Mastering Coding in Medical: Tips, Training, and Career Paths
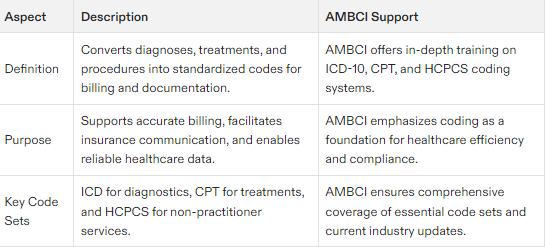
Medical coding, specifically coding in medical contexts, transforms healthcare diagnoses, treatments, and procedures into standardized codes, ensuring smooth billing and accurate medical records. This essential process enables efficient communication with insurance companies, supports research through reliable data, and documents medical necessity to justify treatments, services, or supplies provided to patients. In this article, we will explore the basics of medical coding, essential code sets, the role of a medical coder, and pathways to certification.
Key Takeaways
Medical coding standardizes diagnoses and procedures into codes, facilitating accurate billing and improving healthcare quality.
The key medical coding systems include ICD-10, CPT, and HCPCS, which are vital for reimbursement and healthcare documentation.
Continuous education, certification, and practical experience are essential for success in medical coding, with significant salary potential and career growth opportunities.
Understanding Medical Coding
The translation of medical diagnoses, treatments, and medical procedures into a uniform system of codes represents the essence of medical coding. This crucial step in the medical billing process allows for streamlined communication between healthcare providers and insurance companies to ensure accurate compensation for services provided. Universal medical alphanumeric codes play a vital role in transforming healthcare diagnoses, procedures, medical services, and equipment into a standardized format. Without such standardized codes, there would be rampant confusion with different terminologies being used by various doctors and insurers.
Medical coding also serves as an integral part in maintaining consistency within medical record documentation. This fosters precision within reporting measures and enables proper tracking of administered healthcare services. With the advent of policies like the Affordable Care Act, precise medical coding has become increasingly important to maintain meticulous records for payments received or owed. By standardizing this aspect, not only does it bolster efficiency in billing practices, but it elevates overall health service quality too.
Through converting patient data into globally recognized formats during their work processes, medical coders make substantial contributions towards advancing research across healthcare fields. Their input is critical. Generating reliable information that informs studies on epidemiological patterns and therapeutic effectiveness Ultimately, such detailed accuracy propels advancements in patient care standards while boosting operational proficiency throughout our entire healthcare network.
Medical Coding Process
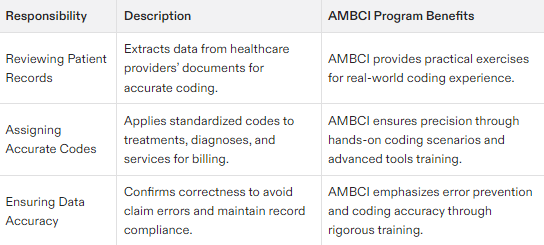
The medical coding process is a meticulous journey that transforms detailed medical information into standardized codes, ensuring seamless communication and accurate billing within the healthcare system. It all begins with the medical coder delving into the patient’s medical record documentation, which includes physician’s transcription notes, lab results, and radiologic findings. This initial step is crucial as it involves abstracting pertinent information such as diagnoses, procedures, and the medical services provided.
Once the relevant data is extracted, the coder assigns the appropriate medical codes using standardized coding systems like ICD-10-CM and CPT. These codes must precisely reflect the patient’s medical condition and the services rendered. The accuracy of this step is paramount, as it directly impacts the reimbursement process and the integrity of the patient’s medical record.
After coding, the report undergoes a thorough review to ensure completeness and accuracy before it is handed over to the medical biller. This review process is essential to catch any potential errors that could lead to claim denials or delays in payment.
Medical coders must exhibit a high level of attention to detail and stay current with the latest coding guidelines and updates. This ongoing education ensures that their coding practices remain accurate and compliant with regulatory requirements, ultimately supporting the efficiency and effectiveness of the entire healthcare system.
Key Medical Code Sets
Medical coding’s foundation is anchored in the diverse code sets designated to catalog medical diagnoses and procedures. The International Classification of Diseases (ICD) stands as a pivotal global system, indispensable for the standardized electronic processing of medical claims. Within the United States, adherence to six official HIPAA-mandated code sets ensures precise and effective medical billing practices. Crucial reference materials for FY2024 encompass HCPCS Level II codes, CPT Professional Edition booklets, along with ICD-10-PCS and ICD-10-CM Code Books.
