Top Medical Billing Assessment Test: Boost Your Skills with Real-World Scenarios
Gearing up for a medical billing assessment test? This examination measures your proficiency in key sectors such as coding, insurance verification, medical billing, and managing claims. In the subsequent text, we delve into the crucial aspects evaluated during these tests along with suggestions on how to prepare effectively and the advantages that come with obtaining certification. Understanding various health insurance options, including Anthem health insurance, is essential as it relates to medical billing assessment tests. Prepare yourself to thrive in your career within medical billing!
Key Takeaways
Medical billing assessment tests evaluate candidates’ proficiency in coding, claims management, and insurance eligibility verification, essential for minimizing errors and optimizing healthcare operations.
Certification exams, such as CPC and CPB, validate medical billers’ knowledge in areas like healthcare regulations and coding, significantly enhancing job prospects and earning potential.
Consistent practice through mock tests and structured study plans is crucial for success in medical billing assessments, equipping candidates with the skills and confidence necessary for the field.
Overview of Medical Billing Assessment Tests
Assessment tests for medical billing are critical in guaranteeing that healthcare providers receive appropriate and timely compensation for their services. These evaluations measure the adeptness of applicants across different facets of medical billing, including coding and managing claims. For hiring entities, these assessments serve as essential instruments to filter prospective employees and confirm that they possess the aptitude required to flourish in positions such as medical billers, coders, or revenue cycle managers.
The importance of assessment tools specific to medical billing is immense. Given the intricate nature of medical billing processes and how inaccuracies can result in substantial financial deficits, these examinations help uphold stringent standards within this sector. They play a vital role by ensuring only highly capable individuals take on the responsibility for key activities like processing bills and codes—this minimizes error margins while boosting efficiency across healthcare administrative functions.
Understanding healthcare costs and the role of healthcare service providers is crucial in the medical billing process. Accurate calculation of co-pays and other expenses ensures correct billing and prevents disputes, which is essential for the overall management of healthcare expenses.
In an arena where precision is crucial at every juncture, tests evaluating proficiency in medical billing set a standard against which professionals’ abilities can be measured. Successfully navigating these examinations underlines practitioners’ dedication to adhering to industry protocols while highlighting their meticulous approach to navigating complex scenarios related to handling tasks associated with both medical billing and coding.
Understanding Medical Billing
Medical billing is the backbone of the healthcare revenue cycle, ensuring that healthcare providers receive payment for the medical services they render. This intricate process involves submitting and following up on claims with health insurance companies, which requires a deep understanding of health insurance policies, medical coding, and reimbursement procedures. The primary goal of medical billing is to secure timely and accurate payments, which is crucial for the financial health of healthcare providers.
In essence, medical billing translates the healthcare services provided into billing claims. These claims are then sent to health insurance companies for reimbursement. The process demands meticulous attention to detail and a thorough understanding of the various insurance plans and their specific requirements. By mastering medical billing, healthcare providers can minimize errors, reduce the risk of denied claims, and ensure a steady flow of revenue.
Medical Billing Process and Procedures
The medical billing process is a multi-step journey that begins the moment a patient registers at a healthcare facility and continues until the provider receives payment. Each step in this process is vital for ensuring accuracy and compliance with regulatory standards.
Patient Registration: This initial step involves collecting and verifying patient information, including demographics and insurance details. Accurate data entry at this stage is crucial for the subsequent steps.
Charge Capture: During this phase, healthcare providers document the services rendered to the patient. This documentation forms the basis for billing and coding.
Medical Coding: Here, the documented services are translated into standardized codes using systems like ICD-10 and CPT. Accurate coding is essential for proper claim submission and reimbursement.
Claim Submission: The coded information is compiled into a claim, which is then submitted to the patient’s health insurance company. Electronic submission is preferred for its efficiency and speed.
Payment Posting: Once the claim is processed and payment is received, the payment is posted to the patient’s account. Any discrepancies or unpaid amounts are addressed through follow-up procedures.
