Medical Coding Compliance Dictionary: Essential Terms
Medical coding compliance is the bedrock of financial integrity and ethical responsibility in healthcare. Without a clear framework for compliance, organizations risk regulatory breaches and monetary penalties. Coders serve as the guardians of this process, translating patient care into codes that dictate billing, reimbursement, and legal standing. In the increasingly digital healthcare landscape, where health data privacy laws such as HIPAA are strictly enforced, understanding compliance isn’t optional—it’s a professional imperative.
Compliance demands more than memorizing codes. Medical Coders must master the language of compliance, grasping the legal and procedural nuances that govern the field. Failure to do so jeopardizes not just claims and revenue, but the reputation of entire institutions. This Medical Coding Compliance Dictionary is a precision tool designed for professionals who want to align coding with compliance seamlessly. It breaks down complex terminologies into actionable knowledge, enhancing accuracy, and fortifying legal standing in every claim submission.
Understanding Medical Coding Compliance
What is Medical Coding Compliance?
Medical coding compliance refers to the strict adherence to legal and ethical guidelines that govern the assignment of codes for healthcare services. This ensures accurate reimbursement and protects patient data. It encompasses a range of regulations, including the Health Insurance Portability and Accountability Act (HIPAA) and the Health Information Technology for Economic and Clinical Health (HITECH) Act. Coders must maintain vigilance over these rules, as even minor deviations can trigger audits, penalties, or denial of claims.
The essence of compliance lies in precision—using the correct codes that reflect the actual care provided while ensuring that documentation supports these choices. This extends to procedural standards, privacy protocols, and data security requirements. Every misstep, from incorrect code selection to data mismanagement, can cascade into financial and legal consequences. True compliance mastery integrates regulatory knowledge with medical coding skills, creating a protective shield against systemic vulnerabilities in healthcare operations.
Why Compliance Matters in Medical Coding
Non-compliance in medical coding has a cascading effect that extends beyond billing errors. It exposes healthcare providers to monetary penalties, claim denials, and reputational damage. Regulatory bodies such as the Office of Inspector General (OIG) monitor coding practices to detect fraud, waste, and abuse. Even unintentional errors can result in fines, audits, and potential exclusion from federal healthcare programs.
Coders who prioritize compliance not only protect their organizations but also uphold the integrity of the entire healthcare ecosystem. Consistent application of compliance principles safeguards patient trust, ensures regulatory approval, and enables continuous revenue flow. A coder’s role is pivotal; by embedding compliance into their daily workflow, they become the frontline defense against financial risk and operational disruption.
Essential Terms in Medical Coding Compliance
Core Regulatory Terminologies
HIPAA (Health Insurance Portability and Accountability Act)
HIPAA establishes strict requirements for protecting patient health information and ensuring data security in medical coding. It governs how patient records are stored, accessed, and shared, mandating coders and organizations to implement safeguards against unauthorized access. Non-compliance with HIPAA can result in severe financial penalties and legal action, highlighting the necessity of maintaining patient privacy at every stage of coding and billing.
HITECH Act (Health Information Technology for Economic and Clinical Health)
HITECH complements HIPAA by focusing on electronic health record (EHR) security and the integrity of health IT systems. It incentivizes healthcare organizations to adopt digital solutions while reinforcing penalties for data breaches and non-compliance. Coders must understand HITECH’s implications, particularly in managing electronic documentation and ensuring accurate, secure transmission of patient data.
OIG (Office of Inspector General)
The OIG is tasked with detecting fraud, waste, and abuse in healthcare. It oversees audits, investigates suspicious billing practices, and enforces compliance protocols. Coders must align with OIG guidelines to avoid penalties and ensure organizational credibility. Mastery of OIG expectations empowers coders to proactively identify potential risks, reducing the likelihood of errors and legal challenges.
Key Coding Concepts for Compliance
ICD-10-CM
ICD-10-CM provides a standardized system for diagnostic coding, crucial for accurately representing patient conditions. Its detailed structure requires coders to select codes that precisely correspond to clinical documentation, reducing claim rejections and facilitating proper reimbursement. Understanding ICD-10-CM’s hierarchy and specificity is essential for compliance.