The extensive ICD-10 code set comprises both ICD-10-CM for diagnostic coding and ICD-10-PCS dedicated to procedure codification, offering over 69 thousand individual codes that span various injuries, diseases, and other health conditions. This broad array offered by ICPCMG delivers meticulous depictions critical in capturing patient health details accurately—a necessary factor influencing treatment strategies as well as billing operations.
A Essential component within this framework is embodied by Current Procedural Terminology (CPT®), holding more than 8 thousand alphanumeric representations which relate distinctly to numerous healthcare services provided. These particular codes are categorized into six sectors based on differing areas such as pathology or surgical services covered under their scope.
To these systems exist HCPCS Level II codes focusing specifically on non-practitioner-related provisions like equipment supplies not included in CPT®, harnessing these uniformed protocols guarantees comprehensive documentation alongside accurate invoicing concerning every element involved in patient care management.
Command over these intricate code compilations remains paramount among medical coders whose expertise supports equitable financial return for healthcare providers’ offerings—integral contributors ensuring seamless continuity throughout our entire healthcare infrastructure.
The Role of a Medical Coder
Healthcare providers rely on medical coders to serve as a crucial link within the healthcare system, facilitating communication between care givers and insurance entities. Medical coders spend their days perusing the patient's medical record from the previous day, condensing critical details from physician’s notes, and assigning appropriate codes for diagnoses and conducted procedures. This detailed coding process is essential in capturing every aspect of a patient’s interaction with healthcare services accurately, which plays an integral role both in billing purposes and ensuring continuity of care.
The foundation for successful coding activities lies in precise medical record documentation by healthcare professionals. The ability to determine accurate codes based on comprehensive and timely documentation is paramount. Without it, there can be considerable repercussions such as significant errors within billing operations that could impact not only revenue streams but also compromise patient treatment quality.
Often operating autonomously, medical coders must occasionally collaborate with fellow colleagues when they encounter complicated cases or need clarification during the assigning of codes. Coders may at times contribute to various tasks associated with billing to guarantee seamless administration of these financial processes. To uphold excellence in code assignment conformity with established guidelines regular scrutiny through monthly evaluations along with constant feedback about coder performance are imperative practices amongst this group of health information management specialists reflecting just how pivotal their expertise is within the broader medical team.
Medical Billing Process
The medical billing process is a critical component of the healthcare revenue cycle, involving the submission and follow-up of claims with insurance companies to secure payment for medical services provided. This process kicks off when the medical biller receives the coded report from the medical coder. The biller then uses this report to create a claim, which encapsulates details about the patient’s visit, symptoms, diagnosis, and treatment.
Once the claim is meticulously prepared, it is submitted to the insurance company for evaluation. The insurance company reviews the claim to determine the coverage and the amount payable. Upon receiving the insurer’s response, the biller assesses the returned claim to ascertain the patient’s financial responsibility, considering factors such as the patient’s insurance plan, co-payments, and any other financial arrangements.
The biller then generates an accurate bill, which is sent to the patient for payment. This step is crucial as it ensures that the healthcare provider receives appropriate compensation for the services rendered.
The medical billing process demands a high level of precision and attention to detail. Accurate billing is essential to avoid claim rejections and ensure timely reimbursement. Medical billers must stay informed about the latest billing guidelines and regulatory updates to maintain compliance and accuracy in their billing practices. This diligence not only supports the financial health of healthcare providers but also contributes to the overall efficiency of the healthcare system.
How to Become a Certified Professional Coder (CPC)
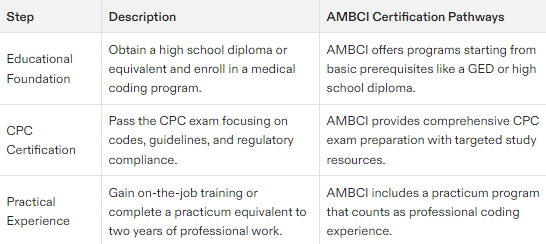
Beginning a career in medical coding necessitates the acquisition of proper education and certification. To meet the typical educational standards, one must earn either a diploma or an associate degree in this field. It’s crucial to undergo training courses that cover coding protocols and best practices, laying down the fundamental skills required for proficient medical coding.
The journey toward becoming a professional coder reaches a significant point upon earning the Certified Professional Coder (CPC) credential from AAPC. Success on the CPC exam is mandatory to secure this certification. It evaluates expertise across several domains such as medical terminology, guidelines adherence, and regulatory compliance. The comprehensive nature of this examination ensures that certified coders are fully prepared to navigate through intricate aspects associated with their profession.
