Essential Guide to CTC Medical Billing and Coding Certification
Medical billing and coding is a vital process within the healthcare industry that ensures the accurate assignment of codes to diagnoses and procedures for insurance reimbursement. Professionals in this field, including medical billers and coders, play an essential role in maintaining up-to-date and accurate medical records. This process involves the use of medical terminology and coding systems to represent patient data effectively, enabling healthcare providers to be reimbursed for services rendered.
Overview of Medical Billing and Coding
The CTC (Certified Training Center) Medical Billing and Coding Certification prepares individuals for a career in this high-demand field, offering significant job growth opportunities. By obtaining a certificate through accredited educational programs, students can demonstrate their expertise in medical billing and coding, which enhances their professional recognition. This certification is vital for pursuing national certification in medical coding, and it can open doors to better job prospects and higher salaries. The CTC certification is not only a valuable qualification but also a competitive edge in the job market. You can get this certification from AMBCI.
Benefits and Admission Requirements of CTC Certification
To be eligible for CTC programs, students must meet certain admission requirements, which typically include possessing a high school diploma or an equivalent qualification. Before beginning the CTC program, students may need to complete prerequisite courses like medical terminology, anatomy, and physiology. These courses are crucial for providing foundational knowledge needed to succeed in medical billing and coding. In some cases, background checks or additional certifications might be required as part of the program.
The CTC curriculum covers a wide range of essential topics, including medical billing, medical coding, medical records, and medical terminology. The program dives deep into various coding systems, such as ICD-10 and CPT, and teaches students how to apply these codes in real-world settings. The curriculum also addresses key areas like insurance billing and reimbursement, as well as the business aspects of healthcare.
Curriculum and Essential Skills for Medical Billing and Coding
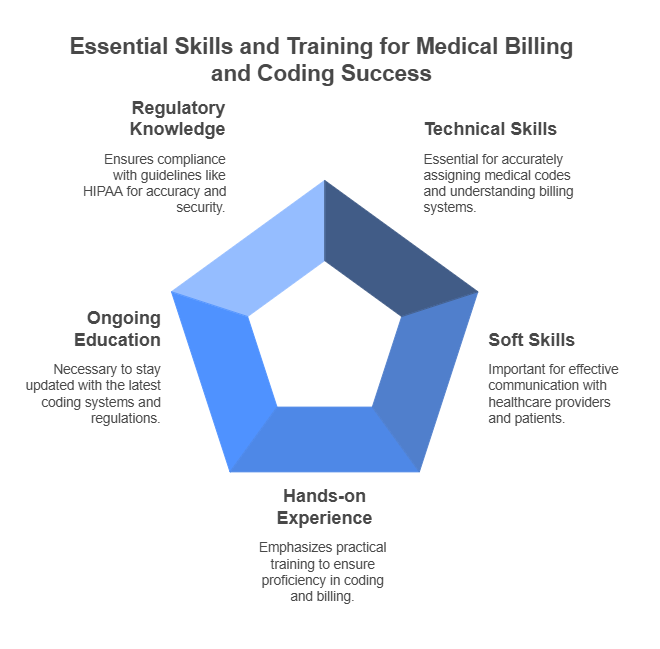
Medical billers and coders need a combination of technical and soft skills. Strong analytical and problem-solving abilities are essential for accurately assigning codes to medical diagnoses and procedures. Additionally, excellent communication skills are important for working with healthcare providers, insurance companies, and patients. Organizational skills, attention to detail, and the ability to work efficiently are also critical in this field.
The CTC program emphasizes hands-on experience, ensuring students are well-versed in coding systems and billing procedures. Medical coders, for instance, must stay current with the latest coding systems and regulations, such as the HIPAA guidelines, to ensure accuracy and security in coding. This requires ongoing education and professional development to keep up with the rapidly changing landscape of medical billing and coding.
Medical Coding Systems and Guidelines
A key aspect of medical billing and coding is understanding the coding systems that dictate how medical procedures and diagnoses are classified. The ICD-10 and CPT coding systems are essential for medical coders to assign the correct codes. Coders must follow specific guidelines to ensure the accuracy of these codes and remain compliant with regulatory standards like HIPAA. As these systems evolve, coders need to adapt to new rules and procedures to maintain accuracy in billing.
Insurance Billing and Reimbursement
A critical component of medical billing and coding is the insurance billing process. Billers must understand how to submit claims to insurance companies and follow up on denied or rejected claims. They should be familiar with various types of insurance, including Medicare and Medicaid, and understand how to navigate the reimbursement process for each. This knowledge is fundamental in ensuring that healthcare providers are compensated for the services they provide.
CTC Certification Process and Career Opportunities
Upon completing the CTC program, students must pass a certification exam to earn their credential. This exam tests their knowledge and proficiency in medical billing and coding. Certification typically lasts for a set period before requiring renewal. Once certified, medical billers and coders can find employment in various healthcare settings, including hospitals, clinics, physician practices, and insurance companies. With experience, they can also move into leadership or management roles within the industry.
The future outlook for medical billing and coding professionals is highly promising. According to the Bureau of Labor Statistics, the employment of medical records and health information technicians, including billers and coders, is expected to grow by 13% from 2020 to 2030, a rate faster than the average for all occupations. This growth is fueled by the increasing demand for healthcare services, driven in part by the aging population. Additionally, the widespread adoption of electronic health records (EHRs) is creating a need for skilled professionals who can manage these digital systems effectively.
