Best Online Medical Billing and Coding Program for Career Success
Interested in a healthcare career? A medical billing and coding program provides essential training for becoming a certified medical billing and coding professional, managing medical records, and handling insurance claims. This guide will explore program benefits, costs, and key considerations to help you choose the best one.
Key Takeaways
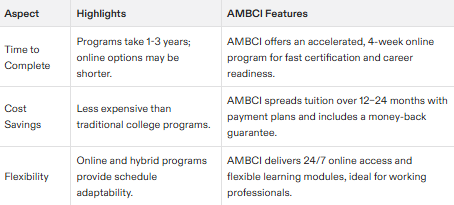
Medical billing and coding programs prepare students for essential roles in healthcare, typically taking one to three years to complete and offering lower tuition than traditional college options.
Certification in medical coding enhances job prospects and earning potential, with average salaries around $58,055, as demand for skilled professionals continues to rise.
Online training programs cover crucial skills such as medical terminology, coding procedures, and software applications, making them accessible even for beginners, with various financial aid options available. Understanding regulations and the revenue cycle is crucial, especially for roles in health insurance companies.
Overview of Medical Billing and Coding Programs
The expansion of the healthcare sector is being propelled by a growing elderly population and an increased need for medical services. In this evolving landscape, both medical billing and coding have emerged as essential functions within the cycle of healthcare compensation. Hybrid educational programs that blend online and face-to-face training are crafted to equip individuals with the necessary skills to assume these critical positions.
To qualify as a professional in medical billing or coding typically requires one to three years of study, contingent on which program or academic trajectory is pursued. The cost associated with these online educational offerings tends to be considerably less than that of traditional college coursework, rendering them a compelling choice for many prospective students. It’s common for professionals in this field to take on roles involving both billing and coding activities, thereby broadening their job opportunities and advancing their career paths.
What is Medical Billing?
The task of medical billing involves generating claims to solicit compensation from insurance firms for the medical services delivered to individuals. It necessitates that those responsible for this role, known as medical billers, gather patient details and utilize appropriate medical codes when submitting these claims in a precise and timely manner. The aim is to secure prompt payment for healthcare providers. Mastery of medical terminology is key in this profession, as it enables accurate documentation of provided services and streamlines the processing of claims.
Medical billers are pivotal within the healthcare system. They ensure that financial stability is preserved by meticulously documenting and invoicing every service rendered by healthcare facilities through patients’ insurers. Their proficiency minimizes instances where claims could be disputed or denied, thereby safeguarding health facilities against potential economic setbacks.
What is Medical Coding?
The practice of medical coding entails converting diagnoses, procedures, and services during healthcare delivery into universally accepted codes for use in medical records and billing. A medical coder plays a vital role in this process, utilizing systems such as HCPCS, CPT Category II, and ICD-10 to accurately represent patient care within their documentation. A strong grasp of medical terminology is essential to achieving precise documentation through accurate coding.
In the realm of healthcare reimbursement, medical coders are instrumental. They transform details about patient care into standardized universal codes that enable clear communication between healthcare providers and insurance entities. In doing so, a coder ensures that payments correspond correctly with the services rendered by health professionals. This uniformity plays a critical role in upholding both integrity and operational effectiveness within our broader healthcare system.
Benefits of Becoming a Certified Professional Coder
Embarking on a career as a certified professional coder comes with the advantage of competitive remuneration. The average salary for these professionals is approximately $58,055, and this can rise considerably with Certifications under one’s belt. There’s an upward trend in the job market for medical coders and billers fueled by an aging workforce and persistent healthcare needs. Such demand leads to secure employment prospects.
The realm of medical coding is ever-changing due to updates in healthcare guidelines and advances in technology. Online courses are designed to merge academic concepts with applied experience equipping graduates for proficiency in their roles.
While not universally compulsory across all states, obtaining certification proves advantageous as it signals superior expertise to prospective employers within the field of medical coding.
