Medical Billing and Coding Certification in North Dakota: Complete Guide for 2025–2026
North Dakota’s care network—from Fargo’s tertiary centers to Minot’s community clinics—runs on accurate claims, fast denial resolution, and airtight compliance. Employers increasingly filter applicants by medical billing and coding certification, favoring candidates who hit ≥96% clean-claim rates and understand payer logic end-to-end. This guide gives you a practical, North Dakota–specific playbook: market demand, salaries, training routes, AMBCI exam tactics, interview expectations, and a 6-week study plan. For regional context, we also reference neighbor state benchmarks—compare workflows in South Dakota, growth arcs in Minnesota, hybrid hiring in Wisconsin, and remote pipelines in Washington.
1) North Dakota’s Hiring Climate & Why Certification Matters
North Dakota’s billing ecosystem depends on coders who can translate documentation into revenue with precision. Health systems (Sanford Health, Essentia Health, Altru) and multi-site physician groups now shortlist credentialed candidates who demonstrate ICD-10-CM structure, CPT®/HCPCS mastery, and payer-specific edit control. Certification via AMBCI proves you can read EOBs accurately, apply modifier logic (25/59/57), and defend claims on appeal—core skills mirrored in nearby markets like Montana/Wyoming corridors, metro hubs across Michigan, and payer-dense regions of Pennsylvania. For telehealth workflows, compare edits and job models seen in Oregon to anticipate remote policy shifts.
North Dakota Medical Billing & Coding — 2025–2026 Salary, Skills & Market Outlook
2) Training Routes & Fastest Certification Pathways
Start with a high-school diploma/GED, then enroll in an AMBCI-aligned program that integrates terminology, anatomy, ICD-10-CM coding, CPT®/HCPCS procedure mapping, and claim lifecycle management. North Dakota candidates typically finish in 4–6 months using hybrid or fully online cohorts—mirroring accelerated formats documented in Utah’s remote programs and cohort pacing seen in Indiana’s externship model. To compare placement metrics, look at outcomes tracked in Iowa and program design ideas from Colorado.
Program features to insist on (for ND employers):
Mock audits & denial labs using CO-16/CO-97/PR-204 scenarios (benchmarked against Illinois’s metropolitan payer mix).
Modifier mastery (25/59/57) reinforced with multi-discipline cases like E/M, ortho, telehealth—similar to labs highlighted in Massachusetts.
EHR fluency (Epic/eCW/Cerner) and claim-edit simulators aligned with payer edits—approaches you’ll also see in Virginia’s audit prep and Maryland’s compliance tracks.
AMBCI exam workshops and resume clinics modeled after Pennsylvania’s hiring playbook.
3) Salary Growth, Remote Roles & Regional Mobility
Certified ND billers average ~$52–53K, with senior coders surpassing $70K as case complexity rises. Fargo and Bismarck trend higher due to multi-facility networks and payer diversity; Grand Forks and Minot climb quickly with telehealth expansion. To pressure-test your earnings path, compare urban deltas in Michigan, remote-first roles in Oregon, and blended teams in Kansas.
Career accelerators that ND employers reward:
A personal metrics sheet (clean-claim %, claims/hour, A/R days)—an interview staple also emphasized in Tennessee.
Portfolio cases (inpatient, outpatient, telehealth) with before/after denial corrections—mirroring documentation styles used in South Carolina.
Payer-policy tracking habits (CMS bulletins, MUE/NCCI edits) comparable to lasting habits taught in Washington.
Quick Poll: What’s Your Biggest Challenge in Medical Billing?
