Medical Billing and Coding Certification in Vermont: Complete Guide for 2025-2026
Vermont’s healthcare sector is small but thriving—especially in hospital billing, telehealth management, and private practice administration. The state’s ongoing adoption of digital health systems has created an urgent need for certified medical billers and coders who can handle complex payer workflows and compliance demands.
The AMBCI Medical Billing and Coding Certification equips Vermont professionals with in-demand coding precision, claims management expertise, and compliance fluency—skills that hospitals and insurance networks rely on for revenue accuracy. This guide unpacks everything you need to know about salary ranges, certification requirements, exam prep, and real job opportunities across Vermont in 2025–2026.
1. Medical Billing and Coding Career Landscape in Vermont
Vermont’s healthcare economy is driven by organizations like the University of Vermont Medical Center, Copley Hospital, and Rutland Regional Health. Billing and coding specialists are the data translators of this ecosystem, ensuring that every procedure and diagnosis aligns with correct CPT® and ICD-10-CM codes for proper insurance payment.
Like the growing career market seen in Medical Billing and Coding Certification in New Hampshire and Medical Billing and Coding Certification in Maine, Vermont’s professionals can expect similar upward mobility and flexibility. The demand for remote-ready billing experts has expanded through AMBCI-certified pipelines, with many coders now supporting multi-state payer systems.
Vermont Medical Billing & Coding — 2025–2026 Salary, Skills & Job Outlook
* Benchmarks reflect typical employer targets and Vermont market snapshots for 2025–2026.
2. Why AMBCI Certification Is Vital for Vermont’s Healthcare Economy
AMBCI-certified coders are recognized for producing audit-ready, compliant, and high-accuracy claims, significantly improving payer approval rates. In Vermont, where healthcare budgets are tight and staff turnover is common, certified coders ensure financial continuity.
Much like professionals trained under Medical Billing and Coding Certification in Massachusetts and Medical Billing and Coding Certification in Connecticut, Vermont graduates stand out for their accuracy and regulatory literacy.
Key benefits of AMBCI certification include:
Access to nationwide job listings
Practical training modules that reflect real insurance workflows
Cross-state license recognition
Continuing education through live policy updates
3. How to Become Certified in Vermont
The AMBCI pathway begins with structured online coursework covering medical terminology, coding systems, and electronic health record (EHR) procedures. Upon completion, students sit for the AMBCI certification exam, which emphasizes real-world billing and compliance scenarios.
