Next Steps After Earning Your CPC Certification
You’ve done it—you’ve earned your CPC certification, and that feeling of accomplishment is real. After the rigorous exam prep, sleepless nights, and hours spent decoding CPT, ICD-10-CM, and HCPCS codes, the weight has finally lifted. But what comes next isn’t always clear. Many new certified coders find themselves caught between relief and uncertainty, wondering how to translate this hard-won credential into a thriving career.
The key now is momentum. You’re entering a competitive—but expanding—job market where organizations urgently need coders who are not just certified, but confident in their tools, specialization, and billing fluency. Whether you’re looking to break into your first healthcare role, build niche experience, or grow your salary trajectory with complementary certifications, this post-certification phase is where those strategic moves begin. Done right, these next steps won’t just secure you a job—they’ll launch you into a future-proof career path in medical coding and health revenue cycle management.
First 30 Days Post-Certification: What to Do
Update LinkedIn, Resume & Job Boards
The moment you pass your CPC certification exam, your professional brand must reflect that. Recruiters regularly scan job boards and LinkedIn for credentialed coders—if your profile doesn’t list your CPC, you’re already being overlooked.
Start by adding "Certified Professional Coder (CPC)" to your name field on LinkedIn and headline. Update the certifications section, and craft a 2–3 sentence summary highlighting your coding focus (e.g., outpatient coding, physician services). If you completed a recognized course or internship, mention that in the experience section. Employers want to see initiative, not just credentials.
On your resume, position the CPC at the top under your name. List it before your education, and in your skills section include tools like encoder software, claim scrubbers, and EHR familiarity. Upload this resume to AAPC’s job board, Indeed, and FlexJobs, and enable alerts for "remote CPC coder" and "entry-level medical coding."
This simple refresh can open real doors—often within days.
Apply to Medical Billing Roles by Specialization
With your CPC in hand, it's time to stop browsing generically and target roles that align with your coding strength—especially outpatient, family practice, dermatology, or radiology coding. Employers aren’t just hiring coders—they’re hiring coders who understand their clinical workflow.
Start with outpatient clinics and physician groups. These are often the most receptive to new CPC holders, especially if you’ve trained on Evaluation & Management (E/M) coding, modifiers, and surgical packages. Use the AAPC Job Board to filter by specialty. A posting labeled “OB/GYN Coder – CPC Required” tells you they’re open to certified but not necessarily experienced candidates.
Next, target remote contract firms. These often offer per-chart or per-hour work for specific specialties, such as cardiology or anesthesia. Many of them use cloud-based tools and asynchronous schedules, which are ideal for new coders building real-world exposure.
Also search for hybrid roles labeled “medical billing & coding”—these often blend front-end billing tasks with backend coding. Even if they lean more billing-heavy, it’s a way in.
Finally, don’t ignore temporary and internship roles posted by RCM vendors or healthcare staffing firms. A three-month contract might not offer benefits, but it gives you hands-on CPT/ICD-10 experience, a referral, and a much easier time landing your second job.
Expanding Your Credentials Further
CPB and Specialty Credentials from AAPC
After earning your CPC, one of the highest-leverage moves is to pursue AAPC’s Certified Professional Biller (CPB) or a specialty coding certification. These credentials complement your CPC by sharpening your focus—either horizontally across the billing process or vertically within a specialty.
The CPB credential is a natural pairing. While the CPC centers on accurate code selection, CPB ensures you understand the reimbursement side—claims processing, denial resolution, and payer policies. Employers love this combo because it means fewer rejected claims and a coder who understands end-to-end revenue impact.
Alternatively, look into AAPC’s specialty credentials like CGSC (General Surgery), CEMC (E/M), or CANPC (Anesthesia). If you already work in—or want to break into—a specialty clinic, this niche credential gives you an instant edge over other CPCs in the candidate pool.
Even without immediate experience, these credentials show one thing: you’re not a passive coder—you’re committed to mastery.
HIM & Revenue Cycle Management Certifications
Medical coding is one part of a much larger operational engine. If you're aiming to lead teams, oversee systems, or transition toward hospital or enterprise roles, then Health Information Management (HIM) and revenue cycle certifications can fast-track you.
Consider the RHIT (Registered Health Information Technician) from AHIMA. It's ideal for coders aiming for data integrity, analytics, or EHR optimization roles. Many HIM departments require dual competency in coding and information systems, and RHIT bridges that perfectly.
