Guide to Durable Medical Equipment (DME) Coding
Durable Medical Equipment (DME) coding is the backbone of accurate healthcare reimbursement, ensuring medical providers get compensated for essential patient care equipment. From wheelchairs and oxygen concentrators to prosthetics, each item requires a precise HCPCS Level II code and corresponding documentation for claim approval. Mastery of DME coding is no longer optional—it’s a necessity. As the healthcare industry shifts towards data-driven and value-based reimbursement models, errors in documentation or misuse of modifiers can result in claim denials, revenue loss, and even audits. Proper coding ensures alignment with physician orders, medical necessity, and insurance guidelines, ultimately safeguarding revenue and compliance.
The challenges of DME coding stem from evolving regulations, diverse equipment categories, and intricate insurance requirements. Medicare sets specific rules for DME reimbursement, including coverage criteria and proof of medical necessity, while private insurers add their own layers of complexity. Navigating these rules demands a strategic approach and expert knowledge. This guide will equip readers with a comprehensive understanding of DME coding, from its core principles to advanced reimbursement strategies. It also highlights how AMBCI’s Medical Billing and Coding Certification equips professionals to thrive in this complex environment by enhancing compliance, accuracy, and revenue cycle management.
Understanding Durable Medical Equipment
Definition and Scope of DME
Durable Medical Equipment (DME) refers to medical devices designed for repeated use, serving patients with chronic conditions or long-term healthcare needs. These include wheelchairs, hospital beds, oxygen equipment, nebulizers, and prosthetics. For an item to qualify as DME, it must meet specific criteria: durability, medical necessity, and usability in a home or outpatient setting. Medicare defines DME as equipment that serves a medical purpose, is appropriate for home use, and can withstand repeated use without replacement. This definition shapes the reimbursement landscape across Medicare, Medicaid, and private insurance plans, requiring precise coding to ensure claims compliance.
Medicare and insurance providers follow strict rules to determine what qualifies for coverage. For example, Medicare requires documentation of medical necessity, supported by physician orders and diagnostic information, to justify DME claims. Equipment deemed for convenience or lacking adequate documentation can lead to denials. Private insurers often mirror Medicare’s guidelines but may have additional criteria or pre-authorization requirements. The key lies in understanding these coverage nuances and integrating them into every coding decision. For billing professionals, this knowledge translates into reduced claim denials and improved reimbursement rates.
Common Categories of DME Codes
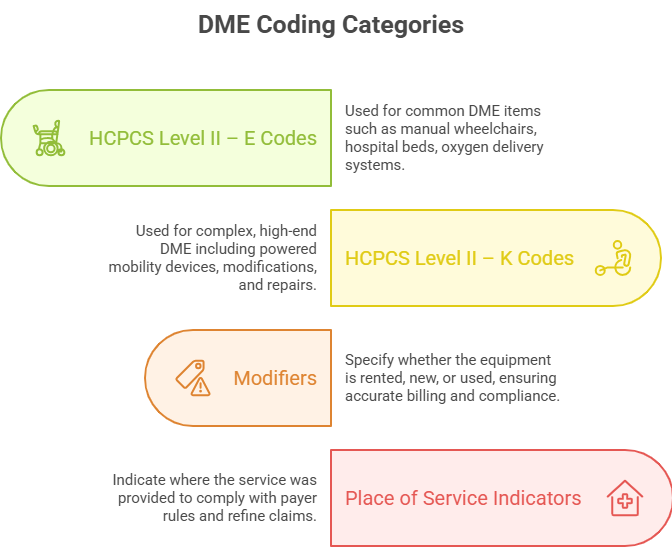
DME coding relies on HCPCS Level II codes, which identify specific equipment and services. The most commonly used codes for DME begin with E (e.g., wheelchairs, oxygen systems) and K (e.g., wheelchairs with power features, custom fittings). Modifiers add layers of specificity, such as rental vs. purchase, initial vs. replacement, or billing for repairs. Place of service indicators further refine claims by specifying where the service occurred—home, outpatient, or skilled nursing facility.
Accurate code selection involves matching the right HCPCS code with appropriate modifiers and place of service indicators. Errors, such as assigning the wrong code or misusing a modifier, can result in payment denials, delayed reimbursement, or compliance risks. Staying current with code updates and payer-specific rules is essential. Experienced coders leverage reference materials, payer guidelines, and EHR-integrated coding tools to minimize errors and optimize reimbursement. Mastery of DME code categories, modifiers, and service indicators forms the core of successful billing practices.
