Essential Guidelines for Accurate Clinical Documentation
Accurate clinical documentation is vital to ensure that healthcare providers deliver the best possible care. It directly impacts patient safety, treatment quality, and care coordination. Inaccurate or incomplete documentation can lead to miscommunication, delayed treatments, or errors that compromise patient outcomes. As the healthcare industry shifts toward value-based care, maintaining proper records has become even more essential, ensuring both regulatory compliance and financial stability.
For healthcare professionals, understanding the importance of precise clinical documentation is critical not just for quality care but also for avoiding legal liabilities and maximizing reimbursement. Proper documentation supports compliance with legal standards and improves overall patient care. This guide will provide practical insights into the key elements of clinical documentation, common mistakes to avoid, and effective strategies to enhance accuracy and efficiency in clinical records.
The Importance of Accurate Clinical Documentation
Improving Patient Safety and Care
Accurate clinical documentation plays a critical role in improving patient safety and ensuring the delivery of high-quality care. When healthcare providers document patient information, diagnoses, and treatment plans correctly, it ensures that all team members are on the same page regarding the patient's condition and care plan. This coordination helps to prevent medical errors, misdiagnoses, and adverse events.
Inaccurate or incomplete documentation can have serious consequences, including miscommunication between providers, incorrect medication prescriptions, or delayed treatment. For example, if a patient's allergy history is not properly recorded, they might receive a medication that could lead to a life-threatening reaction. By focusing on accurate documentation, healthcare professionals can minimize risks, enhance patient safety, and improve clinical outcomes. Accurate records also support patient engagement, ensuring patients fully understand their treatment plans and any potential risks involved.
Compliance with Legal and Regulatory Standards
Accurate clinical documentation is not only vital for patient care but also essential for maintaining compliance with numerous legal and regulatory requirements. Healthcare providers are bound by strict laws such as HIPAA (Health Insurance Portability and Accountability Act) and other state and federal regulations to maintain patient privacy and safeguard health records. Failure to adhere to these standards can lead to legal penalties, lawsuits, and damage to the healthcare provider's reputation.
In addition to legal requirements, healthcare providers must meet the reimbursement standards set by organizations like Medicare and Medicaid. Inaccurate documentation can result in denied claims or under-reimbursement for services provided, leading to financial losses. By ensuring accurate, complete documentation, healthcare organizations protect themselves legally and ensure they are reimbursed appropriately for the services provided. Proper documentation also provides a clear audit trail, which is critical during inspections and reviews by regulatory bodies.
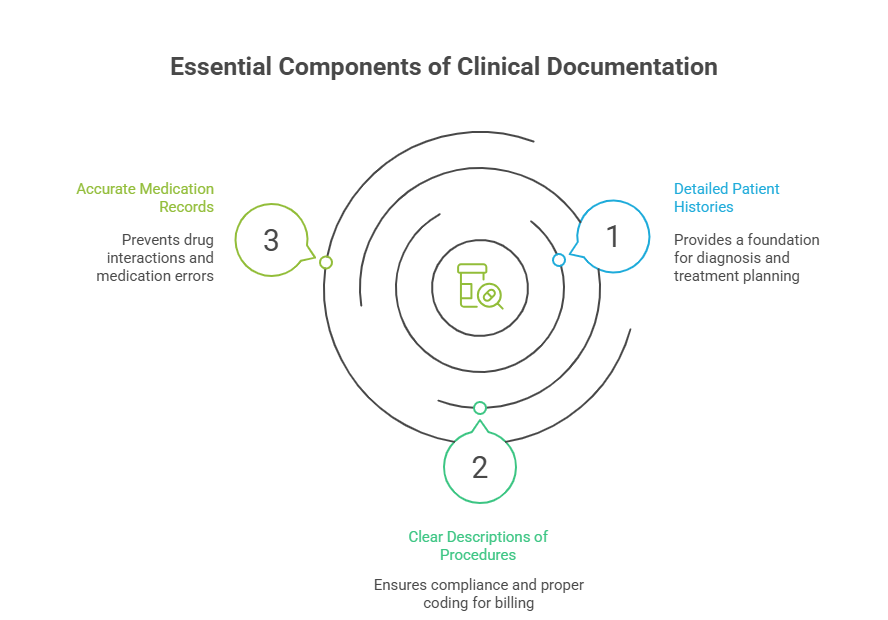
Key Elements of Clinical Documentation
Detailed Patient Histories and Medical Records
Accurate clinical documentation starts with a comprehensive and detailed patient history. This includes recording vital information such as medical conditions, past treatments, current medications, and family medical history. A well-documented patient history provides the foundation for diagnostic accuracy, treatment planning, and future care decisions.