CPT (Current Procedural Terminology)
CPT codes capture procedural details of patient care, serving as the backbone for reimbursement and documentation. Coders must match procedures to appropriate CPT codes, ensuring that documentation supports code selection. Missteps in CPT coding can result in audits, payment delays, or penalties, emphasizing the need for precision.
HCPCS (Healthcare Common Procedure Coding System)
HCPCS expands coding capabilities by addressing supplies, equipment, and ancillary services not covered by CPT. Coders use these codes to accurately reflect non-physician services and durable medical equipment. Mastery of HCPCS ensures comprehensive claim submissions and supports compliance with regulatory billing standards.
Audit and Error Prevention Terms
Medical coding compliance demands vigilance over common pitfalls. Terms like upcoding (using a code for a higher-paying service than performed), downcoding (assigning a lower-paying code despite documentation), and medical necessity (ensuring the service was justified and appropriate) are central to maintaining compliance. Misuse of these concepts can result in claim denials, audits, and penalties. Coders must rigorously align documentation with coding choices to prevent these errors and uphold organizational integrity.
| Term | Explanation |
|---|---|
| HIPAA (Health Insurance Portability and Accountability Act) | Protects patient health information, enforces data security, and mandates safeguards against unauthorized access. Non-compliance leads to penalties and legal action. |
| HITECH Act (Health Information Technology for Economic and Clinical Health) | Reinforces EHR security and integrity, incentivizes digital health solutions, and imposes strict penalties for breaches. |
| OIG (Office of Inspector General) | Detects fraud, waste, and abuse in healthcare, oversees audits, and enforces compliance to prevent errors and penalties. |
| ICD-10-CM | Standardized diagnostic coding system aligning codes with clinical documentation, reducing rejections and ensuring compliance. |
| CPT (Current Procedural Terminology) | Captures procedural details for reimbursement and documentation; errors can cause audits and delays. |
| HCPCS (Healthcare Common Procedure Coding System) | Covers supplies, equipment, and ancillary services beyond CPT; essential for comprehensive and compliant claim submissions. |
| Upcoding | Using a higher-paying code than justified; leads to audits, penalties, and loss of payer trust. |
| Downcoding | Using a lower-paying code despite documentation; results in revenue loss and compliance risks. |
| Medical Necessity | Ensuring services are justified and appropriate; missteps can result in denied claims and penalties. |
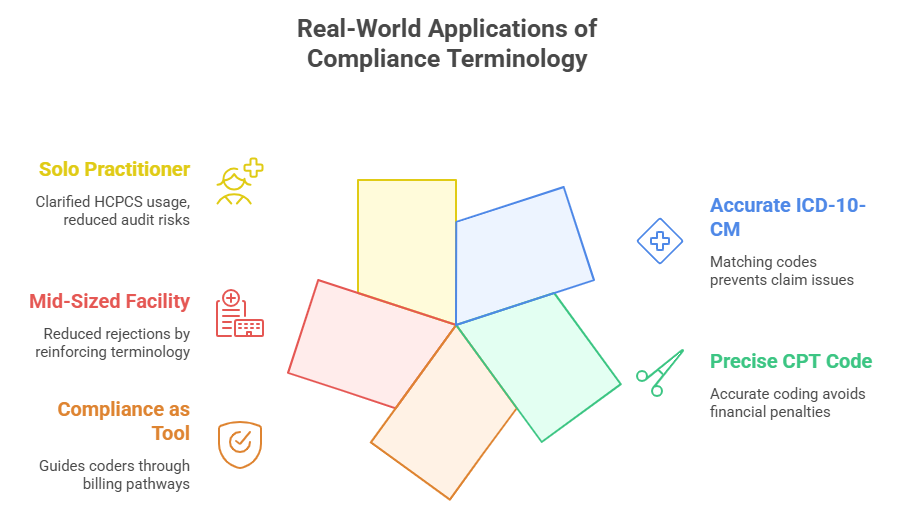
Real-World Applications of Compliance Terminology
How Compliance Terms Affect Day-to-Day Coding
In practical settings, understanding compliance terminology transforms medical coding from a mechanical task into a precise, strategic function. For instance, a coder handling claims for outpatient visits must correctly apply ICD-10-CM codes that align with the physician's documentation. Selecting an incorrect diagnosis code—whether through misunderstanding or oversight—can result in claim rejections or trigger audits. The necessity of matching clinical notes with exact codes reinforces the importance of compliance terms in daily operations.