Key Challenges and Compliance Issues in DME Coding
Documentation Requirements
Documentation is the cornerstone of accurate DME coding and successful reimbursement. Every claim must be supported by detailed physician orders, medical necessity documentation, and proof of equipment delivery. These elements ensure that the equipment meets both Medicare and private insurer requirements. A common pitfall in DME coding is incomplete documentation, such as missing provider signatures, inadequate diagnostic support, or vague justifications for equipment use. Auditors and payers scrutinize these details closely; a single missing element can trigger denials or requests for additional information.
Avoiding audits starts with meticulous attention to paperwork. Providers must ensure that documentation aligns perfectly with HCPCS Level II codes and associated modifiers. For example, when billing for oxygen equipment, documentation should include arterial blood gas results or oxygen saturation levels to substantiate medical necessity. Inconsistent or unclear records increase the risk of denials and can damage the provider’s compliance standing. Regular internal audits and staff training help maintain high documentation standards, reducing error rates and improving reimbursement consistency.
Common Errors and How to Avoid Them
Several frequent errors in DME coding can jeopardize reimbursement and trigger audits. One major issue is mismatches between documentation and codes. For instance, submitting a code for a power wheelchair without supporting medical necessity documentation or with insufficient physician orders will almost certainly lead to denial. Another common error involves misuse of modifiers—incorrectly flagging rentals as purchases, omitting place of service codes, or applying modifiers that don’t align with the documentation.
To avoid these pitfalls, coders should implement standardized workflows that cross-check documentation against codes and payer requirements. Using EHR-integrated coding tools, conducting periodic training, and reviewing payer-specific guidelines can significantly reduce errors. Coders should also stay updated on policy changes affecting HCPCS codes and modifiers, particularly as Medicare and private insurers refine coverage criteria. Precision in coding and documentation ensures a steady revenue flow, enhances compliance, and mitigates audit risks.
| Key Challenge | Description | Solutions |
|---|---|---|
| Incomplete Documentation | Missing physician signatures, inadequate medical necessity proof, or unclear justifications. | Implement thorough documentation workflows, conduct internal audits, and ensure physician compliance. |
| Mismatches Between Documentation and Codes | Codes submitted without matching or sufficient supporting documentation (e.g., power wheelchair claims). | Cross-check documentation with codes, train staff, and use EHR-integrated tools to prevent errors. |
| Misuse of Modifiers | Incorrectly marking rentals as purchases, missing place of service codes, or misapplied modifiers. | Educate coders on modifier rules, stay updated on payer-specific guidelines, and review claims. |
| Policy and Coding Changes | Medicare and insurers updating criteria, which can lead to outdated or incorrect coding practices. | Stay informed on policy changes, update coding references, and retrain staff as needed. |
| Increased Audit Risk | Auditors scrutinize DME claims for compliance; errors or omissions can trigger audits or denials. | Implement proactive audit-prevention measures, maintain meticulous records, and track common errors. |
Mastering Reimbursement Strategies
Navigating Medicare Policies
Reimbursement for Durable Medical Equipment (DME) is tightly governed by Medicare policies, including Local Coverage Determinations (LCDs), which outline coverage rules for specific equipment categories. Each LCD specifies documentation requirements, qualifying diagnoses, and conditions under which the equipment is deemed medically necessary. Coders and billing professionals must be adept at interpreting LCDs to ensure claims align with these stipulations. Overlooking an LCD’s nuance can result in a denied claim, delaying payment and creating administrative burdens.
Medicare also mandates prior authorization for certain DME items, like power mobility devices. This process requires submitting detailed medical records and justifications before equipment delivery. If prior authorization is denied, providers must either appeal or absorb the cost—making proactive, accurate submissions critical. Appeals demand thorough documentation and references to LCDs or National Coverage Determinations (NCDs), along with precise citations from medical records. Mastering these processes elevates reimbursement accuracy and mitigates denials.
Optimizing Revenue and Reducing Denials
Consistent revenue in DME billing depends on strategic approaches that prioritize accuracy and compliance. One essential tactic is ensuring complete, precise claims submissions, with all required documentation, codes, and modifiers. This reduces the likelihood of denials or delays, accelerating reimbursement. Training staff to recognize and correct coding errors before submission is equally important. Regular refresher courses on HCPCS updates, modifier rules, and payer requirements foster a culture of precision.
