Coding vs Billing: Key Differences and Best Career Paths
The healthcare sector is a vital pillar of our society, and within it, medical billing and coding play crucial roles in ensuring the financial health of healthcare providers. As we step into 2025, the demand for professionals skilled in either medical billing or coding continues to rise, driven by the growth of healthcare services and the need for precise documentation. However, many aspiring professionals often find themselves at a crossroads when choosing between these two career paths.
In this comprehensive guide, we’ll dive deep into the key differences between medical billing and coding, explore the skills required for each role, and help you make an informed decision on which path is best suited for you. Whether you're a detail-oriented individual looking for an analytical career or someone who thrives in a communicative role, this article will help you understand the nuances of both fields.
Key Takeaways: Medical Billing vs. Medical Coding
In the healthcare industry, two essential roles play a critical part in ensuring that services are properly reimbursed and documented—medical billing and medical coding. These roles are crucial to the smooth functioning of healthcare providers, ensuring that accurate data is submitted for reimbursement purposes and that the financial aspects of patient care are properly managed. However, while these roles are closely linked, they each require distinct skill sets and knowledge. This article will explore the key differences between medical billing and coding, including their functions, responsibilities, required skills, and career opportunities. Additionally, we will discuss how obtaining dual expertise in both areas can enhance job prospects and marketability in the evolving healthcare sector. To help aspiring professionals make informed decisions, we’ll also provide a Best Value Breakdown: Cost for Medical Coding Training—comparing program types, certification paths, and return on investment.
1. Medical Billing: A Front-Facing Role
Medical billing is a vital function in the healthcare industry, focusing primarily on the financial side of healthcare services. Medical billers are responsible for managing insurance claims, payment collections, and patient communications. Their primary objective is to ensure that healthcare providers receive reimbursement for the services they render, whether through private insurance, government programs like Medicare or Medicaid, or out-of-pocket payments by patients.
Responsibilities of a Medical Biller:
Medical billers have a range of responsibilities that are essential to the healthcare provider’s revenue cycle management:
Creating and Submitting Insurance Claims: Medical billers work with medical coders to submit accurate claims to insurance companies. They ensure that the claims are coded correctly based on the medical services provided and that all the necessary documentation is included.
Managing Patient Accounts: Medical billers communicate with patients to verify insurance information and help resolve billing disputes. They ensure that patients are informed about their financial responsibilities, such as copays, deductibles, or out-of-pocket costs.
Collecting Payments: Once claims are processed, medical billers follow up with insurance companies and patients to collect payments. This includes dealing with unpaid or underpaid claims, resubmitting claims, and negotiating payment plans for patients.
Handling Denials and Appeals: If insurance claims are denied, medical billers investigate the reasons for denial and work on resolving any issues. They may file appeals or provide additional documentation to ensure the claim is paid.
Skills Required for Medical Billing:
To succeed as a medical biller, professionals need a combination of organizational skills, attention to detail, and communication skills. Medical billers must be able to work with complex insurance policies, understand billing codes, and have the ability to explain financial details clearly to patients. Additionally, they should be familiar with healthcare billing software, compliance regulations such as HIPAA (Health Insurance Portability and Accountability Act), and the overall medical billing cycle.
2. Medical Coding: A Back-End Role
On the other hand, medical coding involves the translation of medical documentation into standardized codes that are used for billing and insurance claims. These codes ensure that healthcare providers are reimbursed correctly and that insurance companies can process claims accurately. Medical coding is more of a back-end role, focused on the technical and precise aspects of healthcare documentation.
