Mastering Reimbursement Coding: Tips for Maximizing Healthcare Claims
Reimbursement coding plays a critical role in healthcare administration, ensuring medical services are accurately documented and billed. As healthcare regulations continue evolving in 2025, staying updated with coding practices is more important than ever. Accurate medical coding directly impacts the financial health of healthcare providers by ensuring timely reimbursements and minimizing claim denials.
In this comprehensive guide, we’ll explore advanced strategies to master reimbursement coding, highlight recent updates, and share expert tips to maximize your healthcare claims. From understanding the fundamentals of CPT and HCPCS codes to identifying common billing errors and the latest industry trends, this article covers everything you need to know.
What is Reimbursement Coding and Why Does It Matter?
Reimbursement coding involves translating healthcare services, procedures, and diagnoses into standardized codes used for insurance billing. These codes help healthcare providers communicate effectively with insurance companies to ensure appropriate payment for services rendered.
Key Benefits of Accurate Reimbursement Coding:
Ensures timely and accurate payments for healthcare services.
Minimizes claim denials by aligning with insurer requirements.
Supports compliance with healthcare regulations like HIPAA.
Enhances financial performance through efficient revenue cycle management.
In 2025, the medical billing industry faces new challenges and regulations, making accurate coding practices more critical than ever. According to the American Health Information Management Association (AHIMA), coding errors contribute to nearly 30% of claim denials annually. This underscores the importance of mastering reimbursement coding to protect your healthcare revenue.
The Latest Updates in Reimbursement Coding for 2025
Healthcare coding standards evolve yearly to reflect advancements in medical procedures and technology. In 2025, notable updates include:
1. CPT Code Revisions and Additions
The American Medical Association (AMA) has introduced several new CPT codes to address emerging healthcare services like telemedicine and remote patient monitoring. Notable additions include codes for AI-assisted diagnostics and virtual physical therapy consultations.
Tip: Regularly check the AMA CPT Code Updates to stay informed about new changes.
2. HCPCS Level II Code Adjustments
The Centers for Medicare & Medicaid Services (CMS) have updated HCPCS Level II codes to include new categories for home-based healthcare services and modern medical devices like wearable cardiac monitors.
Resource: Visit the CMS HCPCS Quarterly Updates for the latest information.
3. Telehealth Coding Enhancements
With telehealth becoming more mainstream post-pandemic, CMS has expanded the list of approved services for remote consultations. New codes distinguish between synchronous (real-time) and asynchronous (store-and-forward) telehealth interactions.
Understanding CPT and HCPCS Codes: The Backbone of Medical Billing
Accurate coding hinges on a clear understanding of Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes.
CPT Codes Explained
CPT codes are numeric codes that describe medical, surgical, and diagnostic services. They are essential for billing outpatient and office-based services.
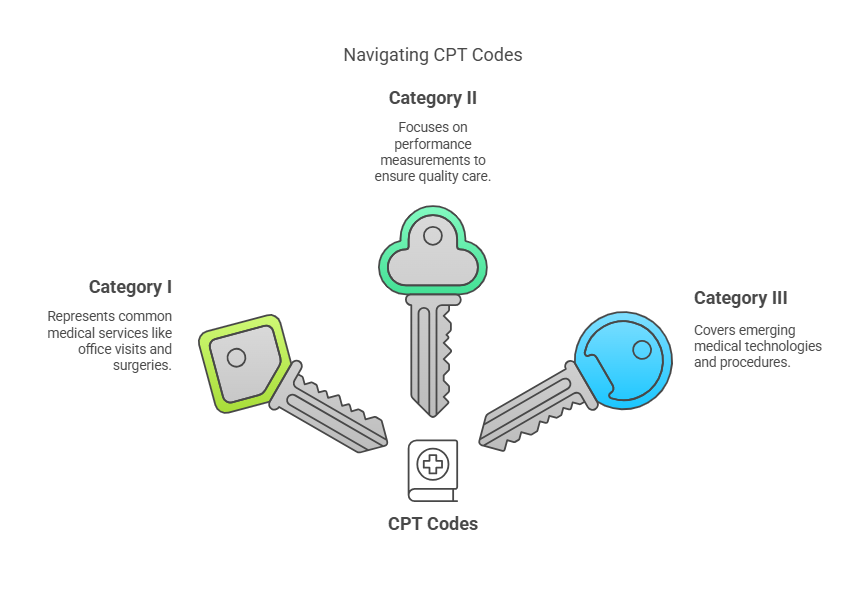
Key Categories:
Category I: Common services like office visits and surgeries.