Efficient medical billing procedures are essential for handling denied claims, appeals, and patient inquiries. By ensuring each step is performed accurately and in compliance with regulatory requirements, healthcare providers can optimize their billing processes and improve their financial outcomes.
Steps Involved in Medical Billing
Medical billing is a complex process that involves several steps to ensure that healthcare providers receive accurate and timely reimbursement for their services. Here are the key steps involved in medical billing:
Patient Registration: The first step in medical billing is patient registration, where the patient’s demographic and insurance information is collected and verified. Accurate data entry at this stage is crucial for the subsequent steps.
Charge Capture: After the patient receives medical services, the healthcare provider captures the charges for those services, including the date, time, and type of service provided. This documentation forms the basis for billing and coding.
Coding: The charges are then coded using standardized coding systems, such as ICD-10 and CPT, to ensure that the services are accurately represented. Accurate coding is essential for proper claim submission and reimbursement.
Claim Submission: The coded charges are then submitted to the patient’s health insurance provider for reimbursement. Electronic submission is preferred for its efficiency and speed.
Adjudication: The insurance provider reviews the claim and determines the amount of reimbursement based on the patient’s coverage and any applicable deductibles or copays. This step is crucial for ensuring that the healthcare provider receives the correct payment.
Payment: The insurance provider sends payment to the healthcare provider for the approved amount. Timely payment is essential for the financial health of the healthcare provider.
Patient Billing: If there is a balance remaining after insurance payment, the healthcare provider sends a bill to the patient for the outstanding amount. Clear communication with the patient is important to avoid confusion and disputes.
Follow-up: The healthcare provider follows up with the patient and insurance provider to ensure that payment is received and any issues are resolved. Effective follow-up procedures help in managing accounts receivable and maintaining cash flow.
By following these steps meticulously, healthcare providers can ensure accurate and efficient medical billing, which is essential for maintaining financial stability and providing high-quality medical services.
Key Areas Covered in Medical Billing Assessment Tests
Assessments in medical billing aim to gauge a candidate’s expertise in several vital areas that contribute to precise and expedient billing processes. A key area evaluated is the candidate’s grasp of medical coding, which requires an intricate understanding of anatomical details and meticulous attention as minor variances in codes can result in significant errors.
The ability to confirm insurance coverage, handle denials effectively, and submit accurate claims is another essential skill scrutinized during these assessments. It’s imperative for healthcare providers to have assurance of proper compensation for their services provided. Knowledge about handling Medicare patient inquiries—along with being aware of filing deadlines—is emphasized.
Evaluation also extends to assessing skills related to documentation—the candidates must prove they are capable of keeping accurate medical records and conveying billing information efficiently—as this plays a critical role in streamlining healthcare service delivery. They must show comprehension concerning ethical practices within the system too. Such considerations include ensuring legality by not charging patients prior to processing insurance claims.
Finally, proficiency questions regarding regulations around health care provision—including those associated with government-funded plans like Medicare or Medicaid—and private insurers form part of these comprehensive exams. Handling medicare patient calls is crucial, as it involves understanding patient interactions related to Medicare services, addressing financial concerns, and providing appropriate responses based on Medicare policies. Such aspects assess whether individuals can adeptly maneuver through various policies pertinent across diverse health insurance arrangements.
Medical Coding and Compliance
Medical coding is a critical component of the medical billing process, involving the assignment of standardized codes to medical diagnoses and procedures. These codes, such as those from the ICD-10 and CPT systems, are used to accurately report the services provided and facilitate reimbursement from health insurance companies.
Medical coders must possess a thorough understanding of these coding systems and ensure that codes are assigned accurately and consistently. This precision is vital for avoiding denied claims, audits, and potential penalties. Compliance with coding regulations is not just about accuracy; it also involves staying updated with the latest coding guidelines and changes in healthcare laws.