Vermont candidates can prepare through:
Local colleges offering hybrid billing programs
AMBCI’s online portal with instructor-led prep
Practice tests modeled on actual claim case studies
Graduates then apply their training to settings like community hospitals or remote RCM teams, similar to peers completing the Medical Billing and Coding Certification in New York who often transition directly into national healthcare networks.
Quick Poll: What’s Your Biggest Challenge in Medical Billing?
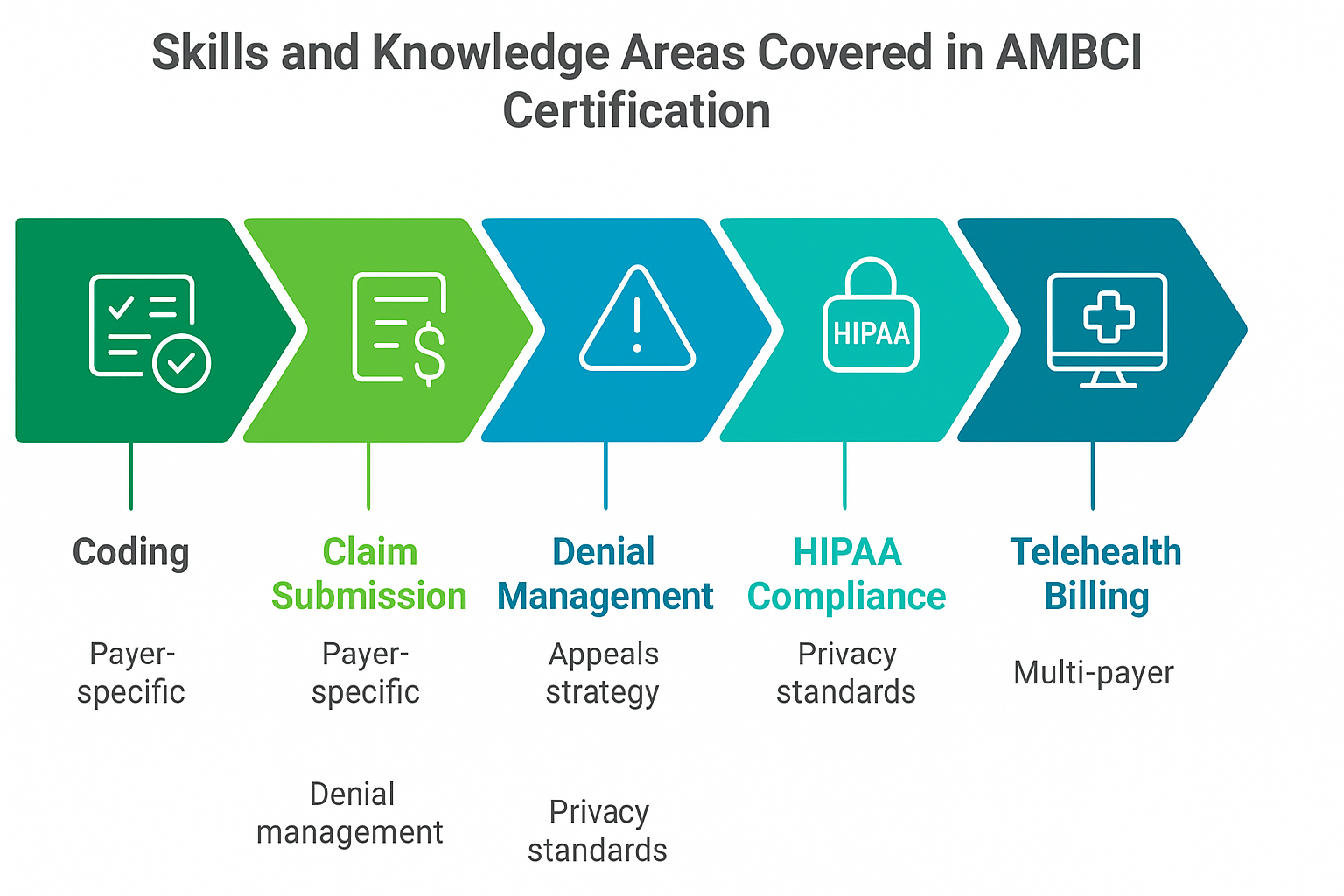
4. Skills and Knowledge Areas Covered in AMBCI Certification
AMBCI’s curriculum aligns with Vermont’s healthcare standards and payer mix. Certified professionals develop expertise in:
CPT®, ICD-10-CM, and HCPCS Level II coding
Payer-specific claim submission
Denial management and appeals strategy
HIPAA compliance and privacy standards
Telehealth billing across multi-payer systems
Professionals trained under AMBCI show superior first-pass claim success rates compared to peers trained via outdated programs. As outlined in Medical Billing and Coding Certification in Rhode Island, mastering EHR workflows and automation tools is also a strong advantage.
5. Career Opportunities and Salary Growth in Vermont
Vermont’s medical billing professionals are seeing consistent pay increases as smaller clinics compete with larger networks for certified staff. Entry-level roles often lead to positions in compliance auditing, data analysis, or healthcare consulting.
Top employers hiring certified professionals include:
University of Vermont Medical Center
Copley Health System
North Country Hospital
Remote RCM firms servicing multi-state clients
Earning the AMBCI credential also enables you to qualify for telehealth and payer-specific roles similar to those available under Medical Billing and Coding Certification in Florida.
The statewide growth projection of 9.3% through 2030 means certified coders can expect long-term job stability even as automation reshapes administrative tasks.
6. FAQs: Medical Billing and Coding Certification in Vermont
-
Most candidates complete training and pass the certification exam within 4–6 months, depending on their study pace and program format.
-
A minimum score of 70% is required, with questions based on real-world coding and claim scenarios.
-
Yes. Certified professionals can work remotely with healthcare systems nationwide through AMBCI’s job partner network.
-
Certified professionals earn around $48,200 annually, with senior coders making over $66,000.
-
Yes. Certification must be renewed every 12 months with continuing education in CPT®, ICD-10, and billing law updates.
-
Absolutely. AMBCI certification is recognized nationwide, ensuring career portability across all U.S. states.
-
Enroll in AMBCI’s prep modules and review practice tests from the official AMBCI learning portal for the best results.