Proactive denial management is another key strategy. When a claim is denied, swift investigation and resubmission with corrected information can recover revenue. Tracking denial patterns reveals systemic issues—whether in documentation, code selection, or modifier use—allowing for targeted corrective actions. Investing in coding technology, such as automated coding tools and EHR-integrated solutions, can also reduce human error and streamline the claims process. Ultimately, coders and billing professionals who master these strategies ensure financial stability and compliance for their organizations.
| Poll: What interests you most about DME coding? | |
|---|---|
Emerging Trends in DME Coding
Impact of Value-Based Care
The healthcare industry’s shift towards value-based care directly impacts DME coding and reimbursement practices. Under value-based models, providers are incentivized to improve patient outcomes while controlling costs. This shift demands meticulous DME coding that not only captures services provided but also aligns with quality measures and compliance mandates. Errors in documentation or coding can skew performance metrics, affect reimbursement rates, and reduce overall revenue. Coders must understand how to accurately document and code DME in alignment with value-based care requirements, ensuring their organization’s performance metrics remain strong.
Tech Innovations
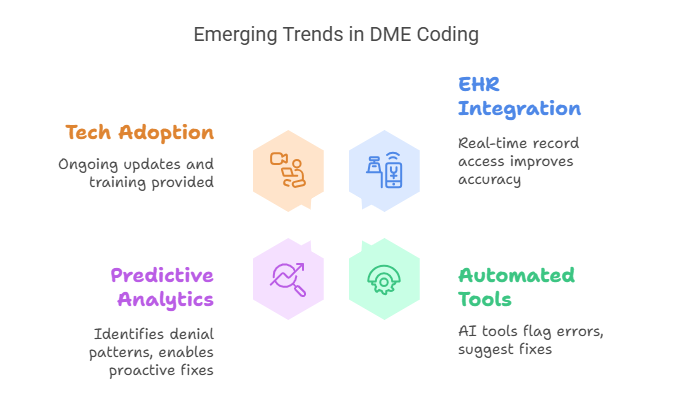
Technology is transforming DME coding by introducing electronic health records (EHR) integration and automated coding tools. These innovations streamline workflows, enhance coding accuracy, and reduce the likelihood of human error. EHR integration ensures coders have real-time access to complete patient records, enabling precise code assignment based on comprehensive data. Automated coding tools, powered by AI and machine learning, offer real-time validation of codes, flag inconsistencies, and suggest corrections before submission.
Another innovation is the use of predictive analytics to identify patterns in denials and coding errors. By leveraging these insights, organizations can preemptively correct issues, optimizing reimbursement and compliance. However, adopting new technologies requires thorough training to ensure coders can effectively use these tools. Staying updated on emerging technology trends ensures billing professionals remain competitive in a rapidly evolving landscape.
Mastering DME Billing Codes Through AMBCI’s Medical Billing & Coding Certification
Why Mastering DME Coding Matters
Mastering DME coding is more than just a technical skill—it’s a direct contributor to billing accuracy, compliance, and revenue optimization. Proper DME coding ensures claims are processed swiftly and accurately, reducing the risk of denials and compliance issues that can jeopardize an organization’s revenue stream. In today’s healthcare landscape, where regulations are increasingly complex, the ability to interpret coding guidelines, documentation requirements, and reimbursement policies is critical. Without precise DME coding, providers risk lost revenue, administrative burdens, and potential audit penalties, all of which impact financial stability and patient care quality.
Billing professionals who develop expertise in DME coding stand out in the field. Their skillset enhances revenue cycle management by streamlining claim submissions, reducing denial rates, and improving reimbursement accuracy. Mastery of DME coding not only benefits healthcare organizations but also boosts the career prospects of coders, making them invaluable assets in the billing workforce.
How AMBCI’s Program Equips You
The AMBCI Medical Billing and Coding Certification provides comprehensive training designed to equip professionals with the knowledge and tools to excel in DME coding. The curriculum covers HCPCS Level II codes, modifiers, Medicare and private insurance policies, documentation best practices, and emerging trends like EHR integration and automated coding tools. This program empowers coders to confidently handle complex billing scenarios, avoid common errors, and navigate reimbursement challenges with precision.
Graduates of AMBCI’s certification program not only gain in-depth knowledge but also benefit from ongoing support, resources, and access to industry updates. This ensures they remain current with evolving guidelines and technologies, enabling them to deliver consistent, accurate results for their organizations. By investing in the AMBCI Medical Billing and Coding Certification, billing professionals secure a competitive edge, elevating their expertise in DME coding and enhancing their contribution to healthcare compliance and financial success.
The Take Away
Durable Medical Equipment (DME) coding plays a pivotal role in ensuring healthcare organizations receive proper reimbursement for essential patient care equipment. This process involves not only selecting the correct HCPCS Level II codes and modifiers but also ensuring meticulous documentation, including medical necessity and physician orders. With regulations evolving and reimbursement models shifting towards value-based care, DME coding’s complexity and significance continue to grow. Errors or oversights in coding can lead to claim denials, revenue loss, and compliance risks, making coding proficiency indispensable.
