact hospital reimbursement. CPCs are typically employed by clinics, whereas CCS coders work in hospital revenue cycle teams, coding departments, or for vendors serving hospital contracts.
Another distinction: CCS requires strong knowledge of Medicare Severity Diagnosis Related Groups (MS-DRGs) and coding compliance audits. These aren’t core requirements for the CPC or CCA. That’s why CCS-certified coders are often chosen for DRG validation, CDI support, or pre-bill coding audits—high-stakes areas with greater advancement potential.
Core Job Settings Hiring CCS Coders
The CCS credential opens doors to some of the most specialized and stable roles in medical coding. Because it emphasizes inpatient coding and DRG assignment accuracy, healthcare systems, federal contractors, and private payors all actively seek CCS-certified professionals for their most complex coding functions. Employers value this credential not just for billing accuracy but for its compliance and audit-readiness assurance.
Let’s explore the most common job environments where CCS coders thrive—and how each setting offers unique career progression paths.
Hospitals, Payors, and Compliance Firms
Acute care hospitals are the top employers of CCS-certified coders. These facilities rely on CCS professionals to code inpatient encounters, validate DRG groupings, and prevent reimbursement errors. In Level I trauma centers and academic hospitals, CCS coders often work side-by-side with CDI specialists and clinical teams to refine documentation, support accurate severity of illness (SOI) and risk of mortality (ROM) scores, and minimize audit risk.
Integrated health systems, such as Kaiser Permanente or Cleveland Clinic, also employ CCS coders at scale—both in-house and through centralized revenue cycle hubs. These coders are often embedded in HIM (Health Information Management) teams and work on high-priority coding queues where accuracy directly affects institutional revenue.
Private insurers and Medicare Advantage payors hire CCS professionals for internal audit teams. These coders are responsible for validating submitted claims, performing retrospective reviews, and ensuring coding aligns with HCC, MS-DRG, and clinical criteria. With healthcare fraud investigations on the rise, CCS coders are also recruited into coding integrity roles that support SIU (Special Investigation Unit) efforts.
Compliance consulting firms—especially those serving hospital groups or state Medicaid contracts—seek CCS coders as DRG validators and pre-bill auditors. In these settings, coders often work across multiple client accounts, reviewing high-dollar inpatient charts for proper sequencing, principal diagnosis accuracy, and query opportunities. These roles offer higher hourly pay and audit exposure, especially for experienced professionals.
Remote Coding & Telehealth Positions
The demand for remote CCS coders has surged, particularly post-2020. Hospitals and third-party vendors have expanded their remote teams to maintain productivity while controlling overhead. As a result, CCS-certified coders can now work from any U.S. location, often earning region-independent salaries.
Many health systems use platforms like 3M 360 Encompass or Optum CAC to facilitate remote coding, and they prefer CCS-certified professionals because of their ability to navigate ICD-10-PCS and inpatient documentation complexity without onsite oversight. These positions typically come with productivity targets but offer flexibility in work hours and access to national-level job markets.
Remote CCS coders also play a vital role in telehealth documentation audits. As telemedicine expands into hospital-at-home programs and virtual inpatient consults, organizations rely on coders who can accurately interpret hybrid documentation and ensure compliant billing. CCS certification is frequently required because of the technical accuracy needed for inpatient and transitional care billing.
Remote audit firms and coding vendors also recruit CCS coders as independent contractors. These roles offer contract-based flexibility, higher pay rates, and access to specialized projects like pre-bill audits, appeals support, or DRG education modules. The key requirement across all these settings? Verified CCS credentialing, ongoing CEUs, and proven command over inpatient code sets and reimbursement frameworks.