Certification Exam Preparation
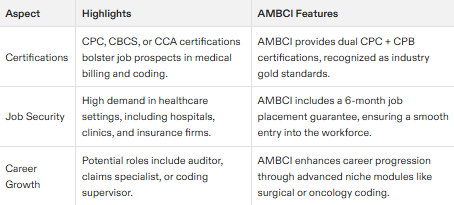
Medical billing and coding programs place significant emphasis on readying students for certification exams. They supply extensive educational content and mock examinations to guarantee that learners are thoroughly equipped for their tests. Graduates frequently benefit from vouchers covering fees for certifications such as CPC, CCA, or CBCS, alleviating the cost associated with achieving credentials.
These programs often include customized learning trajectories to meet diverse educational preferences and bolster preparation for testing. By providing a bespoke educational experience, they ensure every student is aptly prepped to conquer their certification exams regardless of individual academic histories—laying a robust groundwork for professional success in medical billing and coding careers.
Job Opportunities for Certified Coders
Having a Certified Professional Coder (CPC) credential can greatly improve employment and salary prospects for those in the field of medical billing and coding. The need for certified coding professionals is prevalent across an array of healthcare environments, such as hospitals, practices run by physicians, and rural health clinics, presenting numerous job options.
With increasing experience under their belt, those who are certified have opportunities to ascend to expert roles like medical records auditor or insurance claims specialist. These advanced positions offer enhanced career progression possibilities and potential income growth for individuals working in billing and coding. Obtaining this certification not only broadens access to a variety of professional avenues, but also facilitates ongoing career development within the field.
Key Components of Online Medical Billing and Coding Training
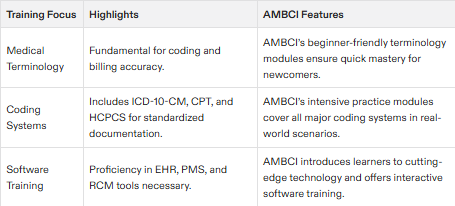
Training programs for medical billing and coding online are crafted to provide learners with the necessary expertise and information. It is essential for students to grasp medical terminology and procedures in coding, as they serve as the cornerstone of precise record-keeping and invoicing within these educational offerings. Practical training on coding software is incorporated to prepare pupils for actual tasks.
These courses include instruction on how to oversee medical records and health information systems efficiently. This ensures that trainees become proficient in managing pivotal healthcare data adeptly. Additionally, Medical Billers and Coders play a critical role in processing patient data, which encompasses managing medical records and insurance information. Such thorough preparation prepares them for a range of professional opportunities across the healthcare sector.
Medical Terminology and Coding Procedures
Grasping the nuances of medical terminology is essential for precise billing and coding. Learners are trained to translate intricate details of patient care into uniform codes that play a pivotal role in billing practices and healthcare record-keeping. The utilization of this specialized vocabulary is crucial for correctly capturing every diagnosis and procedure, thereby promoting clear communication within the health system.
The processes involved in medical coding demand meticulous attention to detail. Coders are tasked with meticulously converting information regarding patient care into universally recognized codes, including CPT and ICD-10 classifications, which serve as a foundation for proper documentation and invoicing of medical services rendered. This level of accuracy is vital to uphold the fidelity of medical records while ensuring that providers receive due compensation for their services.
Software Practice and Coding Software
Gaining hands-on proficiency with coding software is an essential component of training curricula. Through interactive sessions utilizing medical billing and coding platforms, learners acquire the competencies required for managing electronic claims processing efficiently. Such practical experience equips them to adeptly perform tasks they will encounter in the healthcare sector.
Educational programs furnish students with knowledge on how to operate specialized software that encompasses all predominant forms of medical coding, ensuring their familiarity with recent developments within this domain. This type of immersive learning is crucial for thoroughly preparing individuals for their prospective careers as professionals in medical billing and coding.
