What Does A Medical Billing Specialist Do?
A medical billing specialist plays a vital role in the healthcare industry by ensuring healthcare providers are accurately compensated for their services. They manage billing processes, submit insurance claims, and handle payments, acting as a critical link between healthcare providers and insurance companies. Medical billing specialists create invoices, verify codes, and ensure claims are filed accurately, preventing claim denials and safeguarding the financial stability of healthcare facilities. Their work helps medical practices run smoothly, enabling them to focus on patient care.
Key Takeaways on the Role and Importance of Medical Billing Specialists
Medical billing specialists are responsible for managing billing processes, filing insurance claims, and ensuring accurate payment collections. They play an essential role in preventing claim denials, which can disrupt the revenue cycle of healthcare providers. A thorough understanding of medical terminology, coding systems, and billing software is crucial for success in this role. Additionally, certifications help enhance job prospects and credibility. The use of advanced technology, such as medical billing software and electronic health record (EHR) systems, streamlines billing processes, reduces errors, and supports timely payments, all of which contribute to improving patient care.
Defining the Role of a Medical Billing Specialist
Medical billing specialists are responsible for overseeing medical billing, insurance claims, and ensuring prompt payments in healthcare institutions. From the moment a patient enters a clinic to the point where all medical bills are settled, these specialists ensure the entire billing process runs efficiently. They handle the documentation of services rendered, verify billing codes, and maintain accurate records to prevent errors that could lead to claim denials. They serve as intermediaries between healthcare providers and insurance companies, navigating regulatory requirements throughout the billing sequence.
Core Responsibilities of Medical Billing Specialists
The responsibilities of a medical billing specialist include creating bills, filing insurance claims, and overseeing the payment process. They are responsible for accurately coding healthcare services to ensure proper invoicing. They also manage billing issues and verify that codes used on claims accurately represent patient procedures. Attention to detail is crucial in this role, as even small errors can lead to delayed payments or claim rejections. Billing specialists must have a deep understanding of coding systems and insurance guidelines to ensure correct billing practices.
Essential Skills for Accuracy
To succeed as a medical billing specialist, one must possess a solid understanding of medical terminology and coding systems. A strong grasp of mathematical principles is necessary for calculating co-payments and resolving outstanding balances. Communication skills are also critical, as billing specialists must interact with patients, healthcare providers, and insurance companies. Additionally, knowledge of industry-specific codes and regulations is vital to ensure compliance and prevent claim denials. Analytical skills are essential for identifying and resolving billing discrepancies efficiently.
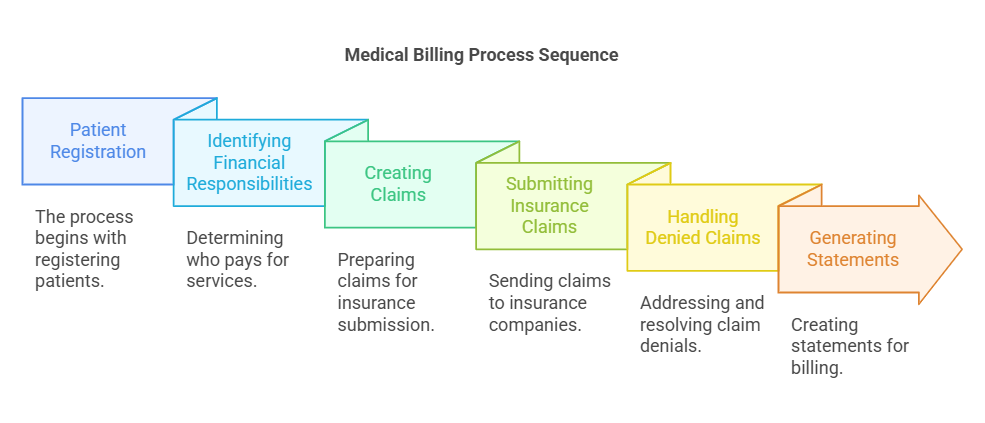
The Medical Billing Process
The medical billing process begins with patient registration and ends when all bills are paid. The process includes identifying the financial responsibilities of patients, creating claims, and generating statements. Medical billing specialists must maintain precision at each stage to ensure regulatory compliance. Electronic Health Records (EHR) systems and medical billing software streamline this process by facilitating data management and improving communication, reducing the chances of errors.
Submitting Insurance Claims and Handling Denied Claims
Medical billing specialists are responsible for submitting insurance claims to insurance companies, adhering to strict protocols to ensure timely reimbursement. Accurate claim submissions are critical to preventing delays in payment. When claims are denied, billing specialists must review the denial reasons, collaborate with medical coders, and resubmit the corrected claims. Their role in resolving denied claims is essential for maintaining the financial health of healthcare organizations.