| Setting | What CCS Coders Do There |
|---|---|
| Acute Care Hospitals | Assign inpatient diagnosis and procedure codes, validate MS-DRGs, ensure accurate revenue capture, and prevent over/underpayments based on clinical documentation. |
| Academic Medical Centers | Handle high-complexity surgical and trauma charts, collaborate with CDI specialists, and support physician query processes to improve coding accuracy. |
| Private Payors | Review submitted claims for inpatient coding accuracy, conduct retrospective audits, and ensure DRG assignments meet medical necessity and payer guidelines. |
| Compliance Firms | Perform third-party DRG validation, execute pre-bill coding audits for hospitals and Medicaid plans, and manage cross-client coding quality assurance. |
| Remote Vendors | Serve as contract coders on inpatient hospital accounts, audit charts, prepare appeal packets, and support RAC or MAC audit response initiatives. |
| Telehealth Programs | Audit hybrid inpatient/telehealth documentation, assign codes for virtual consults, and ensure billing aligns with evolving CMS telemedicine rules. |
| Integrated Health Networks | Code inpatient charts across multiple facilities using centralized EHR systems, monitor coder productivity and accuracy, and support centralized revenue teams. |
Specializations Within CCS Roles
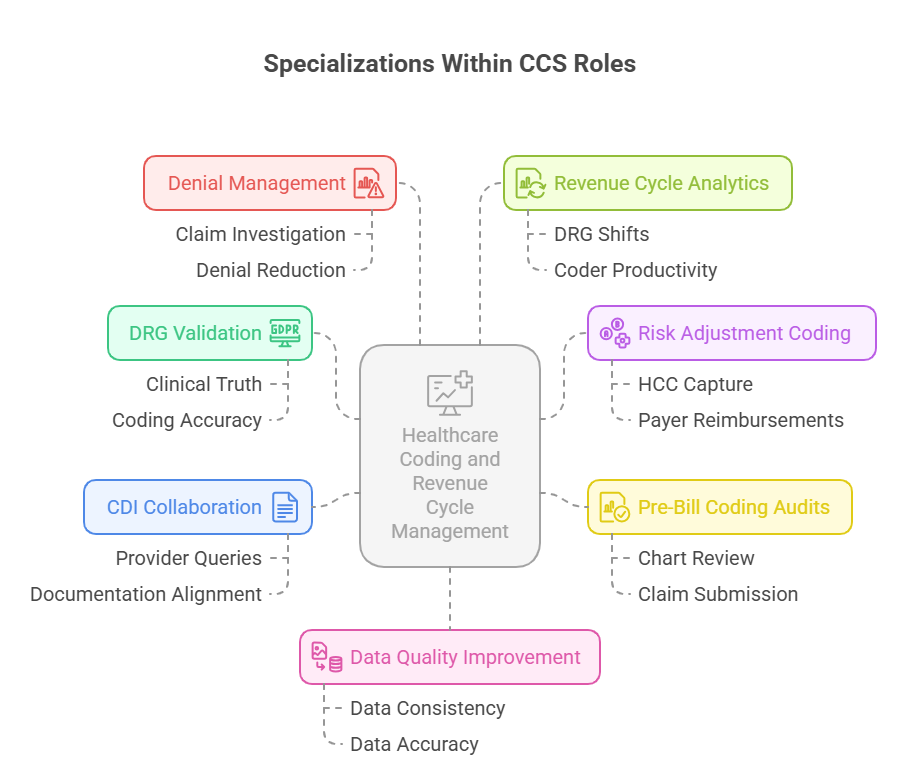
Once certified, CCS coders can move beyond general coding into high-impact specializations that influence hospital revenue, compliance risk, and clinical documentation accuracy. These roles often come with higher compensation, greater autonomy, and influence over revenue integrity decisions. Two of the most sought-after specialization areas are DRG validation and audit support and revenue cycle/data quality improvement.
DRG Validation, Risk Adjustment, Auditing
DRG validation is one of the most lucrative specializations for CCS coders. In this role, coders re-review inpatient charts to verify whether the assigned MS-DRG matches the true clinical picture, ensuring hospitals receive the appropriate payment and avoid overbilling penalties. These positions exist both within hospitals and in third-party audit firms that serve state Medicaid or Medicare Advantage plans.
A critical skill in DRG validation is understanding clinical criteria for principal diagnosis selection, plus the impact of complications and comorbidities (CCs) and major CCs (MCCs) on final DRG weight. Coders must often escalate documentation discrepancies, initiate queries, and justify DRG shifts with clinical backing.
Risk adjustment coding is another growing field. CCS coders fluent in ICD-10-CM and HCC hierarchies are recruited by payors and ACOs to ensure proper capture of patient severity for risk-scored reimbursement models. Coders in this domain often collaborate with care management and actuarial teams, performing retrospective reviews or working within chart review platforms like Cotiviti and Apixio.
Coding auditors with CCS credentials are employed by both provider organizations and external compliance vendors. Their role is to conduct pre-bill audits, education sessions, and retrospective compliance reviews. Audit coders are responsible for enforcing coding accuracy, training new coders, and flagging patterns that may trigger payer audits or recovery actions.