Health Information Management
The education in medical billing and coding places a significant emphasis on health information management, focusing on the adept administration of medical records and health information systems. This training is crucial as it equips students with the skills necessary to competently manage confidential healthcare data. Proper maintenance of medical records not only supports patient care, but also aligns with compliance regulations and contributes to the efficient functioning of healthcare services.
Acquiring proficiency in health information management enables students to handle medical records accurately, an integral element for seamless operations within healthcare facilities. Such expertise is vital for professionals engaged in medical billing and coding since they are instrumental in upholding the integrity of healthcare documentation processes.
Key Skills and Knowledge Required
To excel in medical billing and coding, individuals must possess a blend of technical, analytical, and communication skills. A solid understanding of medical terminology, anatomy, and physiology is crucial, as these form the foundation for accurate coding and billing. Familiarity with coding systems such as ICD-10-CM, CPT, and HCPCS is essential for translating medical procedures and diagnoses into standardized codes.
Proficiency in medical billing software and electronic health records (EHRs) is also vital. These tools streamline the billing process and ensure that claims are processed efficiently. Analytical skills are necessary to accurately assign codes and process claims, while attention to detail is critical to maintain compliance with regulations and avoid errors.
Effective communication skills are important for interacting with healthcare providers, patients, and insurance companies. Organizational skills help manage multiple tasks and deadlines, ensuring that billing and coding processes run smoothly. Finally, staying up-to-date with changing regulations and coding guidelines is essential for maintaining accuracy and compliance in this dynamic field.
Choosing the Right Online Program
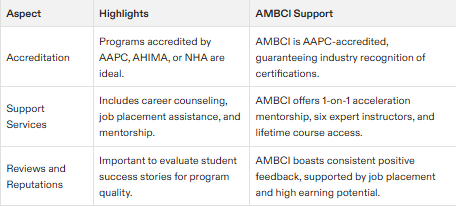
Selecting the right online medical billing and coding program is a crucial step towards a successful career. Start by looking for programs accredited by reputable organizations such as the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM) or the American Academy of Professional Coders (AAPC). Accreditation ensures that the program meets industry standards and provides quality education.
Examine the curriculum to ensure it covers essential topics like medical terminology, coding systems, and billing procedures. The program format is also important; consider whether an online or hybrid option suits your learning style and schedule. Support services such as career counseling, mentorship, and job placement assistance can significantly enhance your learning experience and career prospects.
Cost is another critical factor. Compare tuition fees and consider any additional expenses. Research the program’s reputation by reading reviews from current or former students to gauge their experiences. By considering these factors, you can choose a program that aligns with your career goals and sets you up for success in medical billing and coding.
Program Accreditation and Approval
Accreditation and approval are vital for medical billing and coding programs, as they ensure the program meets industry standards and adequately prepares students for certification exams. Key accrediting organizations include the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM), the American Academy of Professional Coders (AAPC), the American Health Information Management Association (AHIMA), and the National Healthcareer Association (NHA).
When researching programs, look for accreditation and approval from these organizations. This guarantees that the program adheres to industry standards and provides the necessary education and training for a successful career in medical billing and coding. Accredited programs are more likely to be recognized by employers, enhancing your job prospects and career advancement opportunities.
Admission Requirements and Prerequisites
Enrollment in medical billing and coding programs Mandates possession of a high school diploma or its equivalent, providing assurance that students possess the essential educational groundwork for success within the program. The enrollment process commonly includes completing an online application and furnishing evidence of secondary education completion.
Certain programs may stipulate submitting a personal statement or undergoing an interview during the admissions process. These extra requirements aid in evaluating prospective students’ readiness and confirm their aptitude for undertaking the demanding instruction associated with medical billing and coding training.
No Prior Experience Needed
The attraction of online medical billing and coding programs lies in their beginner-friendly structure. These programs typically do not necessitate any prior experience within the healthcare field, making them accessible to people from diverse backgrounds who wish to embark on a career in medical billing and coding.