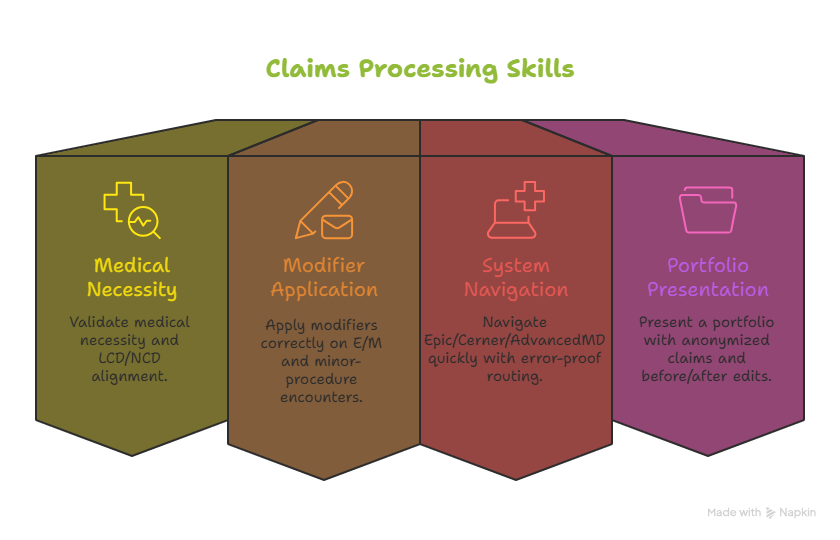
4) Skills North Dakota Employers Test (and How to Prove Them)
Hiring teams assess applied skill, not theory. Expect case tests on CO-16 (information missing), CO-97 (bundling), and PR-204 (non-covered). Demonstrate the ability to:
Validate medical necessity and LCD/NCD alignment (a staple in Massachusetts’s compliance hubs).
Apply modifiers correctly on E/M and minor-procedure encounters (benchmarks echoed in Florida’s high-volume clinics).
Navigate Epic/Cerner/AdvancedMD quickly with error-proof routing—habits seen in Pennsylvania’s enterprise rollouts.
Present a portfolio: three anonymized claims (inpatient, outpatient, telehealth) with before/after edits—an approach mirrored in Wisconsin’s remote network.
To sharpen appeals, study templates popular in Maryland and denial-tracking cadence used in South Dakota. ND recruiters love candidates who can speak in metrics: “Reduced A/R from 52 to 34 days,” or “Sustained 98% coding accuracy over 1,200 monthly claims.”
5) AMBCI Exam Blueprint & 6-Week Study Plan
The AMBCI exam validates practical billing/coding competency with scenario-based items. Use this 6-week sprint that ND candidates report as the most efficient:
Week 1 – ICD-10-CM structure + payer edits: Map diagnoses to medical necessity; cross-reference edits patterns from Arizona’s outpatient mix.
Week 2 – CPT®/HCPCS + modifiers: Practice common E/M, ortho, derm, and telehealth examples; compare modifier policies seen in California’s large networks.
Week 3 – Claims lifecycle & reconciliation: Build muscle memory in ERA/EOB posting using workflows echoed in Virginia.
Week 4 – Mock exams (timed): Two full simulations; target ≥85% before moving on—compare pacing insights from Oregon’s remote cohorts.
Week 5 – Denials & appeals: Build templates for CO-16/CO-97/PR-204; adapt examples used in Tennessee.
Week 6 – Portfolio + job search: Prepare metrics-rich resume; target ND systems first, then remote employers—study placement patterns in Washington and Pennsylvania.
Pro tip: Keep a live Denial Intelligence Sheet—a single spreadsheet where you log denial code, root cause, fix, and turnaround time. This is the fastest way to improve scores and impress hiring managers.
6) FAQs — North Dakota Medical Billing & Coding (2025–2026)
-
-
Yes—AMBCI is recognized in major systems and by national RCM vendors, just as it is across Wisconsin and Oregon.
-
Absolutely—remote hiring has scaled statewide, with patterns similar to South Dakota’s telehealth ecosystem.
-
Entry ranges ~$35–39K, with certified roles quickly rising past $50K. Compare ladders with Kansas and Pennsylvania.
-
Focus on Epic, Cerner, and AdvancedMD—a trio common across ND and also prevalent in Washington.
-
CO-16 (information missing), CO-97 (bundled), PR-204 (non-covered). Denial correction playbooks in South Carolina are a solid practice reference.
-
Bring a mini-portfolio with three anonymized claims and a metrics sheet—methods echoed across Tennessee and Oregon. -
Yes—many AMBCI grads move into auditor, coding lead, or revenue integrity positions within 24–36 months, mirroring growth tracks seen in Virginia.