By carefully documenting all relevant patient details, healthcare providers can ensure that each subsequent treatment decision is informed by a complete and accurate record of the patient's health journey. This comprehensive documentation is essential not only for ongoing care but also for regulatory compliance. It enables healthcare providers to track the progression of a patient’s condition and adjust treatment plans as needed. Patient histories should also be regularly updated to reflect new conditions, medications, or changes in the patient’s lifestyle to maintain the integrity and relevance of the medical record.
Clear and Concise Descriptions of Medical Procedures
Equally important to detailed patient histories is the documentation of medical procedures performed. Clear, concise descriptions of these procedures are critical for ensuring accurate coding, reimbursement, and legal protection. Every step of the procedure, including the rationale, technique, and any complications, should be recorded to ensure compliance with healthcare regulations and insurance requirements.
Inadequate documentation of procedures can lead to misunderstanding between healthcare providers, billing errors, or complications during audits. Additionally, a thorough description of procedures allows for continuity of care—ensuring that specialists, nurses, and other healthcare providers can easily understand the treatment performed and its outcomes. Well-documented procedures are also key to defending against potential legal claims and ensuring that the documentation aligns with clinical guidelines for best practices.
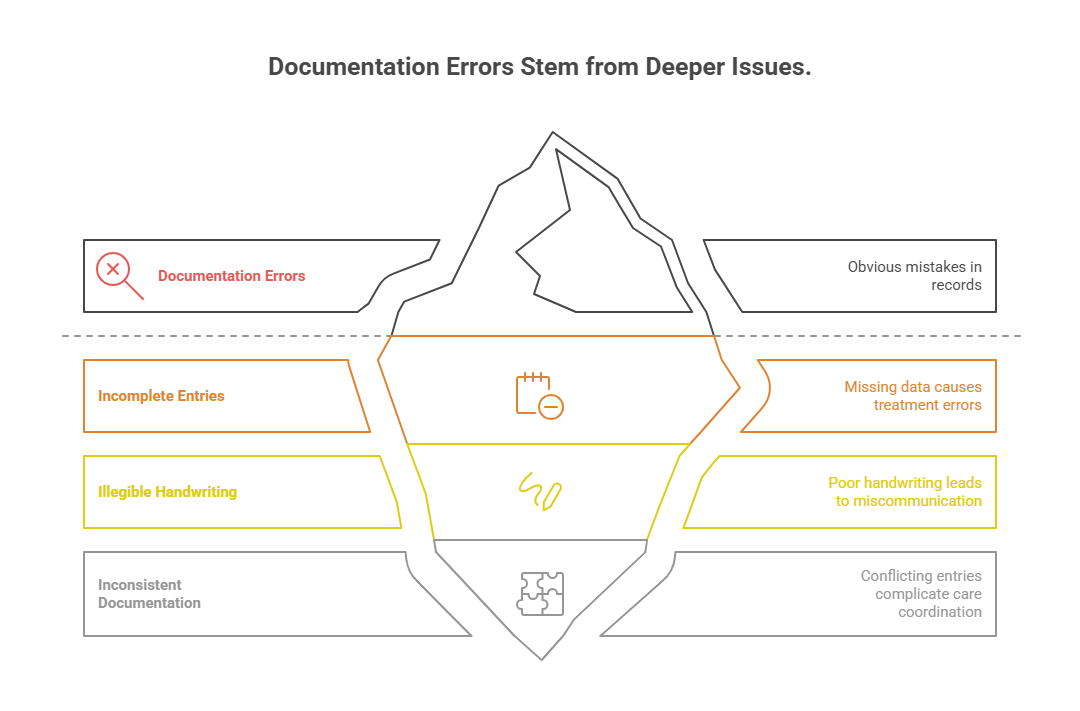
Common Pitfalls in Clinical Documentation
Incomplete or Illegible Entries
One of the most common issues in clinical documentation is incomplete or illegible entries. Healthcare providers sometimes overlook essential details or fail to record certain aspects of a patient’s condition or treatment. Missing information can lead to misdiagnoses, delayed treatment, and compromised patient safety. Additionally, illegible handwriting or poorly entered data can lead to misunderstandings among healthcare teams and reduced efficiency in care coordination.
To prevent these issues, providers should aim for clear, concise, and comprehensive documentation. Using Electronic Health Records (EHR) or digital platforms can greatly reduce the risk of illegibility, ensuring that all data is properly recorded and easily accessible by all involved in patient care. Implementing standardized templates for documenting patient information can also help reduce errors and ensure that no critical data is overlooked. Ensuring accuracy in documentation is a key element of patient safety and regulatory compliance.