Working with Medical Coding Specialists
Medical billing specialists work closely with medical coding specialists to ensure the accurate translation of diagnoses and procedures into standardized codes. This collaboration ensures that all claims are correctly coded and that healthcare providers are reimbursed for their services. Communication between billing and coding specialists is vital to minimize errors and ensure accuracy.
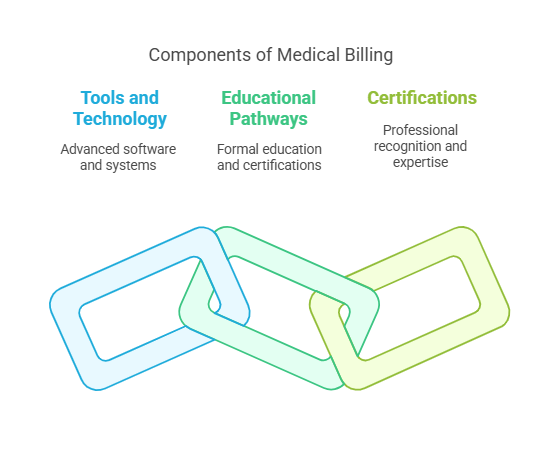
Tools and Technology in Medical Billing
Technology plays a significant role in medical billing. Advanced billing software and EHR systems improve the efficiency and accuracy of the billing process. These tools help automate tasks, track performance, and reduce errors. For example, PracticeSuite is a popular platform that streamlines the entire billing cycle, from claim denials to payment tracking.
Educational Pathways and Certifications
To become a medical billing specialist, one must pursue formal education in medical billing and coding. Certification programs, such as the Certified Professional Coder (CPC) or Certified Professional Biller (CPB), enhance career prospects and provide formal recognition of expertise. Ongoing education is necessary to stay updated on changes in healthcare regulations and billing standards.
Career Opportunities and Advancement
The demand for medical billing specialists is growing, with a projected 8% increase in employment from 2021 to 2031. This growth is driven by the aging population and the increasing complexity of healthcare services. Medical billing specialists can advance their careers by obtaining specialized certifications, such as the Certified Professional Medical Auditor (CPMA) or Certified Revenue Cycle Professional (CRCP). These advanced certifications open up additional career opportunities and higher earning potential.
Impact of Medical Billing Specialists on Healthcare
Medical billing specialists, certified through medical billing and coding certification programs like AMBCI, are crucial for ensuring the financial stability of healthcare institutions. By accurately processing claims, they reduce administrative burdens and expedite the reimbursement process. Their work allows healthcare providers to focus more on patient care and less on financial matters. Efficient billing practices also enhance revenue cycle management, ensuring timely payments and promoting financial sustainability in healthcare organizations.
6 Less Known Facts About Medical Billing Specialists
Medical billing specialists must stay current with frequent changes in healthcare regulations and insurance policies.
Source: American Academy of Professional Coders (AAPC) - Staying Up-to-Date with Healthcare Regulations
Some billing specialists specialize in certain types of insurance, such as Medicare or Medicaid, which requires specific knowledge of those programs.
The growing use of telemedicine has expanded the role of medical billing specialists to include virtual consultations and non-physician services.
Medical billing specialists can often work remotely, as the job primarily involves managing electronic records and insurance claims.
Entry-level medical billing specialists can advance to roles such as revenue cycle manager or medical billing supervisor with experience and additional certifications.
The rise of artificial intelligence in healthcare billing is gradually automating some of the more repetitive tasks, improving accuracy and efficiency.
Frequently Asked Questions (FAQs)
-
Medical billing specialists are responsible for creating invoices, filing insurance claims, managing payments, and resolving any billing issues that arise. They ensure that healthcare providers are accurately reimbursed for their services.
-
Essential skills include a strong understanding of medical terminology, knowledge of coding systems, attention to detail, communication skills, and basic math proficiency.
-
Aspiring medical billing specialists can pursue a diploma or degree in medical billing and coding. Professional certifications such as the Certified Professional Coder (CPC) can also enhance career prospects.
-
Medical billing specialists review denied claims, identify the reasons for denial, and work with insurance companies to resolve discrepancies and resubmit the claims.
-
Medical billing specialists ensure that healthcare providers are paid accurately and promptly, which supports the financial health of healthcare organizations. Their work reduces administrative burdens, enhances revenue cycle management, and ultimately improves patient care.