By adhering to coding standards and maintaining compliance, healthcare providers can ensure that their claims are processed smoothly and that they receive the appropriate reimbursement for their services. This not only supports the financial health of the practice but also contributes to the overall efficiency of the healthcare system.
Health Insurance and Reimbursement
Health insurance plays a pivotal role in the medical billing process. Healthcare providers must navigate the complexities of various insurance plans, including Medicare, Medicaid, and private insurance, to ensure they receive accurate and timely payments for their services.
Understanding the nuances of different health insurance plans is essential. Each plan has its own reimbursement rates, deductibles, and copays, which can significantly impact the billing process. Healthcare providers must be knowledgeable about these aspects to accurately bill patients and insurance companies.
Reimbursement procedures vary depending on the type of insurance. For instance, Medicare and Medicaid have specific guidelines and rates that differ from those of private insurance plans. By mastering these procedures, healthcare providers can optimize their billing processes, reduce the risk of denied claims, and ensure a steady flow of revenue.
Preparing for a Medical Billing Assessment Test
To excel in medical billing assessment tests, it is essential to prepare adequately. Create a well-organized study schedule that designates time slots and pinpoints the main topics that require attention. Opting for brief but regular study intervals tends to be more beneficial than lengthy, exhaustive sessions as this approach aids memory retention and helps prevent fatigue.
It is advisable to engage with practice exams as these can acclimate you to the test layout while pinpointing subjects where additional focus may be necessary. Utilizing a medical biller practice test can be particularly beneficial as it simulates the actual certification examination, helping you demonstrate your knowledge and skills in medical billing. These preparatory assessments are instrumental in mirroring real exam conditions, which bolsters your ability to manage time effectively and alleviates stress related to testing situations. Participation in study groups offers critical support and varied perspectives on intricate matters, thus enriching your grasp of material.
Incorporating relaxation methods alongside established studying tactics can also aid in mitigating tension linked with exams resulting in heightened concentration levels and better performance outcomes during tests. Segmenting learning materials into manageable portions coupled with efficient organization of study time comes highly suggested by educators. Understanding the No Surprises Act can also be beneficial as it relates to financial safeguards in medical billing.
Steadfast commitment through routine practice along with maintaining a disciplined methodology stands imperative for achieving success within medical billing evaluations.
Types of Medical Billing Assessment Tests
Multiple types of evaluation instruments exist to gauge the proficiencies and understanding possessed by individuals in medical billing, each aimed at interrogating various facets of an aspirant’s abilities. Recognized certification examinations like CPC and CPB are instrumental within the sector for measuring a comprehensive grasp of both coding and the intricacies involved in medical billing exams. Such assessments play a pivotal role for those in pursuit of confirming their proficiency while aspiring to elevate their professional trajectory.
Understanding health insurance portability and health insurance probability is crucial as part of these medical billing assessment tests. The Health Insurance Portability and Accountability Act (HIPAA) ensures that patients can maintain their health insurance benefits when they change jobs or move to different states, while analyzing health insurance probability helps in understanding how different insurance plans impact patient care and billing practices.
Pre-employment evaluations constitute another prevalent category used within hiring processes, employed specifically to sift through potential hires based on job-aligned skill sets such as precise code application or adept claims handling. These evaluations serve employers by facilitating informed decision-making when discerning which applicants possess qualifications that align with organizational needs.
For current practitioners who wish to polish or modernize their expertise surrounding medical billing protocols, there are targeted skill enhancement tests available. Concentrating on particular segments such as emerging stipulations or sophisticated coding methodologies, these assessments support medical billers’ efforts to remain well-informed about evolving industry standards thereby preserving an edge within this competitive field. Irrespective of testing type, all aim singularly towards ensuring that professionals engaged in medical billing duties maintain a high caliber performance level essential for effective practice management.
