Top Medical Coding Billing Course: Your Path to Certification Success
Let's be real—medical coding and billing might not sound like the most thrilling career at first. But what if I told you it’s like being the secret agent of the healthcare industry? You’re the one who deciphers complex medical data, translates it into universal codes, and ensures that doctors get paid (which, trust me, they appreciate). Plus, you can work from home, earn a great salary, and never worry about job security. Now, doesn’t that sound like the best-kept career secret? Keep reading, and let’s unlock the world of medical coding and billing together!
people doing medical billing and coding
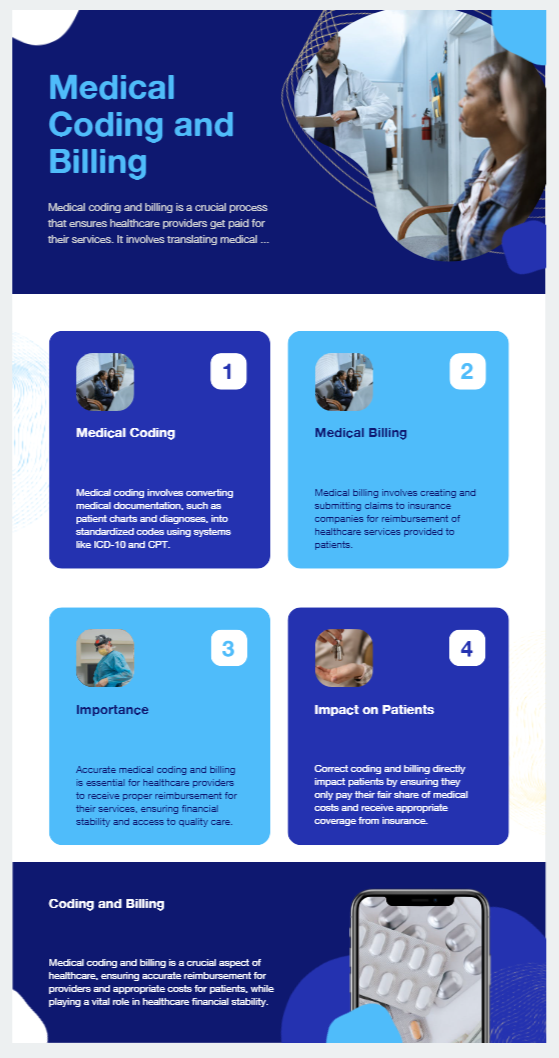
What is Medical Coding and Billing?
Medical coding and billing, along with medical coding and billing certification, is the life support of the revenue cycle in healthcare. It means translating medical diagnoses, procedures, services, and equipment into standardized codes, so that they can be used on insurance claims for reimbursement. Without proper coding and billing, hospitals and clinics would have no means of obtaining payment, and there would be financial chaos in the industry.
Here’s a quick breakdown of the two crucial roles:
Medical Coding: Assigns standardized codes (ICD-10, CPT, HCPCS) to medical diagnoses and procedures.
Medical Billing: Prepares and submits claims to insurance companies, ensuring that healthcare providers are paid accurately and on time.
In 2025, this field is more complex than it has ever been, incorporating AI-assisted coding software, automated billing systems, and compliance with ever-changing regulations. That’s why it is important to stay current, enroll in the best medical coding and billing classes, and become certified!
medical billing and coding impact
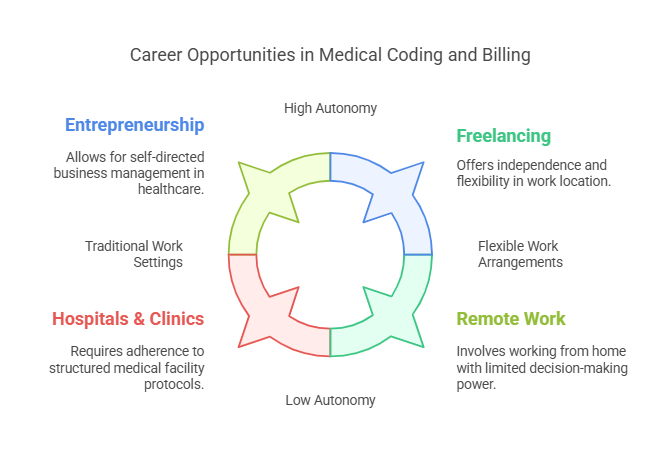
Career Opportunities in Medical Coding and Billing
The demand for trained medical coders and billers is rising, the Bureau of Labor Statistics expecting a 9 percent job growth rate by 2033. This profession has become indispensable due to the digital transformation of healthcare records and the increasing complexity of insurance claims.
Where Can You Work?
Hospitals & Clinics – Work in fast-paced medical environments handling patient data.
Insurance Companies – Review and process medical claims.
Government Agencies – Ensure compliance with healthcare policies.
Remote Work & Freelancing – Work from home as an independent coder.
Entrepreneurship – Start your own billing business and serve healthcare providers.
career opportunities for medical billing and coding
Specialized Career Paths
You don’t have to stick to general coding—specialization can make you an expert in fields like:
Oncology Coding – Handling complex cancer treatments.
Pediatric Coding – Managing children’s healthcare services.
