Healthcare Cost Reporting Essentials for Billing Specialists
Accurate cost reporting in healthcare is essential for ensuring that healthcare providers receive proper reimbursement for services rendered. For billing specialists, mastering cost reporting means not only complying with regulations but also maximizing revenue and preventing financial setbacks. With Medicare, Medicaid, and private insurance reimbursements relying on these reports, any error can result in delayed payments or under-reimbursement, making precision crucial.
Billing specialists are tasked with gathering and reporting cost data, navigating complex regulatory requirements, and ensuring timely submission of reports. These professionals must stay up-to-date with evolving healthcare policies and maintain the accuracy of each report. By understanding the key components of cost reporting and the challenges they face, billing specialists can effectively manage financial data and ensure smooth operations. This guide outlines what makes healthcare cost reporting a critical aspect of billing operations and how it impacts the bottom line of healthcare practices.
Understanding Healthcare Cost Reporting
Key Components of Cost Reports
Healthcare cost reports are comprehensive documents that break down the expenses incurred by a healthcare provider. These reports typically include direct costs, such as medical supplies, labor expenses, and medication costs, as well as indirect costs like administrative overhead and facility maintenance. A critical part of the process is allocating costs appropriately between various services and departments, ensuring accuracy when reporting these figures.
Billing specialists are responsible for accurately categorizing these costs, ensuring that each report is aligned with accounting standards and regulatory requirements. Failure to properly allocate costs can result in reimbursement delays, penalties, or financial loss. Therefore, understanding the full scope of cost components and accurately reflecting them in the report is key for ensuring that healthcare providers are reimbursed for the services provided.
How Cost Reporting Affects Reimbursement
Cost reporting plays a significant role in healthcare reimbursement. Medicare, Medicaid, and private insurers use cost reports to determine how much they will reimburse providers for services rendered. The accurate reporting of costs ensures that healthcare providers receive appropriate reimbursement and maintain financial health. Underreporting or overreporting costs can lead to delayed payments, disputes, or fines.
Billing specialists must ensure that each line item of the cost report is backed by documentation and evidence, such as invoices, receipts, and payroll data. By presenting an accurate account of the costs, billing specialists can support reimbursement claims and avoid audit risks. Moreover, cost efficiency can be determined by comparing actual expenses to the expected rates for services, helping practices make strategic financial decisions that impact overall profitability.
Challenges Billing Specialists Face
Billing specialists face a variety of challenges when preparing cost reports. One of the most significant hurdles is navigating complex regulations set by government agencies and private insurers. Medicare and Medicaid have specific rules for how costs should be categorized and reported, and billing specialists must stay current on any changes to these regulations. Missing these updates can result in non-compliance, penalties, and lost revenue for the healthcare practice.
Another challenge is ensuring data accuracy. Healthcare providers often deal with large volumes of data, and the sheer complexity of the cost reporting process can lead to errors in cost allocation or data entry. Inaccurate reporting may trigger audits or denied reimbursements, leading to delays in payments. Additionally, healthcare cost reporting often involves multiple stakeholders, making coordination between departments, providers, and insurance companies essential. The ability to manage large datasets while maintaining compliance and accuracy is a constant challenge for billing specialists.
Salary and Career Advancement Outlook
Median Salary & High-Paying Markets
The median salary for professionals in healthcare billing can vary depending on location, experience, and specialization. Billing specialists in major metropolitan areas often earn more due to the higher cost of living and the demand for skilled professionals. On average, the median salary for a medical billing specialist ranges from $40,000 to $55,000 annually. However, high-paying markets like California, New York, and Texas offer opportunities for professionals to earn upwards of $60,000 or more, depending on their role and experience level.
Specialized roles, such as medical coding auditor, compliance officer, or billing specialists working in oncology, cardiology, or orthopedics, can command higher salaries due to the complexity and specialization required. With industry growth and the demand for skilled professionals in healthcare, billing specialists have a high potential for salary increases as they gain experience and specialized knowledge.
Promotion Timelines by Organization Size
Promotion timelines for medical billing specialists often depend on the size and structure of the organization they work for. In smaller practices or private offices, career advancement may take less time, and professionals may be able to move into higher positions like office manager or billing supervisor in 1-3 years.