Certification Exams: CPC, CPB, and Medical Billing Exam
Examinations for certifications, including the CPC (Certified Professional Coder) and CPB (Certified Professional Biller), serve to confirm an individual’s expertise and skills within the realms of medical coding and billing. These examinations gauge proficiency in various domains such as understanding insurance programs, familiarity with healthcare regulations, and mastery of medical coding through a series of multiple choice questions that evaluate a comprehensive grasp on these subjects.
Specifically targeting foundational knowledge pertinent to medicine is the focus of the CPB examination. It investigates one’s acquaintance with critical components like medical terminology, anatomy, and pathophysiology. Mastery in these fundamental areas ensures precise execution in tasks related to coding and billing.
The option for candidates to undertake their certification assessments at home comes courtesy of Live Remote Proctored (LRP) exams. This advancement not only simplifies logistics by enabling test-taking from one’s dwelling, but also upholds stringent standards governing exam integrity.
It is strongly advised that prospects seeking success dive into specialized preparation courses crafted by those who designed these exams – AAPC being a notable provider. Such preparatory platforms deliver hands-on experiences through practical examples while sharing insights into effective strategies for taking tests alongside expansive educational content—thus fortifying aspirants’ competencies essential for triumphing over their respective certification evaluations. Securing this credential affirms professional capability, which subsequently amplifies career opportunities along with prospective financial rewards.
Medical Biller Practice Test and Sample Questions
Utilizing practice tests is an essential strategy for those getting ready for either a medical billing assessment test or practicing as a medical biller. They are beneficial in acclimating you to the structure and pace of the actual exam, enabling you to hone your time management capabilities effectively. By doing timed practice exams, you can recreate the conditions of the real test environment, which helps diminish stress levels and bolsters your confidence when taking the actual test.
Understanding skilled nursing facility codes is crucial in the context of medical billing and coding, as these codes are reimbursed on a per diem basis, highlighting their significance in the billing process associated with healthcare services provided in skilled nursing facilities.
For individuals seeking resources, CertificationCoaching.Org offers an exceptional array of complimentary practice tests and study materials tailored for medical billers and coders. The provided practice exams encompass numerous questions that span various aspects of medical billing, assisting in pinpointing specific areas where Study might be required while reinforcing existing knowledge.
Making practice examinations part of your preparation routine can greatly improve your readiness for testing. Engaging in frequent self-assessment not only allows monitoring progress but also reveals strengths and weaknesses – guiding adjustments to learning approaches accordingly. The secret lies in consistent application combined with deep comprehension across all subject matter related to medical billing.
Medical Billing Challenges and Solutions
Medical billing is fraught with challenges that can hinder the efficiency and accuracy of the billing process. Common issues include denied claims, delayed payments, and patient inquiries, all of which can disrupt the revenue cycle and impact the financial health of healthcare providers.
To overcome these challenges, healthcare providers must implement efficient medical billing processes. This includes investing in advanced medical billing software that automates and streamlines various tasks, reducing the likelihood of errors. Additionally, ongoing training for medical billing staff is crucial to keep them updated with the latest coding guidelines and regulatory changes.
Staying abreast of regulatory changes and coding updates is essential for maintaining compliance and accuracy. By implementing these solutions, healthcare providers can enhance their medical billing processes, minimize errors, and ensure timely and accurate payments for their services. This proactive approach not only improves financial outcomes but also contributes to the overall efficiency and effectiveness of the healthcare system.
Real-World Scenarios and Case Studies
Here are some real-world scenarios and case studies that illustrate the complexities of medical billing:
Emergency Medical Treatment: A patient receives emergency medical treatment at a hospital and is uninsured. The hospital must provide emergency medical treatment regardless of the patient’s ability to pay, but may still bill the patient for the services provided. This scenario highlights the importance of understanding emergency medical treatment regulations and the financial implications for both the patient and the healthcare provider.
Health Insurance Portability: A patient changes jobs and health insurance providers, but still receives medical services from the same healthcare provider. The healthcare provider must ensure that the patient’s new insurance information is updated and that claims are submitted to the correct insurance provider. This scenario underscores the need for healthcare providers to be adept at managing health insurance portability to avoid billing errors and ensure timely reimbursement.