Category II: Performance measurements for quality care.
Category III: Emerging medical technologies and procedures.
2025 Insight: In 2025, new CPT codes expand the scope of medical coding to cover procedures for personalized medicine, including gene-editing therapies and AI-supported radiology.
HCPCS Level II Codes Simplified
HCPCS codes go beyond CPT codes to cover non-physician services, including:
Medical equipment (e.g., wheelchairs)
Supplies (e.g., surgical masks)
Services like ambulance transportation
HCPCS Code Structure: Alphanumeric, starting with a letter (A-V) followed by four digits.
Tip: Stay updated with HCPCS changes by referencing the National Uniform Billing Committee (NUBC).
The Critical Role of Accurate Documentation in Reimbursement Coding
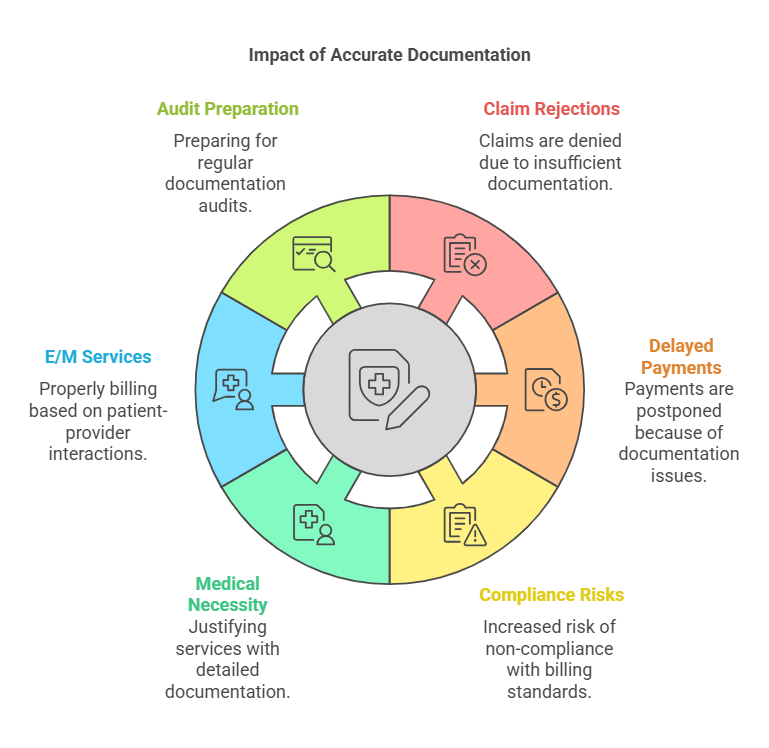
Accurate documentation is the foundation of successful medical billing. Incomplete or incorrect documentation can result in claim rejections, delayed payments, and compliance risks.
1. Medical Necessity Documentation
Insurers require documented evidence to justify the medical necessity of provided services. This involves detailing the patient’s symptoms, diagnosis, and the rationale behind the chosen treatment.
Example: For an MRI scan, documentation should explain why the scan was essential rather than relying solely on a patient’s reported symptoms.
2. Evaluation and Management (E/M) Services
E/M services describe patient-provider interactions like consultations and exams. Proper documentation ensures the correct E/M service level is billed.
2025 Update: CMS has revised E/M codes for virtual visits to distinguish between AI-assisted and human-only consultations.