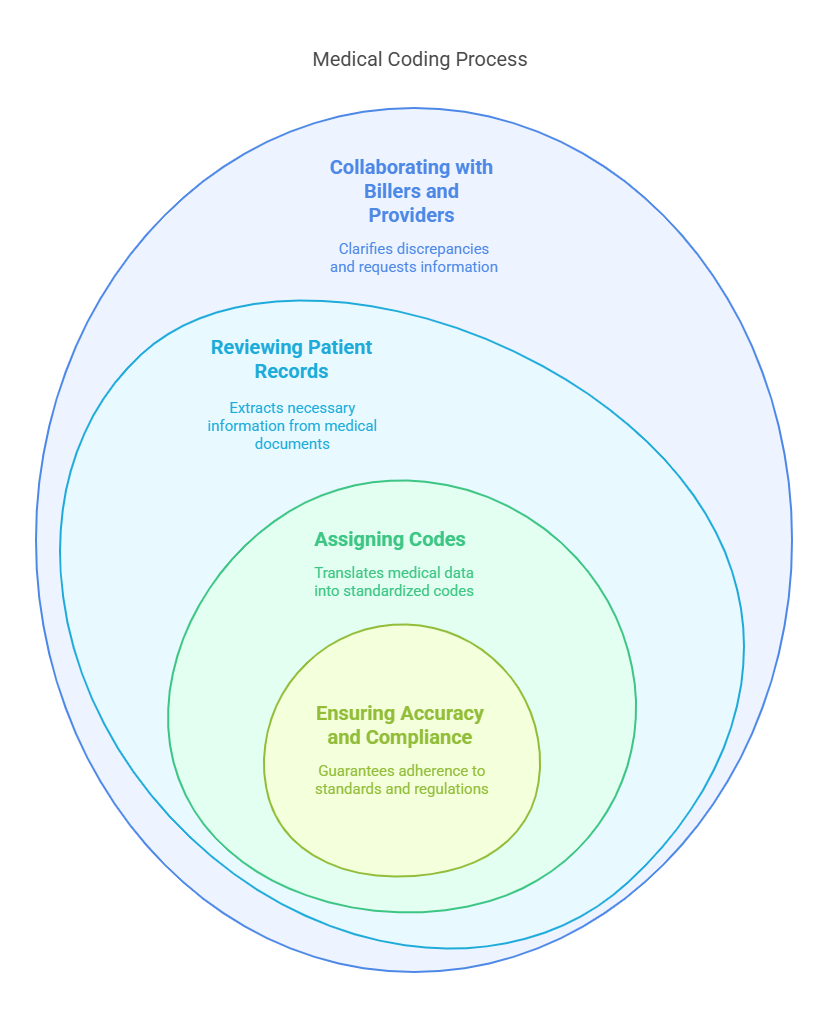
Responsibilities of a Medical Coder:
Medical coders are responsible for converting detailed medical reports, including patient diagnoses, procedures, and treatments, into standardized codes used in the healthcare system. These codes are essential for insurance claims, statistical tracking, and research purposes. The role involves:
Reviewing Patient Records: Medical coders carefully examine medical records, physician notes, lab results, and other documents to extract the correct information regarding diagnoses, procedures, and treatments.
Assigning Codes: Coders assign the appropriate codes to the procedures and diagnoses listed in the medical records. These codes come from established coding systems such as ICD-10 (International Classification of Diseases) for diagnoses and CPT (Current Procedural Terminology) for medical procedures.
Ensuring Accuracy and Compliance: Coders must ensure that the codes they assign are accurate and comply with healthcare regulations and insurance requirements. They also ensure that the coding meets the standards set by various healthcare organizations, including the American Health Information Management Association (AHIMA) and American Academy of Professional Coders (AAPC).
Collaborating with Billers and Healthcare Providers: Medical coders often work closely with medical billers to ensure that the right codes are used for claims. They may also collaborate with healthcare providers to clarify any discrepancies in the documentation or to request additional information.
Skills Required for Medical Coding:
Medical coders need technical knowledge and a deep understanding of medical terminology, anatomy, and the various coding systems used in healthcare. Accuracy is crucial in this role, as incorrect coding can lead to delayed payments, claim denials, or even legal issues. Coders must also be familiar with coding guidelines, regulations, and compliance issues such as HIPAA. Given the rapid advancements in medical technology and practices, coders should also have the ability to adapt and stay updated on changes in coding standards and guidelines.
3. The Differences Between Medical Billing and Coding
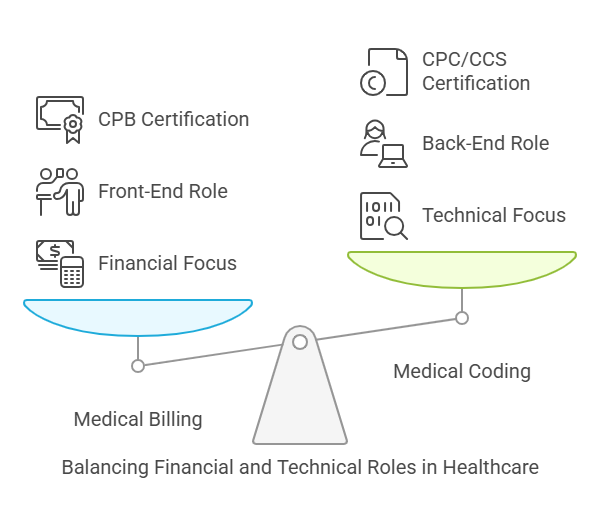
While medical billing and coding are closely related and work hand-in-hand in the healthcare revenue cycle, the primary differences between the two roles lie in their focus and responsibilities.
Key Differences:
Focus on Financial vs. Technical Aspects: Medical billing focuses on the financial aspects of the healthcare process, including claims submission, payment collection, and patient communications. Medical coding, on the other hand, focuses on translating medical documentation into standardized codes for insurance claims and statistical purposes.