Lack of Consistency in Documentation
Consistency is essential when it comes to clinical documentation. Providers should ensure that their documentation is consistent across different patients, procedures, and visits. Inconsistent entries can confuse healthcare teams, delay treatment, and even lead to errors in coding and billing. For instance, if a patient's diagnosis is documented differently in each visit, it can lead to discrepancies in patient care, incorrect treatment plans, and potential reimbursement issues.
To address this, healthcare professionals should follow consistent documentation practices for all aspects of care, from patient histories to procedural notes. Adopting standardized formats, utilizing structured templates, and ensuring proper training on documentation practices can reduce inconsistencies. Additionally, healthcare organizations should conduct regular audits to identify and correct any documentation inconsistencies. This ensures that patient care remains organized, coordinated, and accurate, which is vital for both patient outcomes and financial reimbursement.
Strategies for Improving Clinical Documentation Accuracy
Training and Education for Healthcare Providers
Ongoing training and education for healthcare providers are crucial to ensuring clinical documentation accuracy. As regulations evolve and documentation standards become more stringent, healthcare professionals must stay updated on best practices. Regular training ensures providers understand the importance of compliance, how to accurately document patient interactions, and the role their documentation plays in overall patient care.
Training should cover medical terminology, coding standards, and the use of electronic health record (EHR) systems. Additionally, training sessions should emphasize the importance of timely entries and legible handwriting, as well as the potential consequences of inaccurate documentation, such as denied claims, legal issues, or compromised patient safety. Providing healthcare providers with the tools and knowledge to document effectively will reduce errors, increase efficiency, and support higher quality patient outcomes.
Utilizing Technology to Enhance Accuracy
Advancements in health IT systems can significantly improve clinical documentation accuracy. One of the most effective tools in ensuring accurate documentation is the use of Electronic Health Records (EHRs). These systems facilitate real-time, standardized documentation that is legible, easily accessible, and shareable across the care team. EHRs help reduce common errors such as incomplete entries, illegible handwriting, and duplicated information.
Moreover, healthcare providers can use advanced voice recognition software to streamline documentation, allowing them to document patient interactions more quickly and accurately. Additionally, integrating clinical decision support tools with EHRs can provide real-time prompts for missing information, warnings for potential errors, and suggestions for improvement. By leveraging technology, healthcare organizations can ensure their documentation is consistent, timely, and aligned with the latest clinical guidelines, ultimately improving patient safety and care coordination.
Electronic Health Records (EHR) and Their Role in Accurate Documentation
How EHRs streamline and improve documentation practices
Electronic Health Records (EHRs) play a crucial role in enhancing the accuracy of clinical documentation by providing a digital platform for healthcare providers to record, store, and share patient information. EHRs streamline the documentation process by ensuring standardized data entry, easy access, and improved communication across care teams. With EHRs, providers can quickly enter and retrieve patient histories, diagnostic information, treatment plans, and medications, which increases both efficiency and accuracy.
EHRs also help reduce documentation errors related to legibility, as data is typed directly into the system rather than written by hand. This ensures that information is clear, concise, and easily readable by all healthcare professionals involved in patient care. Additionally, EHR systems are designed with built-in clinical decision support tools that can prompt providers for missing data, suggest appropriate codes, and flag potential inconsistencies, further ensuring the completeness and accuracy of clinical documentation.
Moreover, EHRs make it easier to comply with regulatory standards by providing a consistent format for documenting and storing patient information. They also facilitate easier audits and reporting of clinical data, helping healthcare organizations meet the standards set by organizations such as CMS and HIPAA. By automating workflows, EHRs free up healthcare professionals to focus more on patient care rather than spending time on administrative tasks, ultimately improving the overall quality of care provided.
How the Medical Billing and Coding Certification Prepares You for Accurate Clinical Documentation
The Medical Billing and Coding Certification plays a pivotal role in ensuring healthcare professionals have the necessary skills to maintain accurate clinical documentation. The certification program equips individuals with the knowledge required to accurately document patient information, including diagnoses, procedures, and medications. With the right training, professionals learn how to navigate the complex coding systems (ICD-10, CPT, HCPCS) and apply them to patient records, ensuring compliance and accuracy in clinical documentation.
Through this certification, students are also trained in Electronic Health Records (EHR) systems, which are integral to modern healthcare documentation. The program ensures that participants can confidently use EHR systems to record and retrieve patient data while minimizing data entry errors. This comprehensive training prepares billing and coding specialists to handle medical reports, insurance claims, and other essential documentation tasks efficiently, contributing to the accuracy and reliability of patient records.
