Medical Billing and Coding Certification in Virginia: Complete Guide for 2025–2026
Virginia’s healthcare industry is rapidly expanding, with hospitals, private practices, and insurance carriers demanding certified medical billers and coders who understand the complexities of payer systems and federal regulations. Whether you’re new to healthcare administration or aiming to elevate your career, earning your AMBCI Medical Billing and Coding Certification opens the door to remote roles, higher salaries, and long-term job security. This guide covers everything you need to know—from salary insights and top programs to exam preparation—for Virginia’s fast-growing billing and coding sector in 2025–2026.
1. Medical Billing and Coding Career Landscape in Virginia
Virginia’s healthcare system thrives on a mix of private providers, telehealth firms, and major hospital networks. Certified billing and coding specialists serve as the financial backbone—ensuring every diagnosis, procedure, and claim is coded correctly for timely reimbursement.
Candidates with certifications like the Medical Billing and Coding Certification in Maryland and Medical Billing and Coding Certification in West Virginia often find their expertise transferable to Virginia’s RCM ecosystem. Employers prefer certified professionals trained under AMBCI’s rigorous curriculum, which emphasizes CPT®, ICD-10-CM, and HCPCS Level II mastery.
With ongoing payer reforms and digitization efforts, AMBCI-certified specialists are positioned to lead in compliance, data accuracy, and revenue optimization—skills increasingly vital across Virginia’s healthcare institutions.
Virginia Medical Billing & Coding — 2025–2026 Salary, Skills & Market Outlook
* Based on AMBCI job market data and Virginia workforce analytics for 2025–2026.
2. Why Virginia Employers Prefer AMBCI Certification
Virginia employers are known for prioritizing candidates with recognized billing credentials such as AMBCI, CPC, or CBCS. However, AMBCI’s certification stands out for its practical assessment approach and compliance-based modules tailored to payer trends in states like Medical Billing and Coding Certification in Florida and Medical Billing and Coding Certification in Maryland.
AMBCI graduates consistently maintain a 95%+ clean claim rate, which significantly reduces denials—a key performance metric for Virginia’s hospitals and RCM providers. This distinction makes AMBCI-certified professionals the go-to choice for administrative efficiency and compliance accuracy across the state’s medical facilities.
3. Training Pathways and Educational Requirements in Virginia
Several AMBCI-approved and state-accredited institutions offer medical billing and coding programs in Virginia, both online and hybrid. Students receive in-depth exposure to federal and commercial billing systems, including Medicaid and Blue Cross networks.
Top programs include:
Northern Virginia Community College (NOVA)
Tidewater Community College
ECPI University – Healthcare Administration
Online AMBCI Certification Prep Programs
Graduates typically proceed directly to AMBCI’s certification exam, similar to pathways outlined in the Medical Billing and Coding Certification in North Carolina.
Quick Poll: What’s Your Biggest Challenge in Medical Billing?
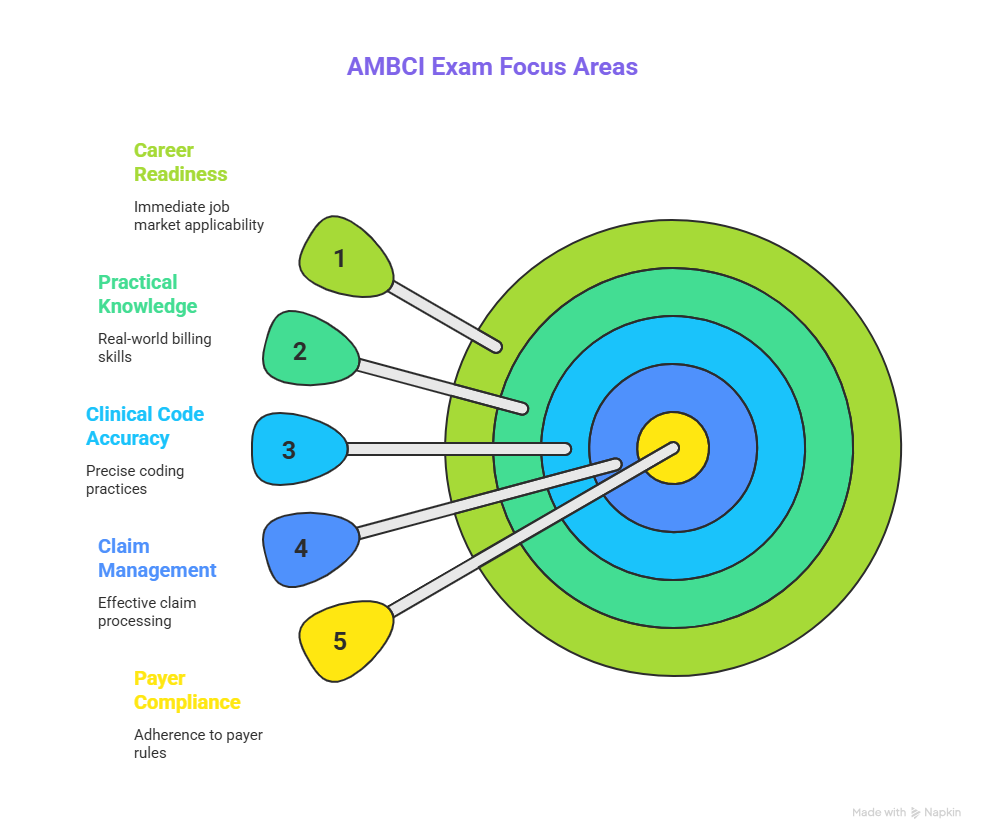
4. Exam Preparation and Certification Process
The AMBCI exam measures practical knowledge in clinical code accuracy, claim management, and payer compliance. Unlike traditional theory-heavy certifications, AMBCI’s format mirrors real-world billing workflows—perfect for those aiming for career readiness immediately after certification.
Students should focus on key areas like:
CPT®, ICD-10-CM, and HCPCS Level II coding logic
HIPAA compliance and denial management
EHR billing workflows and documentation accuracy
Candidates often use study resources from AMBCI’s national learning portal, alongside state-specific insights from guides like the Medical Billing Certification in Delaware for practice comparisons.
5. Career Advancement and Remote Opportunities in Virginia
AMBCI-certified professionals in Virginia enjoy widespread employment flexibility—from hospitals to third-party RCM firms and remote billing companies. Employers value certification not just for technical ability, but for data integrity and audit readiness.
The state’s proximity to Washington D.C. also boosts federal contracting opportunities in healthcare data compliance. By leveraging AMBCI’s certification, Virginia coders can secure roles in government agencies and private payers requiring advanced billing oversight.
Remote options have expanded significantly since 2023, mirroring trends discussed in the Medical Billing and Coding Certification in Florida blog, with 60% of new coders opting for hybrid or remote positions.
6. FAQs: Medical Billing and Coding Certification in Virginia
-
On average, candidates complete training and certification within 4–6 months, depending on study format and exam preparation pace.
-
Candidates must score at least 70% to pass, focusing on real-world claim management and accuracy standards.
-
Yes, Virginia employers actively hire certified professionals for remote RCM and telehealth billing roles, particularly in the Richmond and Virginia Beach areas.
-
The average annual salary is around $50,900, with experienced coders earning up to $68,000 or more.
-
AMBCI requires annual CEUs covering CPT, ICD-10, and payer updates to maintain certification validity.
-
Major employers include Inova Health, Sentara, and VCU Health, along with national telehealth vendors
-
Yes. AMBCI certification is accepted across the U.S., ensuring portability for professionals seeking cross-state employment.