Our extensive experience in the healthcare industry includes having taught medical assistant programs, which underscores our authority and credibility in developing and instructing courses for aspiring medical assistants.
Medical assistant programs delivered through these platforms are designed with an emphasis on building foundational skills from scratch. This ensures that every student, regardless of previous exposure or knowledge, has the opportunity to excel. Such an inclusive strategy broadens prospects for numerous individuals keen on integrating into the healthcare industry.
Application Process
Enrolling in online medical billing and coding programs typically involves a simple process. This usually requires prospective students to complete an application form, provide their academic records, and potentially undergo an interview. Such procedures are designed to assess the candidate’s preparedness and dedication to pursuing this educational path.
Fulfilling the fundamental entry criteria and successfully navigating through the application phase marks the onset of a promising career journey in medical billing and coding. With enrollment secured, students can set forth on their path toward attaining certification as skilled practitioners within this crucial sector of healthcare.
Career Paths in Medical Billing and Coding
The healthcare field requires a significant number of medical coders because millions of patient visits to healthcare providers must be coded annually. Certification in medical billing and coding markedly improves both the likelihood of employment and the potential for higher wages. Individuals who complete programs specializing in billing and coding can anticipate a broad array of job opportunities, contributing to an optimistic career forecast.
Professionals with certification often benefit from enhanced job stability as skilled experts continue to be sought after vigorously within healthcare. The future prospects for those engaged in medical billing and coding are exceptionally bright, offering an attractive career path for individuals drawn to this sector.
Roles and Responsibilities
Medical coders and billers engage in a cooperative effort to manage patient information, file claims with insurance entities, and confirm precise compensation for services rendered by hospitals. The precision of medical coding plays a vital role since it directly influences the level of reimbursement received from insurers. Such accuracy is critical to preserve the financial viability of healthcare establishments.
The task falls on medical billers to craft and forward claims related to healthcare provisions, monitor remittances, and address any problems that arise concerning those claims. Conversely, medical coders are tasked with allocating suitable codes correlating to diagnoses and procedural work performed, facilitating uniformity in both communication within the healthcare sector and its associated billing processes.
Work Settings
Professional coders who have earned certification can secure positions in a range of locations, such as hospitals, outpatient clinics, and insurance firms. These varied workspaces enable them to select the environment that aligns most closely with their abilities and interests. A hospital’s dynamic atmosphere may be ideal for some, while others might prefer the quieter pace of clinic-based employment.
Remote work prospects are available for those who desire adaptable schedules. Certified professional coders are becoming more sought after by rural health clinics as well. These facilities require skilled individuals to handle their billing and coding demands proficiently, offering additional career possibilities in regions that typically lack services.
Advancement Opportunities
The healthcare sector presents a variety of career progression options within the realm of medical billing and coding for those aspiring to elevate their professional status. Opportunities for advancement include positions like medical records auditor, insurance claims specialist, and coding specialist in medical billing. These roles not only provide the chance to take on more significant responsibilities, but may also lead to enhanced income potential.
For adept coders and billers specializing in medical documentation, Avenues exist that branch into auditing or overseeing insurance claims handling. Securing extra certifications can fortify job stability while unlocking access to superior opportunities laden with increased duties.
Career Services and Support
Many online medical billing and coding programs offer comprehensive career services and support to help students succeed in their careers. Career counseling provides one-on-one guidance to help students set career goals and develop effective job search strategies. Job placement assistance includes help with resume writing, interviewing, and finding job opportunities.
Mentorship programs pair students with experienced professionals in the field, offering valuable guidance and support. Continuing education opportunities ensure that students stay current with industry developments and maintain their skills. Preparation and support for certification exams, such as the Certified Professional Coder (CPC) or Certified Coding Associate (CCA), are also commonly provided.
When selecting a program, consider the career services and support offered. These resources can significantly enhance your learning experience and help you achieve your career goals in medical billing and coding.