These advanced specializations often require strong clinical knowledge, critical thinking, and mastery of ICD-10-PCS procedures. As a result, CCS professionals who transition into these roles can see significant salary increases and enjoy more strategic responsibilities in compliance, education, and financial oversight.
Revenue Cycle & Data Quality Improvement
CCS coders also find long-term growth in revenue cycle optimization and clinical data quality roles. These positions focus less on line-by-line code assignment and more on ensuring coding consistency across departments, reducing denials, and improving system-wide documentation habits.
Hospitals often embed CCS coders into denials management teams, where they analyze claim rejections and provide code-based recommendations that prevent future errors. Others participate in CDI alignment committees, helping bridge the gap between physician notes and proper DRG outcomes.
Coders with data analytics skills may enter HIM informatics roles, using tools like Epic Clarity or Tableau to track coding trends, DRG shifts, and revenue leakage. In these roles, CCS-certified staff are not just coding—they’re influencing institutional strategy through data-backed insight.
Average Salaries & Market Outlook
CCS-certified coders consistently earn higher salaries than entry-level or outpatient coders, especially in inpatient and compliance-heavy roles. Their ability to handle complex cases, validate DRGs, and reduce audit risk gives them leverage in both full-time and contract-based markets. Whether you're working in-house or remotely, the CCS credential commands premium pay across all 50 states.
U.S. Salary Ranges by State
On average, CCS coders earn between $68,000 and $92,000 per year, depending on region, experience, and employer type. Coders in states with high healthcare density and payer activity—like California, New York, and Massachusetts—often top the scale, with senior CCS coders earning well over $100,000 annually in high-cost markets.
In rural or lower-cost states, CCS coders typically earn between $60,000 and $72,000, but many supplement income through remote contract work or audits. Additionally, many hospital systems offer performance bonuses tied to coding accuracy, DRG validation success, or revenue targets.
Here’s a snapshot of estimated CCS salary ranges across key regions:
California: $85,000–$105,000
Texas: $70,000–$88,000
Florida: $68,000–$82,000
New York: $80,000–$100,000
Illinois: $72,000–$90,000
Arizona: $65,000–$78,000
Remote National Roles: $75,000–$95,000
Hospitals with unionized coding departments or Level I trauma centers often pay top dollar for CCS-certified talent. Pay is also influenced by the coder’s ability to handle ICD-10-PCS, resolve denials, or manage specialty coding queues.
Contract-based CCS roles with consulting firms may offer hourly rates of $45–$65, especially for coders performing pre-bill audits, DRG reviews, or inpatient HCC coding. These roles are flexible and highly lucrative for experienced professionals with proven audit-readiness skills.
Demand Growth Projections
The demand for CCS-certified coders is forecasted to grow 8%–11% by 2030, according to U.S. Bureau of Labor Statistics data and AHIMA projections. This growth is driven by several trends:
Expansion of Medicare Advantage plans, which rely on accurate inpatient coding
Increased adoption of value-based care and risk adjustment models
Shortage of qualified inpatient coders, particularly for ICD-10-PCS and DRG-heavy roles
Rising volume of inpatient audits, appeals, and compliance reviews
As hospitals double down on coding accuracy to protect revenue, CCS-certified coders are emerging as mission-critical assets across revenue cycle teams, compliance departments, and payer audit units.
Skillsets That Give You an Edge
The CCS credential gets your foot in the door—but what truly separates top-performing coders is technical fluency, ongoing education, and cross-functional adaptability. As healthcare coding becomes more data-driven and integrated with compliance and analytics, CCS professionals must actively sharpen their skillsets to stay competitive. These two categories—technical proficiency and continuous upskilling—have the greatest impact on long-term career growth.
EHR Proficiency, ICD-10-PCS Mastery
Coders who excel in electronic health record (EHR) systems—especially Epic, Cerner, and Meditech—are immediately more valuable to large hospitals and health systems. Employers expect CCS-certified coders to navigate, extract, and validate codes across multiple modules, including inpatient notes, order sets, surgical documentation, and CDI queries. Efficiency in EHR workflows directly affects coder productivity and accuracy.
Another non-negotiable skill? ICD-10-PCS mastery. This procedural code set is required for hospital inpatient coding and is often where many coders fall short. Unlike CPT, ICD-10-PCS requires understanding body systems, root operations, and approach qualifiers. Coders who excel here are typically trusted with high-stakes surgical cases, transplant documentation, or trauma center encounters.