In larger organizations or hospital systems, the promotion timeline may be longer, often requiring 3-5 years of experience before moving into managerial positions such as billing coordinator, compliance manager, or revenue cycle manager. The opportunities for advancement can also be impacted by the size of the team, the complexity of billing operations, and the individual’s ability to take on additional responsibilities or leadership roles.
For those seeking rapid career advancement, it’s advisable to continuously update certifications and stay knowledgeable about changes in coding systems, billing regulations, and healthcare policies to remain competitive in the job market.
| Factor | Description |
|---|---|
| Median Salary | The average salary for billing specialists ranges from $40,000 to $55,000 annually. High-paying markets offer $60,000+. |
| High-Paying Markets | Billing specialists in areas like California, New York, and Texas earn higher salaries due to the cost of living and high demand. |
| Specialized Roles | Specialists in oncology, cardiology, and orthopedics can earn higher salaries due to the complexity of the work. |
| Promotion Timeline (Small Practices) | In smaller organizations, professionals can expect to move into higher roles like office manager or billing supervisor in 1–3 years. |
| Promotion Timeline (Large Organizations) | In larger organizations, it typically takes 3–5 years to advance into roles like billing coordinator or revenue cycle manager. |
CMS Guidelines for Healthcare Cost Reporting
Medicare and Medicaid Requirements
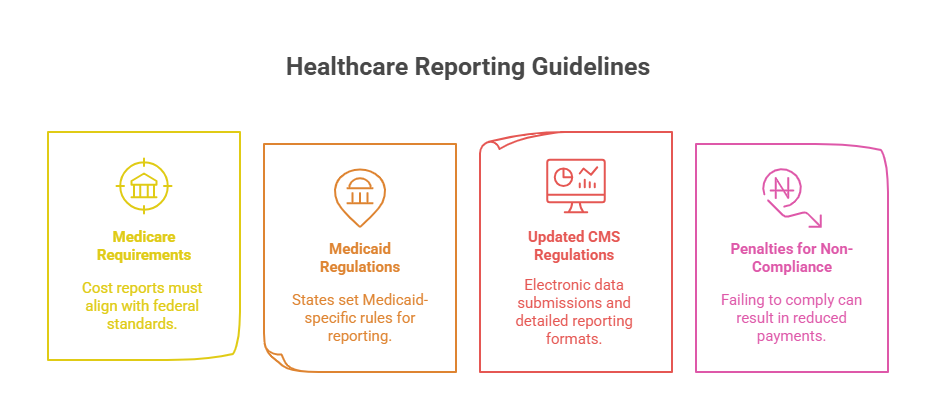
Medicare and Medicaid are two of the largest payers in the U.S. healthcare system, and they each have specific cost reporting requirements for healthcare providers. Medicare cost reports are used to determine the reimbursement rates for healthcare services provided to eligible patients. Billing specialists must accurately report all expenses, including both direct and indirect costs, to ensure providers receive the correct reimbursement.
Medicaid, while similar, has its own set of guidelines, which can vary by state. Medicaid reimbursements are generally based on cost-based reimbursement systems or prospective payment systems (PPS). These systems require billing specialists to break down expenses by service categories and submit detailed reports on utilization rates, patient demographics, and cost allocations. Ensuring compliance with state-specific Medicaid rules is critical to avoid discrepancies in payment.
In both systems, it’s essential that billing specialists follow the proper cost allocation methods, such as cost centers, and understand allowed expenses under Medicare and Medicaid coverage. By doing so, they prevent underpayments or disallowed claims, thereby securing accurate and timely reimbursement for services.
What’s New in 2025 CMS Regulations
In 2025, the Centers for Medicare & Medicaid Services (CMS) is implementing several updates to cost reporting regulations. These updates include changes to the Medicare cost report forms, with a stronger focus on standardizing data submission to streamline the reporting process. One of the most significant changes is the expanded use of electronic data submission, making it easier to track discrepancies and reducing the risk of human error during reporting.
Additionally, CMS is introducing a more detailed breakdown of cost categories, with increased transparency requirements for how funds are allocated across different services. Billing specialists must be prepared to report costs with greater granularity, detailing labor costs, service utilization, and even patient care costs related to specific treatments or procedures. This move is aimed at making the reimbursement process more equitable and transparent.