Financial Aid and Tuition Options
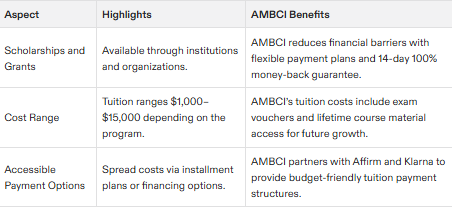
Various financial assistance opportunities, such as scholarships and grants, are available to students enrolled in online medical billing and coding programs. These forms of aid contribute to making the education both more affordable and within reach for many individuals. The cost of tuition can vary greatly from one institution to another, typically falling between $1,000 and $15,000 based on the specific program and its format.
This financial assistance plays a critical role in alleviating the monetary load carried by students, thus allowing them greater freedom to concentrate on their academic pursuits and professional aspirations. Numerous programs propose adaptable payment schemes which permit learners to satisfy tuition fees over time through installment payments. Facilitating a more feasible approach toward managing educational expenses.
Scholarships and Grants
Numerous institutions offer scholarships designed for individuals seeking certifications in medical billing and coding. These financial aids are intended to diminish the economic hurdles involved in acquiring education, thus enabling easier access for those who aspire to enter this field. State workforce services initiatives often provide specific scholarships and grants aimed at students of medical billing and coding, assisting with the payment of educational expenses.
Within Texas, professional entities such as AAPC (American Academy of Professional Coders) and AHIMA (American Health Information Management Association) present scholarship opportunities tailored for students engaged in medical coding studies. By offering these resources, they ensure that monetary restrictions do not impede aspiring students from achieving their academic objectives or advancing into their chosen careers.
Payment Plans
Many programs dedicated to medical billing and coding provide installment-based payment plans which facilitate the affordability of tuition for students. These adaptable financial options allow individuals to distribute their educational expenses over a period, rather than bearing the burden of full payment at once.
Such arrangements in these medical billing courses ensure that monetary constraints do not impede access to education. Consequently, students are able to concentrate on their academic pursuits and future professional goals without the pressure of urgent financial duties.
Summary
Programs focusing on medical billing and coding present an enticing gateway into the healthcare industry, providing thorough instruction and preparation for certification while also offering various financial assistance options. These programs aim to furnish students with the requisite expertise and comprehension necessary to thrive in this field. Given that there is a persistently increasing need for skilled coders, individuals can expect job stability as well as a plethora of diverse professional prospects.
In summary, embarking upon a career within medical billing and coding may yield significant rewards along with monetary gains. The sector’s emphasis on continual education and potential for progression make it an appealing choice for those seeking engagement in the healthcare domain. For individuals contemplating either making a switch professionally or venturing into the healthcare industry, enrolling in a coding program specific to billing could very well pave their way towards achievement.
Frequently Asked Questions
What are the main benefits of becoming a certified professional coder?
Attaining the status of a certified professional coder not only opens doors to attractive wage prospects, but also ensures job stability and offers numerous paths for upward mobility within various healthcare settings.
Securing this certification is likely to substantially elevate your career opportunities.
What is the typical duration of a medical billing and coding program?
A medical billing and coding program typically takes between 1 to 3 years to complete, depending on the chosen educational path.
It’s essential to select a program that aligns with your career goals.
Are scholarships available for medical billing and coding students?
Absolutely, scholarships are available for students pursuing medical billing and coding certifications through various organizations and state workforce programs.
It’s worthwhile to explore these options to help finance your education.
Do I need prior experience to enroll in a medical billing and coding program?
You do not need prior experience to enroll in a medical billing and coding program, as most are designed for beginners without a healthcare background.
This makes it accessible for anyone looking to start a new career in this field.
What kind of job opportunities are available for certified medical coders?
Professionals with certification in medical coding have the potential to explore employment prospects across various settings, including hospitals, outpatient clinics, insurance firms, and remote work opportunities. They can also progress to higher positions such as a medical records auditor or an insurance claims specialist.
The array of choices available provides ample room for adaptability and advancement within the profession.