Similarly, the use of CPT codes requires coders to be acutely aware of procedural details. An inaccurately coded procedure, such as incorrectly billing a complex surgery instead of a minor procedure, can lead to financial penalties and loss of payer trust. Compliance terminology acts as a navigational system, guiding coders through intricate billing pathways and ensuring every claim meets regulatory expectations.
Case Studies in Coding Compliance
Consider a mid-sized healthcare facility that implemented a rigorous compliance training program focused on essential terminology. Prior to this initiative, the facility faced frequent denials due to upcoding errors and vague documentation. By reinforcing compliance vocabulary and ensuring coders fully understood terms like “medical necessity” and “appropriate documentation,” the organization saw a 30% reduction in claim rejections within six months.
In another case, a solo practitioner partnered with a coding consultant to overhaul their billing process. The consultant introduced precise definitions for HCPCS codes related to durable medical equipment, eliminating billing inconsistencies. As a result, the practitioner not only reduced audit risks but also increased reimbursement by 15%, demonstrating the tangible benefits of mastering compliance terminology.
Common Challenges in Coding Compliance
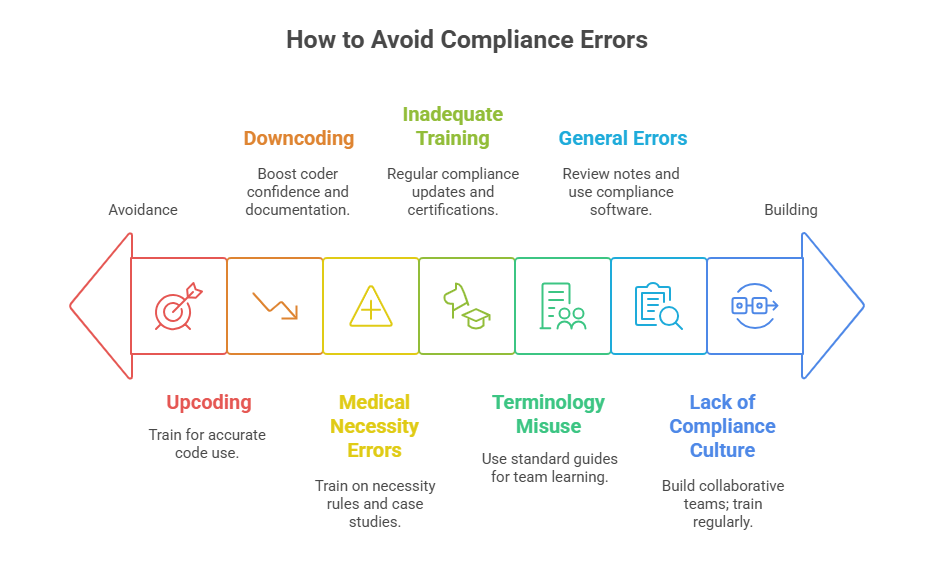
Frequent Pitfalls in Applying Compliance Terms
Even experienced coders encounter challenges when applying compliance terms to real-world cases. One common pitfall is upcoding, which occurs when a code is selected for a higher-level service than was actually performed. This can be due to misunderstanding clinical documentation or pressure to maximize reimbursement. On the flip side, downcoding happens when lower-level codes are selected, often out of caution or uncertainty, resulting in revenue loss. Another prevalent issue is incorrectly determining medical necessity, leading to claims for services that insurers deem unjustified.