Another pathway is HFMA’s Certified Revenue Cycle Representative (CRCR). While not as coding-heavy, CRCR focuses on payer relations, front-to-back revenue cycle operations, and patient access workflows. It's excellent for coders aiming to lead cross-functional RCM teams or collaborate with billing departments more fluently.
The further you go up the ladder, the more hiring managers expect system-level thinking, not just code accuracy. HIM and RCM certs show that you speak both languages.
Compliance or Auditing Certifications (CRC, CIC)
If you have an analytical mindset and a low tolerance for errors, compliance and auditing may be your calling. These roles pay well, demand precision, and are always in high demand at payers, hospitals, and large medical groups.
Start with AAPC’s CRC (Certified Risk Adjustment Coder) if you're interested in Medicare Advantage or value-based care environments. CRC coders ensure accurate HCC coding, which directly impacts provider reimbursements and compliance audits.
For hospital coding specialists, the CIC (Certified Inpatient Coder) is the gold standard. It requires strong knowledge of DRG assignment, ICD-10-PCS procedures, and discharge coding guidelines. It’s ideal for CPCs looking to move into inpatient or facility settings.
Each of these credentials positions you not just as a coder, but as a coding strategist—a role that pays more and influences quality and revenue outcomes.
| Credential | Strategic Benefit |
|---|---|
| CPB (Professional Biller) | Adds reimbursement, denial, and claims knowledge to complement coding accuracy. |
| Specialty Certs (CEMC, CGSC, etc.) | Boosts niche hireability for specific clinical areas like surgery, E/M, and anesthesia. |
| CRC (Risk Adjustment) | Unlocks Medicare Advantage and value-based coding roles focused on HCC accuracy. |
| CIC (Inpatient Coder) | Leads to facility-based roles requiring DRG, ICD-10-PCS, and discharge coding expertise. |
| RHIT or CRCR | Opens leadership tracks in HIM and revenue cycle management with broader system insight. |
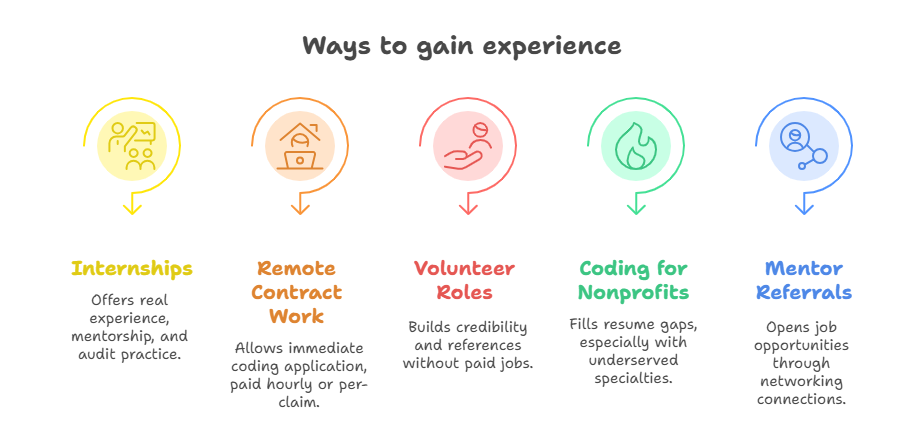
Building Experience and Clinical Know-How
Entry-Level Internships & Remote Contract Work
Even after earning your CPC, many hiring managers prioritize one thing above all: experience. If you're not yet employed, the fastest way to gain real-world coding exposure is through internships or remote contract opportunities—especially those that offer CPT and ICD-10 assignments tied to actual patient cases.
Look for internships through local hospitals, small clinics, or RCM (revenue cycle management) vendors. Some are unpaid, but they offer direct mentorship and access to real encounter notes. Others are part-time, paid roles structured to help bridge newly certified coders into production workflows.
Equally important are remote per-diem or contract coding gigs. Many platforms post chart review or backlog projects that pay per claim or per hour. These roles often require little ramp-up and give you immediate hands-on experience with encoders, scrubbers, and EHR platforms like Epic or Cerner. Be sure to keep every project documented—volume, specialty type, and chart complexity—because it’ll support future salary negotiations.
Start small, but stay consistent. Experience stacks fast when you’re coding daily.