Unexpected Medical Bills: A patient receives unexpected medical bills from a healthcare provider for services that were not covered by their insurance. The patient may dispute the charges or negotiate with the healthcare provider to reduce the amount owed. This case study illustrates the challenges of dealing with unexpected medical bills and the importance of clear communication and billing transparency.
Skilled Nursing Facility Codes: A healthcare provider must use specific codes to bill for services provided at a skilled nursing facility. The codes must be accurate and up-to-date to ensure that reimbursement is received. This scenario highlights the critical role of skilled nursing facility codes in the billing process and the need for precise coding to avoid denied claims.
Bill Medicaid Patients: A healthcare provider must follow specific guidelines when billing Medicaid patients, including using the correct codes and submitting claims in a timely manner. This case study emphasizes the importance of understanding Medicaid billing regulations to ensure compliance and secure reimbursement.
Medicare Patient Calls: A healthcare provider receives calls from Medicare patients regarding their bills and must ensure that the patients’ questions are answered and concerns are addressed in a timely and professional manner. This scenario demonstrates the need for effective communication and customer service skills in handling Medicare patient calls to maintain patient satisfaction and resolve billing issues.
These scenarios and case studies illustrate the complexities of medical billing and the need for accurate and efficient billing practices to ensure that healthcare providers receive reimbursement for their services. By understanding and addressing these challenges, healthcare providers can improve their billing processes and enhance their financial outcomes.
Benefits of Passing a Medical Billing Assessment Test: Reducing Healthcare Costs
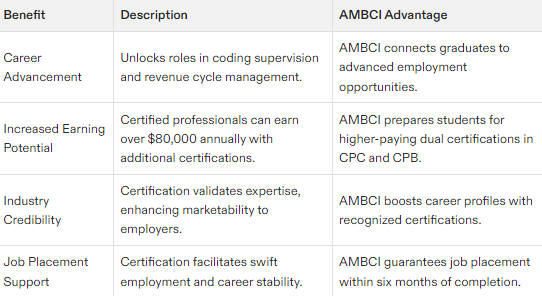
Achieving success in a medical billing assessment test can lead to substantial career progression and monetary advantages. Individuals who are certified as medical billers typically encounter better remuneration prospects compared to those without certification, with potential annual incomes exceeding $80,000 for graduates of certification programs. Thus, acquiring certification constitutes a prudent investment.
Securing this credential offers pivotal career enhancement opportunities within the healthcare sector. A triumph in these rigorous tests paves the way toward elevated roles like revenue cycle management or coding supervision, catalyzing professional development while bolstering job stability and personal market appeal.
Being prepared for unexpected medical bills is crucial, and passing a medical billing assessment test can help manage such situations by ensuring you understand the No Surprises Act and other financial safeguards.
Obtaining medical billing certification underscores a dedicated adherence to industry norms and an ongoing educational pursuit. It communicates to prospective employers that you have mastered the essential expertise required to navigate through the intricacies associated with medical billing tasks—elevating your chances for employment and aiding in delivering superior quality healthcare services.
Expert Tips from AMBCI Instructors
Instructors at AMBCI, who bring a wealth of practical and educational experience, provide essential advice for excelling in medical billing assessment exams. They stress the importance of devising an organized study schedule to systematically tackle the test content. Segmenting the material into digestible parts can not only boost comprehension but also keep you methodically on track as you prepare.
They underscore effective time management as a pivotal factor in succeeding. By designating specific durations for each exam question, it helps prevent disproportionate time being spent on any one area, ensuring completion within the given timeframe. Practice with timing is key to honing this skill and elevating your exam performance.
Gaining certification in medical billing empowers professionals with confidence by arming them with vital capabilities to resolve intricate billing issues competently. It reflects their dedication towards upholding industry standards and commitment to ongoing professional development, which potentially improves employment possibilities and paves the way for career growth.