Inadequate training or failure to stay updated with evolving regulations exacerbates these pitfalls. Misunderstanding terminologies or applying them inconsistently invites audits, financial penalties, and even exclusion from insurance programs. Coders must proactively stay informed and develop the skill to interpret complex clinical documentation with precision.
How to Avoid Compliance Errors
To prevent errors, coders must adopt a proactive and structured approach. First, ongoing education is critical. Attending webinars, certification programs, or workshops focused on current regulatory updates and coding standards helps maintain competency. Regular participation in case study discussions can also sharpen decision-making skills and reduce coding inaccuracies.
Second, thorough documentation review is essential. Coders should cross-reference clinical notes with applicable codes, verifying consistency and accuracy. Leveraging coding compliance software can assist in detecting potential discrepancies before claims submission. Implementing internal audit systems provides an additional layer of protection, identifying and correcting errors early.
Finally, fostering a culture of compliance mindfulness within organizations ensures coders, billers, and clinical staff collaborate effectively. This holistic approach not only mitigates risk but also supports consistent revenue flow and operational stability.
How AMBCI Certification Can Boost Your Medical Compliance Mastery
Why Get Certified in Medical Coding?
Mastering medical coding compliance terminology is not just about passing audits—it’s about building long-term professional credibility. Certification equips coders with in-depth knowledge of ICD-10-CM, CPT, HCPCS, and regulatory guidelines like HIPAA and HITECH. Through formal training, coders develop the capacity to interpret documentation accurately, apply correct codes, and anticipate compliance pitfalls.
A coder with certification is far better prepared to navigate the complexities of medical billing, reducing the risk of penalties and revenue loss. Certification also opens doors to higher earning potential, greater job stability, and expanded career opportunities. The healthcare industry recognizes certified coders as professionals committed to maintaining accuracy and compliance, which is a competitive advantage in a saturated job market.
Enroll in the Medical Billing and Coding Certification
For coders aiming to strengthen compliance mastery, the CPC + CPB Medical Billing and Coding Certification is a comprehensive solution. This dual certification not only sharpens coding skills but also reinforces critical compliance concepts. Covering regulatory frameworks, billing protocols, and code-specific scenarios, the course transforms knowledge into actionable expertise.
By enrolling, you’ll gain access to real-world case studies, live training sessions, and expert-led discussions that align with current compliance demands. Whether you’re entering the field or seeking to elevate your coding practice, this certification ensures you’re well-versed in compliance terminology and prepared to excel. Learn more about our course and take the next step in your compliance journey.
Conclusion
Understanding and mastering medical coding compliance terminology is not a luxury—it’s a necessity for safeguarding both revenue and reputation. Precision in coding, rooted in a firm grasp of ICD-10-CM, CPT, HCPCS, and regulations like HIPAA and HITECH, is essential to ensuring compliance integrity. Coders must not only keep pace with evolving terminology but also integrate these principles into every workflow.
Certification, such as the CPC + CPB, equips coders with the knowledge and confidence to navigate this complex landscape effectively. It bridges the gap between theory and practice, turning compliance from a challenge into an asset. Invest in continuous learning and certification to fortify your expertise and position yourself as an indispensable asset in the healthcare industry. Compliance mastery isn’t just about passing audits—it’s about leading with precision.
Frequently Asked Questions
-
Medical coders must master key regulations like HIPAA, which governs patient data privacy, and HITECH, which strengthens electronic data security. The Office of Inspector General (OIG) guidelines set fraud detection and audit protocols, while ICD-10-CM, CPT, and HCPCS coding systems ensure accurate billing. Understanding these rules isn’t optional—it’s essential for avoiding claim denials, penalties, and audits. Regulatory compliance aligns coding practices with legal requirements, helping organizations safeguard revenue and maintain trust. Ignoring these rules can trigger costly mistakes, damage reputations, and invite regulatory action, making coders the first line of defense in healthcare compliance.