Volunteer Coding Projects or Small Clinics
Volunteer work in the coding field is undervalued and underutilized—but it’s often a direct gateway into your first paid job. Community clinics, nonprofit health centers, and university-affiliated outpatient groups often lack dedicated coding staff and welcome help from certified professionals—even new ones.
Reach out to small practices in your area, especially those in family medicine, urgent care, or behavioral health. Offer to assist with coding cleanup projects, backlogged denials, or even pre-billing reviews. These tasks give you direct access to real patient documentation, allowing you to practice critical skills: modifier use, linking diagnosis codes, and applying LCD/NCD rules.
If you have a mentor or belong to an AAPC local chapter, ask them to connect you with facilities open to volunteer help. These relationships often evolve into referrals or job offers when paid positions open up.
And while you’re volunteering, keep records. Track your hours, chart types, and any measurable impact you contributed—such as improved clean claim rates. It’s not filler. It’s foundation.
Tools Every New CPC Should Master
Encoders, Claim Editors, and Billing Systems
To thrive in your first role as a certified coder, mastering industry-standard tools isn’t optional—it’s essential. The top coders aren’t just accurate with CPT and ICD-10; they’re fluent in the digital tools that drive productivity, reduce rework, and prevent claim denials.
Start with encoder software—platforms like TruCode, 3M, and Optum EncoderPro. These tools streamline code lookup, apply compliance edits, and support logic-based code selection. Many employers will expect you to work within these systems from day one.
Next, familiarize yourself with claim editing tools (e.g., Claim Scrubber or Optum Claims Manager). These systems flag coding errors, bundling violations, and payer-specific modifier requirements before claims are submitted. Knowing how to use them makes you not just a coder, but a billing partner.
Finally, build comfort with EHR-linked billing systems like eClinicalWorks, Athenahealth, or Epic's HIM module. These platforms combine clinical documentation with revenue cycle workflows—and being proficient in them makes you highly marketable.
Code Lookup Resources & Audit Trackers
Accuracy in medical coding isn’t just about knowledge—it’s about using the right tools to apply that knowledge in context. Top coders use a stack of verified lookup tools and internal systems to cross-reference guidelines, detect discrepancies, and track trends.
Bookmark reliable code lookup tools like the AAPC Codify platform, CMS code lookup site, and Find-A-Code. These give you real-time access to CPT Assistant references, NCCI edits, LCD/NCD rules, and payer-specific guidance—all critical for compliant coding.
Also build an internal system for audit tracking. Even a basic spreadsheet can track denied claims, coding patterns that cause red flags, and documentation gaps across specialties. The goal is to spot trends early, especially with modifier misuse, upcoding risks, or missing linkage between codes.
This isn’t just a good practice—it’s how you transition from coder to specialist. The ability to audit your own work in real time sets you apart in any RCM environment.
AI-Based Coding Assistance Tools
Artificial intelligence is rapidly changing the coding landscape. As a new CPC, you’re entering the field at a time when AI-assisted coding (AIAC) isn’t a luxury—it’s becoming standard across midsize and enterprise practices.
Tools like CodaMetrix, nThrive, and 3M M*Modal use natural language processing (NLP) to scan EHR documentation and suggest CPT/ICD-10 codes in real time. Learning how to validate, override, or adjust AI-generated suggestions will be a day-to-day part of your coding workflow.
AI tools also offer predictive logic and risk score assessments. For example, in risk adjustment environments, they help identify missed HCC opportunities or diagnosis code specificity gaps—critical in value-based care settings.
Don't fear AI. Learn how to work with it. Knowing how to manage AI-assisted coding platforms puts you in a position to scale your work faster, audit more effectively, and take on higher-level cases confidently.
| Tool Type | Examples & Purpose |
|---|---|
| Encoders | TruCode, 3M, and Optum EncoderPro help coders accurately assign CPT, ICD-10, and HCPCS codes. These tools apply bundling logic, enforce payer rules, and increase code selection speed while reducing human error. |
| Claim Editors | Platforms like Claims Manager and Claim Scrubber identify bundling errors, modifier misuse, and unsupported diagnoses before claims are submitted. They help prevent rejections and shorten reimbursement timelines. |
| Billing Systems | Tools like Epic (HIM module), Athenahealth, and eClinicalWorks allow coders to work directly within electronic health records. These systems integrate billing, scheduling, and documentation to streamline charge capture and claim submission. |
| Lookup Tools | Codify by AAPC, CMS Code Lookup, and Find-A-Code provide access to coding guidelines, NCCI edits, LCD/NCD coverage details, and CPT Assistant references. These ensure coding accuracy and regulatory compliance. |
| Audit Trackers | Coders use Excel, Google Sheets, or custom tools to monitor coding trends, error rates, and denial reasons. Tracking this data enables self-auditing, root-cause analysis, and improves overall coding quality. |
CPC Salary Benchmarks & Career Pathways
Entry-Level CPC Salary Averages by Region
One of the most important questions after earning your CPC is: What should I expect to earn? While salaries vary by geography, experience, and setting, there are clear benchmarks every new coder should know before accepting an offer.