Testimonials and Success Stories
Listening to the experiences of those who have made a successful switch into the field of medical billing can be quite motivational. Take Binta Patel, for instance, who moved from her corporate role into medical billing and quickly amassed a roster of 13 clients by applying what she learned in her training course. Her narrative is evidence of both the effectiveness of such courses and the possibility for swift professional advancement.
Similarly impactful is Tanya Uzan’s journey. As someone managing household responsibilities, she was able to launch her own venture in medical billing following comprehensive instruction. Her tale underscores not only how adaptable a career in medical billing can be, but also its potential as an attractive option for individuals aiming to strike a balance between their occupation and home life.
Jennifer Moran and Steven Anderson are examples who underscore this point after completing their respective educational programs within the realm of medical billing. Upon finishing her coursework, Jennifer quickly onboarded her inaugural client. Meanwhile, Steven extols his program’s community support system, which significantly broadened his grasp on medical billing concepts that were crucial in acquiring clientele. Their success stories together reinforce just how actionable these training courses are while illustrating entrepreneurial opportunities and career growth available within this sector.
Resources for Further Learning
Those interested in expanding their expertise and capabilities within the realm of medical billing have a plethora of resources at their disposal. The American Association of Professional Coders (AAPC) is renowned for providing an array of study guides, preparatory classes, and certification initiatives that are specifically geared toward enhancing professional proficiency in medical billing, which includes readying individuals for the AAPC medical billing exam. These resources hold significant prestige and credibility across the sector.
Likewise, emergency medical treatment along with a diverse suite of educational materials and seminars aimed at professionals engaged in both delivering medical services and managing related financial aspects are offered by the Centers for Medicare & Medicaid Services (CMS). Their offerings delve into vital areas such as compliance with healthcare laws, procedural nuances around invoicing patients or payors, as well as understanding insurance schemes – all crucial knowledge points for novices through to seasoned practitioners.
Understanding how to bill Medicaid patients is also essential, as it involves specific procedures and legal obligations to ensure compliance with Medicaid regulations.
Accessible online learning portals like Udemy and Alison serve up beginner-level courses on coding tasks connected to patient care accounting practices without charging learners any fee. Such instructional content lays down basic yet robust groundwork pivotal to someone just entering this field. In particular, Alison’s diploma program encompassing key subjects within this domain paired with evaluative tests designed to ascertain participants’ grasp on those very essentials.
Summary
To summarize, assessments in medical billing are crucial for affirming your proficiency and unlocking superior career prospects. Acquiring expertise in critical domains such as medical coding, verifying insurance eligibility, and overseeing claims helps ensure meticulous and prompt billing processes. Adequate preparation through well-organized study agendas, mock examinations, and stress-reduction strategies can markedly improve your likelihood of test success.
Passage of these evaluations brings more than just monetary gains. It paves the way for professional growth and enhances job stability. With sage advice from seasoned educators, motivating accounts of accomplishment, and a wealth of educational materials at your disposal – you possess every requisite tool to thrive within the field of medical billing. Approach this endeavor with assurance and embark on a path that leads to triumph within the realm of medical billing.
Frequently Asked Questions
What is the job placement guarantee offered by AMBCI?
AMBCI instills confidence in those looking to start a new career after program completion by guaranteeing job placement for its graduates within six months.
What is required for enrollment in the program?
A high school diploma or GED is required for enrollment in the program. This is the sole prerequisite.
What type of support is available for students during the program?
Students have access to personalized 1-on-1 career acceleration mentorship and tutoring, providing essential support throughout the program.
This tailored guidance helps ensure their success and development.
What is the cost of the program and the payment plan options?
The program’s cost includes payment plans starting as low as $189 per month, which offers an accessible option for many students.
What kind of instructors are part of the AMBCI program?
The AMBCI program includes expert instructors who possess decades of experience in both practical application and teaching, ensuring high-quality education.