Front-End vs. Back-End Role: Medical billing is considered a front-facing role that interacts with insurance companies and patients to ensure payment is made, while medical coding is a back-end process that ensures accurate coding of medical services provided.
Certifications and Training: Both roles require specialized training and certifications, but the specific certifications differ. Medical billing professionals often pursue certifications such as the Certified Professional Biller (CPB), while medical coders typically pursue certifications like the Certified Professional Coder (CPC) or Certified Coding Specialist (CCS). Additionally, coders may specialize in specific areas of medicine, such as radiology, pediatrics, or surgery.
4. The Value of Dual Expertise
In today’s evolving healthcare landscape, dual expertise in both medical billing and coding can significantly enhance a professional’s job prospects and marketability. Employers value professionals who can perform both roles as it increases their versatility and ability to streamline processes within healthcare organizations. Additionally, understanding both sides of the revenue cycle allows for more accurate claims submission, fewer denials, and more efficient patient communications.
Career Opportunities with Dual Expertise:
Increased Job Marketability: Having expertise in both billing and coding makes a professional more adaptable and increases job opportunities. It also allows individuals to fill more specialized roles, such as medical billing and coding specialist or healthcare revenue cycle manager.
Higher Salary Potential: Professionals with dual certification often command higher salaries, as they are seen as more valuable employees who can manage multiple facets of the healthcare revenue cycle.
Expanded Career Pathways: Dual expertise can open doors to more advanced roles, such as medical audit, coding supervisor, or compliance officer, as well as opportunities in healthcare consulting or IT roles focused on healthcare billing and coding systems.
Understanding Medical Billing
What is Medical Billing?
Medical billing is the administrative backbone of healthcare finances. Medical billers ensure that healthcare providers are compensated for their services by processing insurance claims and ensuring that payments are received. This process starts with patient enrollment and continues through to the final payment, where medical billers manage the submission of claims, track payment statuses, and handle patient invoices.
The Billing Cycle: From Patient Check-In to Payment Collection
The journey of medical billing begins when a patient checks in for a service. The process involves verifying patient information, submitting claims to insurance companies or directly billing the patient, and following up until payment is received. Medical billers are tasked with managing this complex cycle, which includes keeping detailed records and communicating with patients and insurers to resolve any discrepancies or claims denials. For those interested in pursuing a career in this vital healthcare field, exploring the Best Medical Billing and Coding Certification Programs in 2025 is an excellent starting point to gain the skills and credentials needed to succeed.
Skills Required for Medical Billing
Proficiency in medical billing requires a combination of technical and interpersonal skills. Some of the key competencies include:
Communication Skills: Medical billers must effectively communicate with both patients and insurance companies to resolve billing issues.
Attention to Detail: Billers must have a sharp eye for detail to ensure accurate billing and prevent costly errors.
Medical Terminology Knowledge: A solid understanding of medical terminology, anatomy, and physiology is crucial for accurate billing.
Regulatory Knowledge: Billers must stay up-to-date with healthcare regulations and coding standards to ensure compliance and reduce the risk of claim denials.
Exploring Medical Coding
What is Medical Coding?
Medical coding is the process of converting patient medical records into standardized codes that are used for billing and insurance purposes. These codes are part of essential coding systems like ICD-10 (International Classification of Diseases) and CPT (Current Procedural Terminology). Medical coders play a vital role in the revenue cycle by ensuring that procedures and diagnoses are accurately coded, which directly impacts the billing process.
The Role of a Medical Coder
A medical coder’s primary job is to read and analyze clinical documents, assigning the correct codes to diagnoses, treatments, and procedures. This requires deep knowledge of medical terminology, anatomy, and coding systems. Coders typically work behind the scenes in hospitals, insurance companies, or private practices, ensuring that patient records are accurately converted into code for billing and insurance claims.
Skills Required for Medical Coding
Analytical Skills: Medical coders must possess strong analytical abilities to interpret complex clinical documents.
Attention to Detail: Precision is paramount in coding, as even small errors can result in claim denials or underpayments.
Medical Knowledge: A firm understanding of medical terminology and anatomy is essential for correctly assigning codes.
Coding Systems Proficiency: Coders must be familiar with multiple coding systems, including ICD-10, CPT, and HCPCS codes.
Comparing Medical Billing and Medical Coding
While medical billing and coding are both crucial for the revenue cycle in healthcare, they serve distinct roles and require different skill sets. Here’s a comparison to help you understand the key differences:
Responsibilities and Job Function
Medical Billers focus on managing claims, verifying insurance information, and communicating with patients and insurance companies. They ensure the timely and accurate submission of claims and follow up on denied claims.