As a result, billing specialists will need to stay informed about these regulatory changes and ensure that their healthcare organizations adapt to new CMS rules. Keeping up-to-date with these changes is crucial for avoiding penalties and ensuring that providers remain eligible for maximum reimbursement.
Penalties for Non-Compliance
Non-compliance with CMS cost reporting requirements can result in severe financial consequences. Failure to submit accurate cost reports or meet CMS deadlines can lead to reimbursement reductions, denial of claims, or even audits that result in penalties. In some cases, healthcare providers may face disqualification from receiving Medicare or Medicaid payments until the issue is resolved.
Billing specialists must also be vigilant about reporting unallowable costs—costs that do not meet CMS standards. If these costs are included in the report, the provider may face fines or disallowance of payments. Additionally, improper allocation of expenses can lead to audits, where providers are asked to return funds they received based on inaccurate reports.
To avoid these risks, it’s essential for billing specialists to double-check all data entries, ensure that cost categories are correctly classified, and that all supporting documentation is accurate and accessible. Compliance also involves maintaining thorough records that can be easily retrieved during audits or for any required follow-up actions.
Tools for Accurate Cost Reporting
EHR and Billing System Integration
Integrating Electronic Health Records (EHR) with billing systems is crucial for ensuring the accuracy of healthcare cost reporting. EHR systems store detailed patient information, including diagnosis codes, treatment plans, and billing codes associated with services rendered. When integrated with billing systems, cost data flows seamlessly from the clinical side to the financial side, reducing the risk of errors caused by manual data entry.
Billing specialists rely on this integration to automatically pull cost data from the EHR and ensure that it aligns with insurance claims and Medicare/Medicaid requirements. By connecting EHR systems with billing software, specialists can avoid duplicate data entries, minimize coding errors, and ensure that reimbursement claims are filed correctly. This seamless connection between clinical documentation and billing systems also enhances data accuracy, improves efficiency, and reduces the chances of payment delays caused by administrative mistakes.
Automating Cost Reporting Processes
Automating cost reporting processes is a game-changer for billing specialists who manage large volumes of data. Automation tools allow for the streamlined collection of cost data, categorization, and submission, significantly reducing the amount of time spent on manual reporting. By using automated cost reporting software, billing specialists can automatically generate reports based on pre-set parameters, which are consistent with the latest CMS regulations.
Automating processes also ensures timeliness by setting reminders for report submission deadlines, which helps avoid penalties for late filing. Additionally, it ensures that reports are always up-to-date, making it easier to track ongoing healthcare expenses and adjust for any changes in Medicare or Medicaid rules. Automation also helps in forecasting costs, providing healthcare providers with better financial visibility, and aiding in strategic decision-making for long-term sustainability.
Software Solutions That Can Help
There are numerous software solutions that can assist billing specialists in accurately preparing cost reports. Some of the most widely used systems for cost reporting include:
Epic Systems: A widely adopted EHR system that integrates seamlessly with billing tools to ensure accurate cost allocation and billing code usage.
Cerner: Another popular EHR platform that enables healthcare providers to efficiently manage cost data and comply with Medicare/Medicaid regulations.
TruBridge: Specializes in providing cost reporting tools for healthcare providers that integrate financial data from various sources, making it easier to generate accurate and timely reports.
3M Health Information Systems: Offers specialized coding software and cost reporting tools that help billing specialists manage clinical documentation and billing processes more efficiently.
HMS (Health Management Systems): Provides a comprehensive suite of software for managing claims processing, cost reporting, and insurance verification, offering a complete end-to-end solution.
These tools are designed to reduce manual errors, improve efficiency, and ensure compliance with both federal and state guidelines. By leveraging these solutions, billing specialists can maximize productivity while ensuring the accuracy and integrity of their cost reports, reducing the risk of financial discrepancies and compliance issues.
| Tool | Description |
|---|---|
| EHR Integration | Integrating Electronic Health Records with billing systems for accurate cost tracking, ensuring seamless data flow between clinical and financial operations. |
| Billing Software | Specialized software for managing billing codes, cost reports, and reimbursement claims, helping to streamline the cost reporting process and reduce errors. |
| Automated Reporting Tools | Automation tools for generating timely, accurate reports to reduce manual errors and ensure cost data is updated in real-time. |
| Data Analytics Solutions | Tools for analyzing cost trends and forecasting future expenses, allowing healthcare providers to optimize their budgeting and reporting strategies. |
Best Practices for Billing Specialists
Keeping Up with Regulatory Changes
One of the primary challenges billing specialists face is staying current with healthcare regulations. CMS guidelines, Medicare, Medicaid, and private insurance providers are constantly updating their policies, and it’s crucial for billing specialists to stay informed about these changes. Regulatory updates can affect everything from cost reporting requirements to reimbursement rates, and failing to comply with the latest rules can result in penalties, denied claims, or under-reimbursement.