Billing professionals who invest in advanced DME coding knowledge, such as through AMBCI’s Medical Billing and Coding Certification, position themselves as experts in an increasingly competitive landscape. Mastery of DME coding translates into improved revenue cycle management, reduced audit risk, and enhanced patient care quality. In an era where precision and compliance define success, specialized certification in DME coding isn’t just an asset—it’s a career-defining advantage.
Frequently Asked Questions
-
Durable Medical Equipment (DME) coding involves assigning precise HCPCS Level II codes to medical equipment prescribed for patients’ long-term health needs, such as wheelchairs, oxygen equipment, and prosthetics. Each code represents a specific item or service, ensuring accurate documentation and proper reimbursement from payers like Medicare, Medicaid, and private insurers. Precise DME coding is essential because it validates medical necessity, supports compliance, and secures timely payment. Errors in DME coding can lead to claim denials, delayed payments, and even audits, jeopardizing the provider’s financial stability and compliance with regulations. Mastery of DME coding is therefore vital for healthcare organizations and billing professionals alike.
-
HCPCS Level II codes are alphanumeric codes used to report products, supplies, and services not covered by CPT codes, which primarily cover medical procedures and services. In the context of DME billing, HCPCS Level II codes describe equipment and supplies like oxygen concentrators, wheelchairs, and prosthetic limbs. These codes typically start with letters such as “E” for DME or “K” for power mobility devices. CPT codes, in contrast, are reserved for services rendered by healthcare providers, including surgeries and office visits. Billing professionals must use HCPCS Level II codes for DME claims to ensure proper reimbursement and compliance with payer guidelines.
-
The most common documentation errors in DME claims include missing or incomplete physician orders, inadequate proof of medical necessity, and mismatches between documentation and the codes submitted. For example, failing to include oxygen saturation levels when billing for oxygen equipment, or omitting provider signatures on orders, can result in claim denials. Another frequent error is using outdated or incorrect HCPCS codes, leading to mismatched claims. To avoid these issues, billing professionals should implement standardized documentation workflows, regularly audit records, and ensure that all documentation aligns with coding and payer requirements.
-
Modifiers in DME coding add crucial details to HCPCS codes, indicating factors such as rental versus purchase, repair versus replacement, or specific service circumstances. For instance, modifiers like RR (rental) or NU (new equipment) clarify the nature of the claim, while UE (used equipment) signals reissued items. Using the correct modifiers ensures accurate reimbursement and avoids potential claim denials. Misuse or omission of modifiers is a common error that can trigger audits or revenue losses. Billing professionals must stay updated on payer-specific guidelines and coding updates to use modifiers effectively and maintain compliance.
-
Medicare’s prior authorization process requires providers to obtain approval for certain DME items before delivery, such as power mobility devices or high-cost prosthetics. The process involves submitting detailed medical records, including physician orders, medical necessity documentation, and supporting test results. If prior authorization is denied, providers must either appeal or absorb the equipment cost, which can significantly impact revenue. Timely and accurate submissions that meet Medicare’s guidelines are crucial to securing prior approval. This process not only safeguards reimbursement but also reduces the likelihood of audits and compliance risks for healthcare organizations.
-
EHR (Electronic Health Record) integration streamlines DME coding by providing coders with real-time access to comprehensive patient data, including medical history, diagnostic information, and provider notes. This seamless access ensures accurate code assignment based on complete documentation, reducing errors and improving claim accuracy. EHR systems can also integrate with automated coding tools, offering suggestions and flagging discrepancies in real time. The result is improved coding efficiency, fewer denials, and enhanced compliance with payer requirements. Billing professionals using EHR-integrated systems are better equipped to navigate complex coding scenarios and adapt to evolving healthcare regulations.
-
Billing professionals can reduce DME claim denials by implementing several key strategies:
Accurate Documentation: Ensure that every claim includes complete, clear, and accurate documentation aligned with the assigned codes and modifiers.
Training and Updates: Regularly train staff on coding updates, payer policies, and best practices.
EHR and Coding Tools: Leverage EHR-integrated systems and automated coding tools to minimize human error.
Pre-Submission Reviews: Conduct thorough pre-submission checks to catch errors before claims are sent.
Proactive Denial Management: Track denials, identify patterns, and implement corrective actions promptly.
By consistently applying these strategies, billing professionals can optimize reimbursement, maintain compliance, and strengthen financial performance.