Medical Coders, on the other hand, analyze clinical documentation, assigning codes to diagnoses and procedures. Their primary responsibility is ensuring that medical records are correctly coded to facilitate proper billing.
Work Environment
Medical Billers often work in office settings, where they directly interact with patients, insurance companies, and healthcare providers.
Medical Coders usually work in the background, interpreting medical records and working independently with minimal patient interaction. Many coders also have the option to work remotely.
Salary Comparison
Medical coders typically earn higher salaries than billers due to the more technical nature of their work. However, both fields offer competitive salaries, with pay varying based on location, experience, and industry.
Education and Certification Requirements
Medical Billing Education
To become a medical biller, you typically need a high school diploma or GED, followed by specialized training in medical billing and coding. Many programs are available online or in-person, ranging from certificate courses to associate degrees.
Certification for Medical Billers
Certified Professional Biller (CPB): Offered by the AAPC, this certification enhances a biller's credentials and opens doors to more job opportunities.
Certified Coding Specialist (CCS): This certification, offered by AHIMA, is beneficial for those looking to specialize in coding and billing.
Medical Coding Education
A career in medical coding typically requires a high school diploma followed by a coding-specific training program, often culminating in certification. Some aspiring coders pursue associate degrees in health information management, which provide a broad understanding of both coding and billing.
Certification for Medical Coders
Certified Professional Coder (CPC): Offered by the AAPC, this is the most widely recognized certification for medical coders.
Certified Inpatient Coder (CIC): A certification for those specializing in inpatient coding, offered by AAPC.
Career Opportunities in Medical Billing and Coding
Both medical billing and coding offer ample career opportunities in various healthcare settings. As healthcare regulations become more complex, the demand for skilled professionals in both fields will continue to grow. In fact, the Bureau of Labor Statistics projects an 8% growth rate for medical records and health information technicians over the next decade.
Dual Expertise: Benefits and Challenges
While pursuing expertise in both medical billing and coding can be challenging, it offers distinct advantages. Professionals with dual expertise are highly sought after, as they can take on multiple roles within healthcare organizations, enhancing their job security and career prospects.
FAQs
-
Medical billing focuses on submitting claims and handling payments, while coding involves translating patient records into standardized codes used for billing and insurance.
-
Yes, professionals with expertise in both fields are highly valued by employers, especially in smaller healthcare practices where roles may overlap.
-
Medical billers can earn certifications such as the Certified Professional Biller (CPB) or Certified Coding Specialist (CCS) to enhance their career prospects.
-
Becoming a certified medical coder typically takes 6 months to 2 years, depending on the type of training program you choose.
-
Yes, there is a growing demand for both medical billers and coders, driven by the expanding healthcare industry and the need for precise medical documentation.
5 Lesser-Known Facts About Medical Billing and Coding
1. Medical Billing Errors Cost the Healthcare Industry Billions Each Year
Inaccurate medical billing is a significant issue, with studies indicating that up to 80% of medical bills contain errors. These mistakes can lead to substantial financial losses for healthcare providers. For instance, billing errors contribute to over $125 billion in lost revenue annually for U.S. doctors due to poor billing and coding practices. CollaborateMDConifer Health Solutions
2. Medical Coders Are in High Demand for Remote Work
The demand for remote medical coders has surged, with over 65% of medical records specialists working remotely as of 2025. This shift reflects the growing trend of flexible work arrangements in the healthcare industry. AAPC
3. Medical Coding Helps Reduce Healthcare Fraud
Medical coders play a crucial role in identifying and preventing healthcare fraud by ensuring accurate and standardized coding practices. Their expertise helps detect anomalies and prevent fraudulent billing activities.
4. Specialized Certifications Can Significantly Increase Salary Potential
Certifications in specific coding areas can enhance a medical coder's earning potential. For example, certified coders earn higher average salaries compared to non-certified coders. Additionally, those with multiple certifications can command even higher salaries. AMN Healthcare+1certmage.com+1Nurse.org
5. Medical Coders Often Work with Electronic Health Records (EHR) Systems
EHR systems are integral to the medical coding process, allowing coders to access and input patient data efficiently. These systems streamline the workflow, reduce paperwork, and enhance the accuracy of coding and billing.
Conclusion
The choice between medical billing and coding depends on your personal strengths, career goals, and work environment preferences. Both professions offer rewarding career opportunities, job security, and competitive salaries. By understanding the key differences, required skills, and certifications—such as the medical billing and coding certification offered by AMBCI (American Medical Billing and Coding Institute)—you can make an informed decision on which path is right for you. If you are considering a career in either field, be sure to pursue relevant education and certifications to set yourself up for long-term success in the ever-growing healthcare industry.