Billing specialists should subscribe to industry newsletters, attend webinars, and participate in professional development opportunities to keep their knowledge up to date. Regular training ensures that they are always familiar with new regulations, such as changes to coding systems, claim submission processes, and cost allocation methods. By remaining proactive and continuously educating themselves, billing specialists can avoid compliance issues and maintain the integrity of their reports.
Ensuring Data Accuracy and Timeliness
The accuracy of healthcare cost reports depends on timely and precise data entry. Billing specialists must ensure that patient information is correctly entered into the EHR system, that billing codes are accurately assigned, and that cost data is properly allocated. One error in data entry can cause a ripple effect, leading to incorrect reimbursements, audit risks, or delays in payments.
To ensure data accuracy, billing specialists should use double-checking protocols and automated tools to cross-reference cost data before submission. They should also establish a system for tracking report deadlines and consistently review data to ensure timeliness. Keeping accurate and up-to-date records is vital for maintaining a steady cash flow for healthcare providers and avoiding financial discrepancies.
Managing Multiple Reporting Streams
Billing specialists often deal with multiple reporting streams, including Medicare, Medicaid, and private insurance reimbursements, all of which have different cost reporting requirements. Managing these diverse reporting systems can be complex, but it’s necessary to ensure compliance and timely reimbursement.
One of the best practices for managing multiple reporting streams is to automate as much as possible. Using specialized software can help streamline the cost reporting process, ensuring that billing data is automatically transferred across systems, reducing manual errors. Billing specialists should also establish clear workflows for each reporting stream, ensuring that they can easily track progress, flag discrepancies, and address any issues in real-time. Being organized and managing multiple streams with a systematic approach ensures that billing specialists can handle increased workload and maintain report accuracy across the board
How Our Medical Billing and Coding Certification by AMBCI Helps
Practical Application of Reporting Skills
Our Medical Billing and Coding Certification by AMBCI offers practical, hands-on experience that ensures you’re fully prepared for real-world cost reporting tasks. Throughout the course, you’ll gain a deep understanding of the regulatory framework that governs healthcare billing, including Medicare, Medicaid, and private insurance requirements. You'll also learn how to handle complex cost reporting scenarios, apply accurate coding systems, and manage cost data effectively. By working on real-world examples, you'll understand how to navigate the complexities of healthcare billing, ensuring accuracy and timeliness in reporting.
Additionally, the certification provides you with a solid foundation in using EHR systems, billing software, and cost-reporting tools, which are essential for integrating data across different healthcare platforms. This practical experience ensures that once you complete the certification, you’re equipped with the skills to handle cost reports and meet industry standards confidently.
Real-World Case Studies in Training
In our Medical Billing and Coding Certification by AMBCI, we provide real-world case studies that simulate the challenges you will face as a billing specialist. These case studies offer you a chance to apply the skills you’ve learned to solve actual billing problems, including discrepancies in cost reporting, coding errors, and compliance issues. By working through these case studies, you will gain hands-on experience in managing multiple reporting streams, interacting with payers, and ensuring accuracy in cost reporting submissions.
Additionally, you will engage in scenario-based exercises where you’ll practice handling complex billing situations, such as denied claims, under-reimbursement, or disallowed costs. This approach gives you the confidence and real-world readiness to thrive in the fast-paced environment of healthcare billing. The Medical Billing and Coding Certification by AMBCI equips you with the practical tools to hit the ground running and drive better outcomes for healthcare providers.
Frequently Asked Questions
-
The Medical Billing and Coding Certification by AMBCI provides in-depth training on key aspects of medical billing, including EHR integration, coding systems (CPT, ICD-10), and cost reporting. The program also covers Medicare and Medicaid regulations, insurance claim processes, and the use of billing software to ensure accuracy and timeliness. Additionally, the certification program includes real-world case studies, practical assignments, and scenario-based exercises that simulate real-life challenges in medical billing. By completing the program, you will be equipped to handle both basic and complex billing tasks, ensuring you're ready to excel in the healthcare administration field.