Industry Trends and Program Accreditation
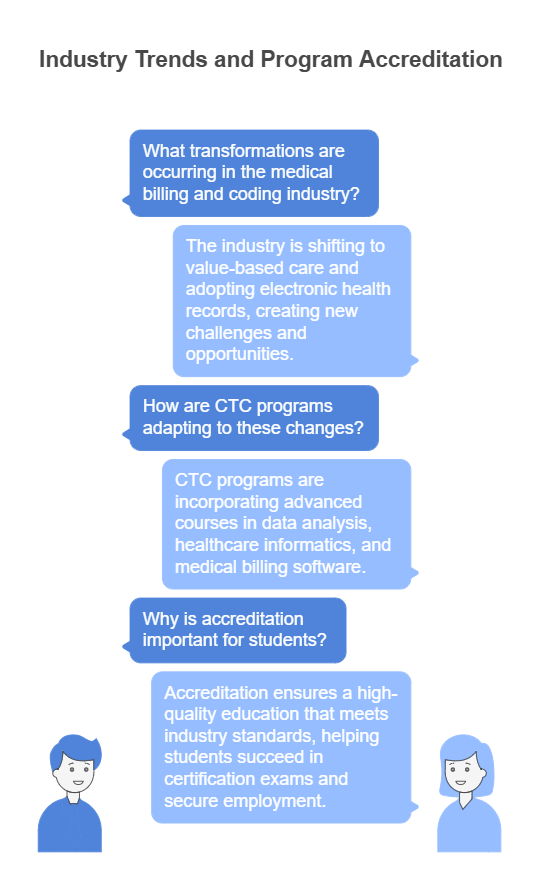
The medical billing and coding industry is undergoing significant transformations, particularly with the shift to value-based care and the adoption of electronic health records. These changes are creating new challenges and opportunities for professionals in the field. To stay competitive, CTC programs incorporate advanced courses in data analysis, healthcare informatics, and medical billing software to prepare students for these evolving industry demands.
The CTC program is accredited by a recognized accrediting body, ensuring that students receive a high-quality education that meets industry standards. Accreditation is a crucial factor for students, as it guarantees that the program provides the necessary training to succeed in the certification exam and secure employment in the field.
Conclusion: The Importance of Medical Billing and Coding in Healthcare
Medical billing and coding is a critical component of the healthcare system, ensuring that medical services are accurately recorded and reimbursed. With the proper training and certification, professionals in this field can enjoy rewarding careers with excellent job prospects. The CTC Medical Billing and Coding Certification program equips students with the skills and knowledge needed to excel in this fast-growing industry. By earning certification, individuals can enhance their career opportunities, increase their earning potential, and contribute to the efficient functioning of healthcare systems.
6 Lesser-Known Facts about Medical Billing and Coding:
Medical coding specialists must update their knowledge regularly:
"Medical coders must regularly update their skills to keep up with the frequent changes in coding systems like ICD-10 and CPT."
American Health Information Management Association (AHIMA) on Medical Coding UpdatesMedical billers work closely with insurance companies:
"Medical billers often collaborate with insurance companies to appeal denied claims, which can be a challenging and time-consuming part of the job."
American Academy of Professional Coders (AAPC) on Billing and InsuranceOver 50% of medical coders work from home:
"Over 50% of medical coders work from home, a trend that has grown significantly since 2020 due to advances in technology and remote work options."
Forbes article on remote work trends in healthcareMedical billing and coding does not require direct patient care:
"Medical billing and coding is one of the few healthcare professions that does not require direct patient care, making it ideal for individuals who prefer office-based work."
U.S. Bureau of Labor Statistics on Medical Coding and BillingSpecializations in medical coding:
"Some medical coding specialists specialize in particular areas, such as oncology or cardiology, requiring a deep understanding of specific medical fields."
AAPC on Coding SpecialtiesAI and machine learning in medical billing:
"A growing trend in medical billing is the use of Artificial Intelligence (AI) and machine learning to streamline coding processes and reduce human error."
Harvard Business Review on AI in Healthcare
FAQs:
-
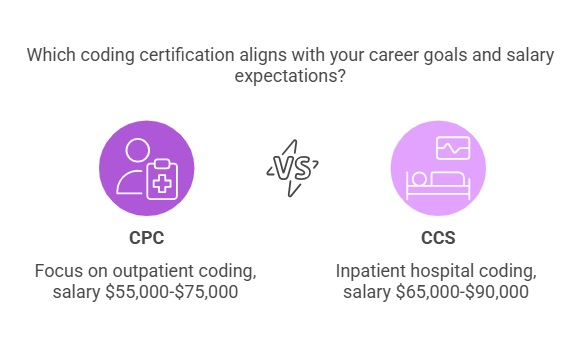
After completing the CTC program, students can pursue certification as a Certified Professional Coder (CPC) or Certified Coding Specialist (CCS), among other options.
-
The median annual salary for medical records and health information technicians was $42,820 in 2020. However, salaries can vary based on location, experience, and certification.
-
The length of the program varies but typically takes around 9-12 months to complete, depending on whether it is pursued full-time or part-time.
-
Certification is not always required, but it is highly recommended as it demonstrates your expertise and can lead to better job opportunities and higher salaries.
-
Medical billing involves preparing and submitting claims to insurance companies for reimbursement, while medical coding involves assigning standardized codes to diagnoses and procedures.