Nationally, entry-level CPC holders earn between $42,000 and $52,000 in their first year. However, location plays a major role. In metropolitan areas like New York City or San Francisco, salaries start closer to $55,000–$60,000, while rural or smaller markets may begin near $40,000–$45,000.
Here’s a breakdown of estimated first-year salaries by region:
Northeast (e.g., Massachusetts, New Jersey): $50,000–$58,000
South (e.g., Florida, Texas): $42,000–$50,000
Midwest (e.g., Ohio, Illinois): $44,000–$52,000
West Coast (e.g., California, Washington): $54,000–$60,000
Remote (nationwide firms): $45,000–$55,000
Additional factors like working in a specialty practice, mastering key tools, or having a CPB alongside your CPC can increase offers by $3,000–$6,000 in year one. Don’t settle for the minimum if you bring added value to the table.
Promotions: Senior Coder, Auditor, Manager Roles
CPC certification is your entry point—but it doesn’t define your ceiling. Within 2–4 years, coders who build a portfolio of experience, accuracy, and additional credentials can move into higher-paying, more strategic roles.
The first promotion pathway is Senior or Lead Coder. These roles typically require 18–24 months of experience and proficiency in claim audits, denials, and specialty coding. They come with salaries ranging from $58,000 to $70,000, especially in larger practices or multispecialty groups.
Next is Coding Auditor. These professionals review charts for accuracy, compliance, and revenue integrity. Employers look for CRC or CPMA certification, plus 2+ years of clinical coding experience. Salaries for coding auditors range between $65,000 and $80,000, with remote roles widely available.
Finally, there’s the transition into Coding Manager or RCM Supervisor. These are leadership roles that combine team oversight, performance metrics, and payer interaction. Professionals in these roles typically earn $75,000–$95,000, with bonuses tied to claim resolution rates or documentation compliance.
Climbing the ladder depends on two things: measurable outcomes (like reduced denial rates or increased clean claim percentages) and continuous upskilling. If you treat the CPC as your baseline—not your peak—you can reach six-figure roles faster than most expect.
Why AMBCI’s Medical Billing and Coding Course Is the Smart Next Step
Gain reimbursement strategy skills alongside coding
After earning your CPC, the most valuable upgrade isn’t just more codes—it’s mastering the billing and reimbursement logic behind them. That’s where AMBCI’s dual certification pathway stands out. Pairing the CPC with the CPB means you’re not only fluent in CPT and ICD-10, but also in claim lifecycle management, payer policies, denial prevention, and revenue optimization.
Most entry-level coders lack billing fluency, which can hold them back from higher-paying or leadership roles. This program closes that gap. You’ll gain practical skills in payer-specific guidelines, EDI workflows, and front-end denial management—making you indispensable to any healthcare or RCM team. It’s not just a dual credential—it’s dual leverage in the job market.
Dual CPC + CPB Certification by AMBCI
If you’re ready to go beyond code books and into career-building revenue skills, explore the Dual CPC + CPB Certification by AMBCI. It’s fully online, AAPC-aligned, and designed to help you get certified and job-ready in less than 3 months. The CPC opens doors—but the CPB opens budgets. Together, they put you on track for long-term financial and professional growth in medical billing and coding.
Frequently Asked Questions
-
For most CPC-certified coders, it takes anywhere from 3 to 12 weeks to land their first position—depending on location, resume presentation, and whether additional credentials or experience are in place. Coders who proactively update their LinkedIn, resume, and apply daily to specialized billing roles tend to find jobs faster. Adding a CPB certification or taking on short-term remote contract work significantly improves response rates. Employers prioritize candidates who understand both coding and the reimbursement pipeline. If you pair your certification with practical exposure—even unpaid—you’ll accelerate interviews. Platforms like AAPC’s job board, Indeed, and specialty forums are excellent for daily monitoring and applications.