Additionally, the Medical Billing and Coding Certification includes real-world case studies, enabling students to understand the practical application of clinical documentation and how it affects patient care and reimbursement. By completing this certification, professionals gain the expertise to enhance clinical workflows, reduce documentation errors, and comply with legal regulations governing patient records.
Frequently Asked Questions
-
The Medical Billing and Coding Certification is a credential that validates a healthcare professional's ability to accurately document patient diagnoses, treatments, and medical procedures. This certification is essential because it ensures that healthcare providers follow accurate coding and billing practices, which are crucial for compliance, proper reimbursement, and effective care coordination. Certified professionals help healthcare organizations avoid payment delays, denied claims, and legal liabilities by ensuring that all clinical documentation aligns with industry standards and regulatory requirements.
-
The Medical Billing and Coding Certification provides comprehensive training in medical terminology, ICD-10 coding, CPT codes, and HCPCS. This training ensures that professionals can accurately document patient diagnoses and medical procedures, which is critical for patient care, billing accuracy, and regulatory compliance. The program also emphasizes the importance of using Electronic Health Records (EHR) systems to ensure legibility, timeliness, and completeness of documentation. Graduates are equipped with the skills needed to reduce documentation errors and improve the overall quality of clinical records.
-
Accurate clinical documentation is essential for high-quality patient care. It ensures that healthcare providers have access to complete and reliable information about a patient's medical history, treatment plans, and medications. This reduces the risk of misdiagnoses, medication errors, and adverse reactions. Proper documentation also enhances care coordination, allowing all members of a healthcare team to collaborate effectively. Inaccurate or incomplete documentation, on the other hand, can lead to delayed treatments and potentially life-threatening mistakes, ultimately compromising patient safety.
-
Common challenges in clinical documentation include incomplete entries, illegible handwriting, and lack of consistency in documentation practices. These issues can lead to billing errors, miscommunication between healthcare providers, and reimbursement delays. To address these challenges, healthcare organizations should implement standardized documentation practices, utilize Electronic Health Records (EHRs), and provide ongoing training for healthcare providers. Additionally, ensuring that providers have access to real-time clinical decision support tools can help reduce errors and improve documentation quality.
-
Electronic Health Records (EHRs) play a crucial role in improving clinical documentation accuracy by providing a digital platform that reduces the risk of illegible handwriting and ensures timely documentation. EHR systems help standardize data entry, making it easier to record and share patient information across healthcare teams. EHRs also incorporate clinical decision support tools, which flag potential errors, missing data, or discrepancies in real-time. By using EHRs, healthcare providers can ensure accuracy, compliance, and better care coordination, ultimately improving patient outcomes and operational efficiency.
-
The key elements of clinical documentation include detailed patient histories, clear descriptions of medical procedures, and accurate coding of diagnoses and treatments. Healthcare providers should ensure that their documentation is complete, legible, and consistent. This includes recording vital patient information such as medications, allergies, diagnostic results, and treatment plans. Furthermore, providers should use standardized formats to enhance clarity and ensure that billing codes are applied accurately. Consistent, thorough documentation is essential for ensuring compliance, improving patient care, and securing appropriate reimbursement.
-
Regular training and education are crucial for improving clinical documentation accuracy. Healthcare providers need to stay updated on coding standards, regulatory changes, and the latest best practices in documentation. Training should cover areas like medical terminology, EHR usage, and legal and ethical documentation standards. By providing ongoing education to healthcare providers, organizations ensure that staff is well-prepared to meet documentation requirements and reduce errors. This enhances compliance, minimizes the risk of denied claims, and improves patient care.
Conclusion: Enhancing Clinical Documentation for Better Healthcare Outcomes
Accurate clinical documentation is essential for quality care, patient safety, and regulatory compliance. It ensures that healthcare providers have the information they need to make informed decisions, coordinate care effectively, and meet payment requirements under various reimbursement systems. Inaccurate documentation not only jeopardizes patient safety but can also lead to financial losses and legal complications.
By focusing on detailed patient histories, clear descriptions of procedures, and utilizing Electronic Health Records (EHRs), healthcare providers can significantly enhance the quality of their documentation. Training and education play a pivotal role in improving accuracy, ensuring that providers stay compliant with evolving standards and regulations. The Medical Billing and Coding Certification offers professionals the tools they need to succeed in this evolving field, providing them with the knowledge and skills to produce accurate, timely documentation that supports both patient care and organizational goals.
Through continuous improvement in documentation practices, healthcare organizations can achieve better clinical outcomes, improve patient satisfaction, and maintain financial stability.
Poll: What is the most challenging aspect of maintaining accurate clinical documentation?