Those who successfully pass the examination but still lack sufficient experience will be granted provisional status under the designation CPC-A (Apprentice). This title affords individuals an opportunity to accrue needed practical exposure while initially working within coded regulations. For full-fledged CPC status achievement requires completing two years of work within medical coding or alternatively fulfilling one year plus additional coursework tailored towards code-specific preparation.
Supportive online materials along with instructional programs offer aspiring coders ways forward toward passing their CPC examinations and upholding these certifications thereafter—effectively streamlining accessibilities into starting off one’s role as a certified coder.
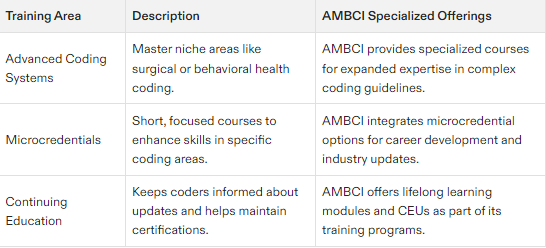
Advanced Training and Microcredentials
The domain of medical coding is subject to constant change, and it is essential for professionals in the field to engage in ongoing education. Microcredentials serve as a tool that allows these individuals to distinguish themselves and broaden their career prospects. These concise programs are crafted with an emphasis on pivotal competencies that healthcare recruiters actively seek, offering participants an advantageous position when seeking employment.
Most microcredential programs tailored for medical coding cover integral subjects such as medical vocabulary, fundamentals of health insurance, and procedures related to coding. By completing these focused courses, medical coders not only augment their skill set but also remain abreast of current developments within the industry—thereby enhancing opportunities for professional growth and progression.
Practical Experience and Job Placement
Practical experience is an indispensable element for anyone pursuing a career in medical coding. Immersing oneself in the field through on-the-job learning allows individuals to translate their academic knowledge into practical application, facing real challenges and tasks. Guidance from seasoned professionals during this stage accelerates skill development by providing critical insights and expert advice.
Externship programs are instrumental in furnishing students with vital hands-on practice, which not only enhances their capabilities but also builds confidence within the realm of medical coding and billing. Achieving certification often necessitates such direct experience, attainable via specialized training initiatives that ensure practitioners remain abreast of evolving technologies and regulatory standards.
The American Medical Billing and Coding Institute (AMBCI) confidently backs its education program with a 6-month job placement assurance. Failure to secure employment within this timeframe triggers a refund of tuition fees paid by the student. Alongside individualized mentorships designed to expedite one’s professional progression, AMBCI Offers comprehensive tutoring services as well as an advanced practicum acknowledged equivalent to two years’ worth of professional work for those preparing for the AAPC examination.
Salary Expectations and Medical Coding Career Growth
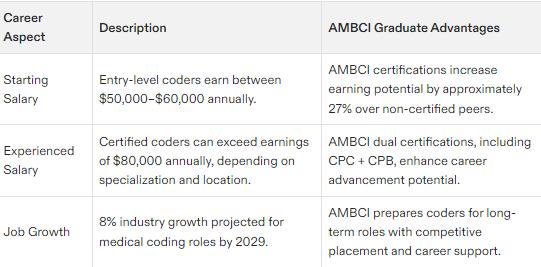
In the healthcare industry, medical coders can anticipate a lucrative career with an average yearly income of about $51,090 throughout the United States. For those just entering the field of medical coding, starting salaries range between $50,000 to $60,000. The earnings for certified coders are notably higher by approximately 27% compared to their peers without certification, which underscores the benefits of professional credentials.
Top-paying states like New Jersey and California offer substantial incomes for medical coders where advanced certifications may lead to annual wages over $80,000. Opportunities for salary enhancement and improved job prospects within the healthcare billing and coding sectors are available through micro-credentials and ongoing education.
Over the next ten years, in this realm of healthcare services including billing and coding, expect a promising 8% growth in employment opportunities due primarily to an increasing elderly population along with intensified emphasis on quality care provision. Career trajectories encompass various roles such as health information technicians alongside positions focused specifically on either medical coder or biller duties. Each path presents diverse possibilities for progression within one’s profession.
Remote Work Opportunities in Medical Coding
Engaging in medical coding from a remote setting presents several advantages that attract many experts in the field. The option to craft one’s work schedule affords coders an improved harmony between their private life and their career duties. Coders working remotely often notice a boost in efficiency, attributed to reduced interruptions and the freedom to design an environment conducive to their workflow.