-
Yes, but it requires strategic positioning. Many employers label roles as “CPC preferred” but are open to hiring new coders—especially those who show initiative through internships, volunteer experience, or dual certifications like the CPC + CPB. Emphasizing coding tools (e.g., encoder use, EHR familiarity), resume optimization, and willingness to work remote contracts or entry-level hybrid roles makes you far more attractive. Clinics, smaller hospitals, and third-party billing services are more flexible than large systems. Remember, you’re not competing with veteran coders—you’re competing with other new CPCs. Those who build experience and specialize quickly get hired first.
-
The CPC (Certified Professional Coder) focuses on accurate code selection—CPT, ICD-10, and HCPCS coding tied to clinical documentation. It’s all about translating patient encounters into billable codes. The CPB (Certified Professional Biller), on the other hand, is about revenue mechanics—understanding claim submissions, denials, payer policies, EOB interpretation, and patient billing workflows. Coders with both certifications aren’t just accurate—they’re efficient, reducing denials and accelerating payments. Most healthcare employers value this combo highly, especially for roles that bridge coding and billing teams. It’s a strategic pairing that helps you stand out and move up faster.
-
It depends on your career goals and current job prospects. If you’re aiming to work in a specific clinical area (like general surgery, OB/GYN, or E/M), a specialty certification such as CGSC or CEMC can make you far more competitive. However, if you’re still applying broadly or lack a defined path, starting with a CPB or gaining work experience first may offer more flexibility. Specialty certs are most effective when tied to your job environment. That said, even without direct experience, taking a specialty exam demonstrates dedication, niche interest, and readiness for advanced cases, all of which can tip hiring decisions in your favor.
-
Yes—but they’re competitive. Remote roles often require coders to be independent, efficient, and highly accurate, since training and oversight are minimal. However, there are contract positions that cater to entry-level coders, particularly through third-party billing firms, temp agencies, and niche remote job boards. The best way to qualify is to build initial experience—whether through internships, small clinic work, or even volunteer coding projects. Also, mastering billing software and encoders, and showing comfort with EHR systems like Epic or Athenahealth, gives you a technical edge. Keep applying daily, and tailor your resume to highlight tech skills and coding reliability.
-
Most first-year CPC-certified coders earn between $42,000 and $52,000, depending on location, industry, and skill set. Coders in large cities or high-demand states may start at $55,000 or higher, especially if they bring a CPB credential or specialty coding knowledge. Remote positions tend to average $45,000 to $50,000, with potential for rapid increases after 12–18 months of consistent accuracy. If you’re applying to entry-level hybrid or billing-heavy roles, expect to start near the lower end—but you’ll gain practical exposure fast. Negotiation improves when you show how your coding reduces rejections and increases clean claim submission rates.
-
After certification, focus on three core categories of tools:
Encoders – TruCode, 3M, and EncoderPro are industry standards.
Billing systems – Learn how to navigate tools like Athenahealth, eClinicalWorks, and Epic’s HIM module.
Code lookup + compliance tools – Codify, Find-A-Code, CMS lookup portals, and tools with integrated NCCI edits or LCDs.
Also gain comfort with Excel or Google Sheets for building audit trackers. Familiarity with AI-assisted coding tools like CodaMetrix or 3M M*Modal is increasingly valuable. Mastering these platforms proves you can code efficiently and keep up with fast-moving revenue teams—exactly what employers are looking for in CPCs today.
The Take Away
Earning your CPC certification is not the finish line—it’s the starting gate. This credential proves your foundational coding knowledge, but what you do next determines your income, specialization, and upward mobility. The most successful CPCs don’t just stop at certification—they build experience, master billing systems, and pursue complementary credentials that multiply their impact.
Whether you’re exploring specialty coding, diving into billing with a CPB, or targeting remote opportunities, the post-certification phase is where momentum matters most. Employers aren’t just looking for certified coders—they want coders who take initiative, optimize revenue, and think like analysts.
So treat your CPC not as a badge, but as a platform to launch your next level—whether it’s a higher salary, a more flexible career, or long-term leadership in health information management. Every step you take now compounds your credibility, income, and career freedom over time.
What’s your next move after earning your CPC certification?