-
The Medical Billing and Coding Certification by AMBCI provides a solid foundation for a career in healthcare administration. With this certification, you can pursue roles such as medical office manager, billing specialist, and coding technician. The program’s focus on practical coding applications and cost reporting ensures you're equipped with skills that are in demand in healthcare settings. Additionally, by gaining expertise in Medicare and Medicaid regulations, you’re positioned for career advancement, especially in specialized healthcare sectors such as oncology or pediatrics. Having a recognized certification increases your employability, helps secure higher-paying positions, and supports your professional growth within the healthcare industry.
-
The Medical Billing and Coding Certification by AMBCI is designed for flexibility and can typically be completed in 4 to 6 weeks depending on whether you study full-time or part-time. The program includes online modules, which allow you to learn at your own pace. You’ll engage in practical assignments, case studies, and interactive lessons, ensuring that you grasp key concepts before moving on to the next level. Upon completion, you’ll be fully equipped to take the certification exam and begin applying for jobs in healthcare administration, making the certification a quick and effective way to launch or enhance your career.
-
After completing the Medical Billing and Coding Certification by AMBCI, you will be qualified for a range of entry-level and advanced roles in healthcare billing and administration. Job opportunities include positions such as medical office assistant, coding specialist, patient services representative, medical biller, and claims processor. As you gain experience, you can advance to roles like billing manager, practice coordinator, or office manager. The certification also opens doors to specialized areas like healthcare reimbursement, insurance billing, and medical auditing. With the healthcare industry continually expanding, the demand for certified professionals is high, and your certification will help you secure a competitive edge in the job market.
-
The Medical Billing and Coding Certification by AMBCI incorporates real-world case studies and practical exercises that simulate actual billing situations, allowing you to apply your skills in realistic settings. These exercises include handling complex coding issues, denied claims, and insurance discrepancies that you may encounter in the workplace. By completing these tasks, you will build the confidence and experience needed to handle real-world challenges. The program also emphasizes regulatory compliance and provides hands-on experience with billing software, ensuring that you’re fully prepared to navigate the complexities of healthcare cost reporting and billing processes effectively.
-
Preparing for the Medical Billing and Coding Certification by AMBCI exam involves a mix of study materials, including interactive lessons, practice quizzes, and hands-on exercises. The program provides you with comprehensive study guides, which cover essential topics like CPT coding, ICD-10 coding, billing cycles, and cost reporting techniques. We also offer mock exams and review sessions to help reinforce key concepts and assess your readiness for the final exam. With these resources, you can ensure that you're fully prepared to pass the exam and begin your career as a certified medical billing and coding professional.
-
Upon earning the Medical Billing and Coding Certification by AMBCI, you can work in various healthcare settings, including hospitals, clinics, private practices, and telehealth offices. Additionally, specialized healthcare fields such as oncology, cardiology, dentistry, and pediatrics also require billing specialists with knowledge of specific coding and reporting processes. The certification prepares you to handle general billing tasks as well as the more complex billing processes in specialized medical fields, where accurate cost reporting is essential. With flexible job opportunities in a variety of healthcare settings, this certification opens doors to multiple career paths.
The Take Away
The Medical Billing and Coding Certification by AMBCI is a powerful step toward advancing your career in the healthcare industry. With comprehensive training in coding systems, cost reporting, and insurance billing, this certification prepares you for the challenges and demands of the healthcare billing sector. Through real-world case studies, practical exercises, and hands-on tools, you’ll gain the confidence and expertise needed to excel in billing roles across various healthcare settings.
This certification not only improves your job prospects but also positions you for career advancement and higher salary potential. By mastering Medicare, Medicaid, and private insurance requirements, you’ll be equipped to handle the complex billing processes in any healthcare practice. Whether you’re just starting or looking to specialize further, the AMBCI Medical Billing and Coding Certification offers the foundational skills and real-world knowledge that will set you apart in a competitive job market.
Start your journey today and equip yourself with the expertise to navigate the dynamic world of healthcare billing and coding.
Poll: What aspect of healthcare cost reporting do you find most challenging?