Employers often test ICD-10-PCS proficiency during hiring, especially for DRG validation and audit roles. Mastery here not only boosts salary potential—it signals to hiring managers that you can handle complex, high-dollar inpatient cases with minimal supervision.
Continuing Education & Specialty Credentials
Ongoing education is critical in a field where guidelines change yearly. CCS coders who actively earn CEUs, micro-credentials, or secondary certifications gain an edge in promotions, contract offers, and leadership roles. AHIMA offers specialty certifications like CDIP (Clinical Documentation Improvement Practitioner) and RHIT (Registered Health Information Technician) that pair well with CCS.
Additionally, coders who pursue credentials in risk adjustment (CRC), auditing (CCA or CHC), or informatics gain access to broader job markets. For example, a CCS + CDIP combo is ideal for CDI leadership roles, while CCS + CRC is attractive to Medicare Advantage contractors and ACOs.
Top employers also look for CCS coders who participate in AHIMA conferences, coding roundtables, and case-based workshops. This signals a commitment to lifelong learning and shows initiative beyond basic compliance.
Finally, mastering payer policies—especially CMS inpatient reimbursement rules, NCCI edits, and audit defense practices—positions you as a revenue safeguard, not just a coder. Those who consistently invest in education are the ones who move fastest into lead roles, audit consulting, or remote education teams.
| Skill Area | Why It Matters |
|---|---|
| ICD-10-PCS Proficiency | Essential for coding complex inpatient procedures; directly impacts DRG accuracy and hospital reimbursement. Many CCS roles require advanced PCS logic and surgical coding confidence. |
| EHR System Navigation | Fluency in systems like Epic or Cerner improves coding speed, minimizes documentation errors, and supports accurate interpretation of multi-module inpatient records. |
| CDI Collaboration Skills | Ability to align coding with provider documentation ensures better DRG outcomes, supports SOI/ROM accuracy, and reduces query response times across teams. |
| Continuing Education (CEUs) | Keeps coders up to date with new coding guidelines, CMS changes, payer rules, and audit triggers—making them more valuable and compliance-ready. |
| Add-on Certifications (CDIP, CRC) | Expands eligibility for advanced roles in CDI, risk adjustment, and auditing. Enhances your marketability and boosts long-term salary potential. |
| Data Literacy (Excel, Tableau) | Enables coders to analyze DRG shifts, spot coding trends, and support revenue cycle analytics. Increasingly important in large health systems. |
| Payer Rule Knowledge | Understanding of CMS, NCCI edits, and payer-specific denial patterns equips coders to defend claims, write appeals, and reduce revenue loss. |
Fast-Track Your CCS Career with AMBCI’s Advanced Coding Pathway
If you're serious about leveling up into inpatient hospital coding, DRG auditing, or high-paying remote roles, you need more than just basic training—you need a pathway that’s designed for real-world CCS exam success. That’s exactly what AMBCI’s Medical Billing and Coding Certification Prep delivers.
Built around the full AHIMA CCS exam blueprint, this program covers ICD-10-CM, ICD-10-PCS, MS-DRGs, HIPAA compliance, and coding scenarios, all while preparing you to handle chart audits, query logic, and reimbursement analytics. You’ll learn how to navigate inpatient EHR documentation and master procedural coding through case-based simulations, not just theory.
This isn’t a passive video course. It’s an instructor-developed curriculum with interactive modules, timed practice exams, and DRG-based coding drills—the exact skills you’ll use daily in the field. Whether you’re transitioning from CPC roles or entering the hospital coding space for the first time, ACMSO’s certification pathway gives you a tactical advantage.
Frequently Asked Questions
-
A CCS certification qualifies you for roles such as inpatient medical coder, DRG validator, clinical data analyst, CDI support specialist, and coding auditor. These roles exist across hospitals, Medicare Advantage plans, revenue cycle vendors, and federal compliance contractors. You may also work in specialized functions like risk adjustment coding or telehealth audit review. Some CCS-certified coders transition into leadership roles such as coding supervisor or compliance trainer, especially if they combine their credential with CDIP or RHIT certifications. Overall, CCS opens doors to higher-paying, more complex coding roles beyond what entry-level or outpatient credentials offer.
-
It depends on your career goals. CCS is ideal for coders targeting inpatient hospital settings or advanced DRG-related roles. CPC, from AAPC, focuses on outpatient and physician-based coding, while CCA is AHIMA’s entry-level credential for beginners. If you're aiming for roles in hospital revenue cycle departments, DRG auditing, or inpatient CDI, then CCS is more aligned with your goals. It also commands higher salaries in most markets due to its technical rigor and specialized scope. Many coders even pursue both CPC and CCS to expand their job opportunities across settings.