-
Non-compliance with coding regulations results in severe financial penalties, denied claims, and potential exclusion from federal health programs. For instance, upcoding or downcoding errors can trigger audits and fines, while mismanaging patient data under HIPAA or HITECH can result in multimillion-dollar settlements. Beyond direct penalties, coding inaccuracies damage the organization's reputation and revenue flow. Providers may face payment delays or outright denial, leading to cash flow disruptions. Compliance isn’t just about legality; it’s about sustaining financial stability. Coders who ensure precise compliance protect healthcare organizations from avoidable losses and ensure uninterrupted revenue streams.
-
Absolutely. Certified coders possess a deep understanding of compliance principles, coding systems (ICD-10-CM, CPT, HCPCS), and regulations like HIPAA and HITECH. This expertise reduces errors, prevents audits, and ensures accurate claim submissions. Certified coders are trained to align documentation with billing codes, reducing the risk of penalties. Their knowledge also supports operational efficiency and strengthens the organization’s reputation for compliance excellence. Hiring certified coders isn’t just about credentials—it’s a strategic investment in revenue protection and risk mitigation. Coders with certifications like CPC + CPB bring proven compliance mastery to the table, safeguarding the organization’s financial health.
-
Coders can maintain compliance by implementing a structured workflow: reviewing clinical documentation meticulously, cross-referencing codes with notes, and staying updated on regulatory changes. Regular training and certification programs ensure coders stay sharp and adapt to evolving compliance standards. Using coding compliance software adds an extra layer of accuracy, flagging discrepancies before claims submission. Coders should also participate in internal audits and case discussions to refine decision-making skills. Fostering a collaborative culture with providers and billing teams ensures alignment and prevents coding errors. These proactive measures form the backbone of consistent, error-free, and compliant coding practices.
-
HIPAA mandates that coders handle patient data with the highest level of confidentiality, ensuring that only authorized individuals access records. It also enforces safeguards like encryption and secure storage. HITECH amplifies this by applying stricter controls over electronic health records (EHRs), mandating prompt breach reporting and imposing higher penalties for violations. For coders, this means integrating data protection protocols into daily coding tasks, verifying EHR accuracy, and maintaining audit trails. Compliance with these laws isn’t just IT’s job—it’s integral to every coder’s workflow, ensuring privacy, security, and legal compliance across the coding process.
-
“Medical necessity” is the cornerstone of compliant coding. It refers to the justification for services based on a patient’s diagnosis, aligning care with recognized standards. If coders assign codes for services lacking clear medical necessity, claims may be denied, and providers may face audits or penalties. Understanding this concept helps coders align clinical documentation with coding choices, ensuring claims reflect necessary, documented care. It also helps prevent upcoding or downcoding, which can occur when services are coded incorrectly based on necessity. Mastery of medical necessity protects providers’ financial health and maintains compliance integrity.
-
Compliance terminology and regulations evolve frequently, making continuous learning essential. Coders should engage in annual training, attend webinars, and subscribe to compliance updates to stay informed. Regulatory bodies like CMS, OIG, and AHIMA regularly release updates that coders must incorporate into their workflows. Even subtle changes in coding guidelines or documentation requirements can have significant compliance implications. Organizations benefit from supporting coders with professional development opportunities, while individual coders should take ownership of their education. Staying current isn’t optional; it’s a professional responsibility that ensures continued accuracy, compliance, and risk mitigation.
-
The Medical Billing and Coding Certification equips coders with advanced knowledge of compliance principles, including mastery of ICD-10-CM, CPT, HCPCS, and key regulatory frameworks like HIPAA and HITECH. It combines procedural and billing competencies, ensuring coders can align documentation with codes accurately. This dual certification enhances coders’ understanding of revenue cycle management, compliance pitfalls, and coding best practices. It also provides hands-on case studies and expert-led discussions, sharpening skills for real-world scenarios. Organizations value certified coders for their commitment to precision, making the CPC + CPB an essential credential for those seeking to lead in coding compliance.