One significant perk of home-based employment is bypassing the daily travel to and from work, which conserves time and diminishes commute-related stress. Remote roles also translate into financial savings for workers by cutting down on costs associated with transit fares, professional attire purchases, and lunchtime expenses out of pocket. Telecommuting extends job prospects across territorial boundaries, empowering coders with the ability to pursue opportunities situated in various states or even abroad.
Nevertheless, operating from afar brings its own set of hurdles. Ensuring there’s a distinct separation between domestic activities and vocational tasks can be tough. In addition, fostering productive communication might prove more complex when physically distant from colleagues—potentially giving rise to confusion or hold-ups within projects’ timelines., Despite these impediments, embracing remote modalities continues to be a feasible choice growingly embraced among those specializing in medical coding.
Coding Guidelines and Best Practices
Observing coding guidelines meticulously is critical for preserving precision and adherence in the domain of medical coding. Deviating from these standards can lead to economic setbacks and judicial ramifications for healthcare providers. The measurement of code assignment accuracy typically hinges on the proportion of codes assigned correctly, with a common benchmark being a 95% accuracy rate. Maintaining such an exacting standard guarantees that medical billing procedures remain precise and streamlined.
By embracing optimal coding methodologies, healthcare institutions are better positioned to accommodate shifts in coding protocols while upholding quality and compliance within their processes. An anticipatory approach to managing medical codes is vital for securing correct payments, underlining the need for timely, accurate, and uniform application of coding practices.
The diligence demonstrated by medical coders in applying suitable codes plays an instrumental role in enhancing both efficiency and efficacy within the broader healthcare system’s operational framework through meticulous billing practices.
Challenges in Medical Coding
Medical coding encompasses a complex set of tasks that come with their own set of hurdles. Constantly evolving guidelines in the field require medical coders to engage in perpetual learning to ensure they remain precise and adhere strictly to regulations. Frequent staff turnover within these departments can Complicate matters, leading not only to disruptions but also heightened rates of mistakes and inefficiency.
Technical glitches can pose significant barriers for medical coders, especially those working remotely. Issues like unreliable internet connections or software clashes disrupt the smoothness of the healthcare billing cycle. Errors made during this intricate process may result in claim rejections, which subsequently delay reimbursements and add administrative strain—underscoring how critical consistent training and support are for individuals in this profession.
Deficiencies related to documentation stand out as yet another major obstacle confronting coders. Healthcare providers under time constraints often leave behind ambiguous patient records, posing challenges for accurate code assignment by medical professionals tasked with deciphering them. Such inaccuracies hold serious implications for revenue while potentially compromising quality care, when key documentation doesn’t substantiate the necessity medically, a situation addressable only through meticulous coder training paired with effective communication channels and ongoing dedication towards improving quality control measures.
Summary
Embarking on a medical coding career is an intricate process that requires mastering detailed code sets, strictly following established guidelines, and keeping abreast of the latest changes in the field. This guide has offered insights into vital strategies for success, available training options, and potential career trajectories for those interested in becoming medical coders. It’s important to grasp not only what it means to be a medical coder, but also how Education and specialized credentials can significantly enhance one’s proficiency within this profession.
As transformations continue within the healthcare industry, there will be an escalating need for proficient medical coders. Advancing your educational background, securing relevant certifications, and acquiring hands-on experience are all pivotal steps towards cementing your place within this lucrative sector of healthcare. By embracing both the challenges and prospects presented by a career in medical coding, you stand ready to play an integral role at the heart of modern healthcare administration.
Frequently Asked Questions
What are the prerequisites for enrolling in the AMBCI program?
You only need a high school diploma or GED to enroll in the AMBCI program, and no prior experience in healthcare or coding is required.
What is the job placement guarantee offered by AMBCI?
AMBCI guarantees job placement within 6 months and promises to refund tuition fees if a position is not obtained during that period.
How long does it take to complete the Advanced CPC + CPB Certification program at AMBCI?
You can complete the Advanced CPC + CPB Certification program at AMBCI in just 8 weeks. This timeline allows for efficient progress towards your certification goals.
What kind of support do students receive in the AMBCI program?
Students in the AMBCI program receive personalized support through 1-on-1 career acceleration mentorship, tutoring, and advanced practicum opportunities, ensuring they are well-prepared for their future careers.
What is the potential annual salary for graduates of the AMBCI program?
Graduates of the AMBCI program can expect to earn $80,000 or more annually.
This level of income reflects the program’s value in today’s job market.