-
Yes—remote coding jobs for CCS-certified professionals have surged since 2020. Hospitals, third-party vendors, and insurance firms now actively hire remote inpatient coders, especially for DRG validation, pre-bill audits, and Medicare Advantage risk adjustment reviews. These roles typically require access to secure EHR systems like Epic or 3M 360 Encompass and may involve productivity tracking. Many CCS-certified coders also work remotely as independent contractors, handling multiple client accounts across the country. With CCS, you're eligible for remote jobs offering $75K–$95K annually, often without geographic limitations.
-
The CCS exam is known to be challenging due to its case-based format and scenario-driven coding tasks. It tests not only your knowledge of ICD-10-CM, ICD-10-PCS, and CPT, but also your ability to apply codes accurately based on complex clinical documentation. Many candidates fail the exam on their first attempt due to gaps in procedural coding and reimbursement rules. Preparation requires more than reading—it demands hands-on practice with inpatient coding cases, DRG assignments, and real EHR scenarios. The most effective prep courses simulate exam conditions and emphasize audit-style accuracy, not just speed.
-
Salaries for CCS-certified coders vary by region, role, and experience. Entry-level inpatient coders typically earn around $68,000–$75,000 annually. With 3+ years of experience or specialization in auditing or DRG validation, coders can earn $85,000–$100,000 or more. Remote contract roles may offer hourly rates between $45–$65, especially for those performing high-stakes coding reviews or Medicare appeals support. Employers in states like California, New York, and Massachusetts tend to offer the highest salaries, but remote positions are leveling pay across states. Certifications like CDIP or CRC, when combined with CCS, can further boost salary potential.
-
No, a degree is not required to take the CCS exam, though it helps. AHIMA recommends—but does not mandate—that applicants have formal training in medical coding, anatomy, pharmacology, and reimbursement systems. Many successful candidates come from certificate programs or accelerated coding bootcamps, provided they include hands-on ICD-10-PCS practice. Some employers prefer candidates with an associate degree or RHIT credential, but it's not a barrier to certification. What matters most is your coding fluency, accuracy under pressure, and ability to interpret inpatient documentation confidently—skills developed through focused prep programs like ACMSO’s.
-
CCS (Certified Coding Specialist) focuses on accurate code assignment and reimbursement integrity—mainly coding inpatient encounters and assigning MS-DRGs. In contrast, CDIP (Clinical Documentation Improvement Practitioner) emphasizes documentation accuracy, working closely with providers to clarify notes and align documentation with coding best practices. While CCS is coding-heavy, CDIP leans more into communication, query writing, and clinical validation. However, the two credentials complement each other. Many coding leaders hold both CCS and CDIP, making them highly effective in audit defense, query compliance, and CDI leadership roles. Together, they unlock senior positions in coding departments and hospital revenue teams.
-
For most learners, it takes about 4 to 6 months of focused preparation to pass the CCS exam, assuming they already have basic coding experience or a CPC background. Those starting from scratch may need 8 to 12 months, including foundational training in medical terminology, anatomy, ICD-10-CM, and ICD-10-PCS. The time commitment depends on your schedule, prior exposure, and the quality of your prep program. Self-paced certification courses like the one offered by ACMSO allow flexible timelines but still emphasize case-based application to ensure you’re truly exam- and job-ready—not just memorizing codes.
Summing Up: Unlocking Long-Term Roles
The Certified Coding Specialist (CCS) credential is more than just a career step—it’s a gateway to high-impact, high-paying roles in the healthcare system. As coding complexity increases and hospitals face greater scrutiny over reimbursement, CCS-certified coders are becoming indispensable to both clinical and financial operations. From DRG validators and audit specialists to remote inpatient coders and CDI collaborators, the job landscape is rich and expanding.
Those who succeed long-term aren’t just technically accurate—they’re adaptable, compliance-minded, and committed to ongoing education and specialty growth. Whether you aim to transition from CPC-level coding, break into hospital systems, or lead revenue integrity initiatives, CCS gives you both the credibility and capability to stand out.
Start smart: choose a prep program like AMBCI’s Advanced CCS Certification Pathway, designed to take you from concept to command. The healthcare industry is ready to reward skilled, certified coders. All you need is the right launchpad—and the focus to build a career that lasts.