3. Audit Preparation
Regular documentation audits help identify potential errors and ensure compliance with updated billing standards.
Action Step: Schedule quarterly audits to review documentation practices and address inconsistencies proactively.
Decoding Evaluation and Management (E/M) Codes: A Step-by-Step Guide
E/M codes are essential for reporting patient interactions accurately. Inaccurate use can lead to underbilling or claim denials.
Key Components for E/M Coding:
History: Patient's medical background and current symptoms.
Examination: Findings from the physical examination.
Medical Decision-Making (MDM): Complexity of evaluating and treating the patient.
Distinguishing New vs. Established Patients:
New Patient: No services from the provider in the past three years (e.g., CPT code 99202).
Established Patient: Services provided within the last three years (e.g., CPT code 99214).
Common Billing Errors and Strategies to Avoid Them
Billing mistakes can disrupt cash flow and lead to compliance penalties. Here are the most prevalent errors and how to prevent them:
1. Incorrect Code Usage
Cause: Misunderstanding code requirements or using outdated codes.
Prevention: Use certified medical coding software and refer to updated CPT and HCPCS manuals regularly.
2. Insufficient Documentation
Cause: Missing essential details like diagnosis codes or procedure notes.
Prevention: Train staff on documentation best practices and implement a standardized checklist.
3. Upcoding and Undercoding
Upcoding: Assigning a code for a more expensive service.
Undercoding: Using a less complex code, leading to revenue loss.
Prevention: Conduct random audits and educate staff on ethical coding practices.
The Growing Impact of Technology on Reimbursement Coding in 2025
The healthcare industry is increasingly adopting Artificial Intelligence (AI) and Machine Learning (ML) for medical billing and coding. These technologies automate code assignment, detect anomalies, and improve billing accuracy.
Key Trends to Watch:
AI-Driven Coding Software: Reduces manual workload and minimizes errors.
Blockchain for Medical Billing: Enhances data security and streamlines insurer-provider communication.
Telehealth Billing Innovations: New codes for remote monitoring and virtual care services.
Explore More: HealthIT.gov offers insights into digital healthcare advancements.
Best Practices for Healthcare Providers in Reimbursement Coding
1. Stay Informed on Coding Changes
Regularly check resources like the CMS and AMA websites for updates to CPT and HCPCS codes.
2. Invest in Staff Training
Provide ongoing training to coding professionals to maintain high accuracy levels.
3. Leverage Technology
Adopt AI-based coding tools and billing software to streamline processes and reduce manual errors.
4. Collaborate with Coding Specialists
Work with certified medical coders to navigate complex procedures and prevent compliance issues.
Conclusion: Future-Proofing Your Medical Coding Practices
As healthcare continues to evolve, mastering reimbursement coding remains essential for financial stability and regulatory compliance. By understanding the latest updates in CPT and HCPCS codes, prioritizing accurate documentation, and leveraging modern technology, healthcare providers can optimize their billing processes in 2025 and beyond.
Implement these strategies to reduce claim denials, ensure timely payments, and maintain a robust revenue cycle. Accurate medical coding is more than just a technical task—it’s a critical component of effective healthcare management.
Frequently Asked Questions (FAQs)
1. What is the main purpose of reimbursement coding?
Reimbursement coding ensures healthcare providers are accurately compensated by translating medical procedures into standardized codes for insurance claims.
2. How often are CPT and HCPCS codes updated?
CPT codes are updated annually by the AMA to reflect changes in medical procedures and technology, while HCPCS codes receive quarterly updates through CMS to accommodate new services, supplies, and equipment used in healthcare.
3. How can I avoid coding errors in 2025?
Stay updated on coding guidelines, invest in staff training, and use advanced coding software to reduce manual errors.
4. What role does AI play in medical coding today?
AI streamlines coding processes by automating code assignment, detecting anomalies, and improving billing accuracy.
5. Where can I learn more about reimbursement coding regulations? Visit the CMS Official Site or the American Health Information Management Association for the latest guidelines.