Emergency Room Coding – Processing urgent care and trauma cases.
Auditing & Compliance – Ensuring that coding meets strict legal standards.
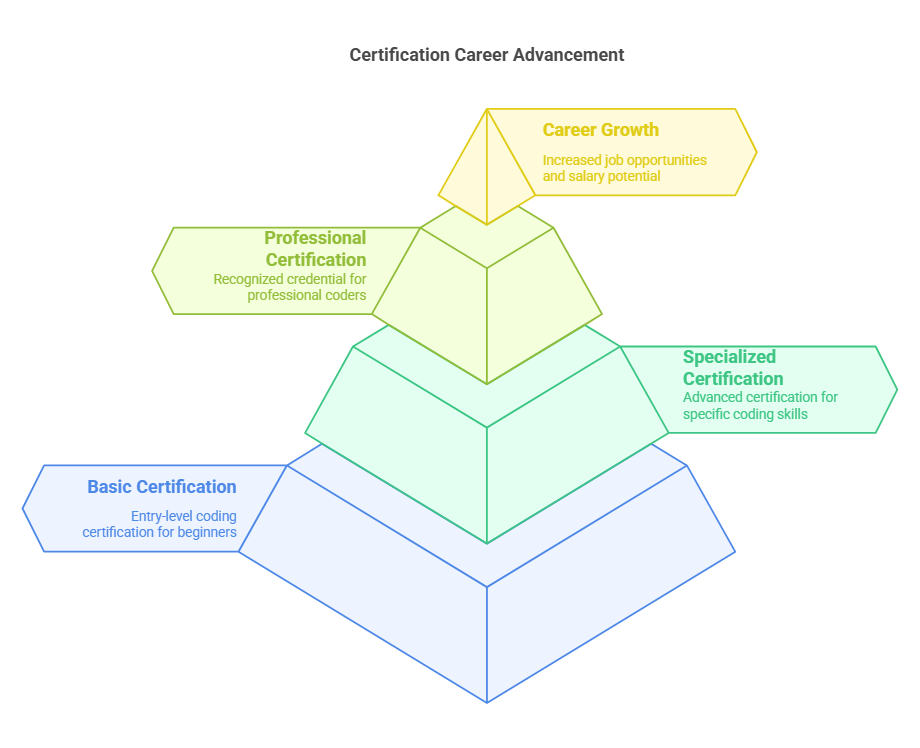
Why You Should Get Certified in 2025
You need expertise certifications to prove it and significantly increase your earning potential. Employers value certified coders and some won't hire without it.
The Top Certifications to Consider:
Certified Professional Coder (CPC) – AAPC
Certified Coding Specialist (CCS) – AHIMA
Certified Billing & Coding Specialist (CBCS) – NHA
Certified Inpatient Coder (CIC) – AAPC
Certified Outpatient Coder (COC) – AAPC
As for every certification, there is one that is most relevant to your career path so pick the one that fits what you want to achieve in 2025. The CPC remains the most recognized and most sought after credential in 2025.
career advancement
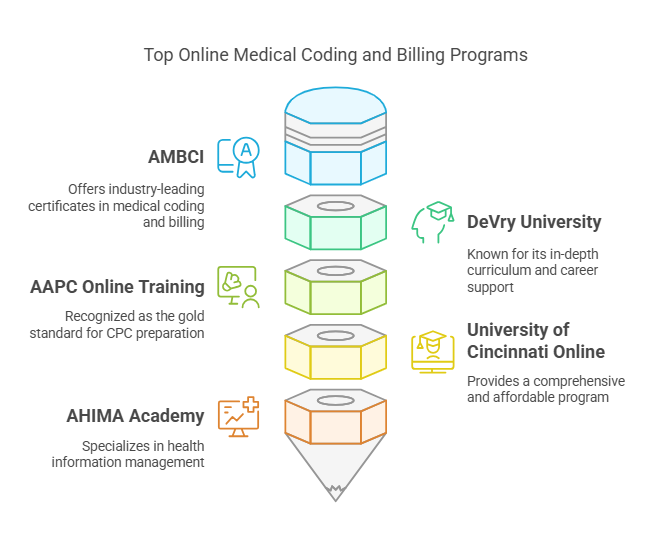
Best Online Medical Coding and Billing Courses
Online courses have transformed the learning experience, allowing flexibility without compromising on quality. Some of the top-rated online programs in 2025 include:
AMBCI– Industry-leading medical coding and billing certificates.
DeVry University – Known for its in-depth curriculum and career support.
AAPC Online Training – The gold standard for CPC preparation.
University of Cincinnati Online – Offers a comprehensive and affordable program.
AHIMA Academy – Specializes in health information management.
FAQs About Medical Coding and Billing
-
Not if you choose the right training! It’s detail-oriented work, but anyone with determination and good organizational skills can succeed.
-
Most certifications take 4-12 months, depending on your study pace and course type.
-
Absolutely! Remote medical coding is more popular than ever, with many companies hiring certified coders for work-from-home positions.
-
In 2025, the average salary is $48,780, with experienced professionals earning over $70,000+.
-
No! A certification is enough to land a great job in this field.
-
The Certified Professional Coder (CPC) is widely recommended for newcomers.
-
Nope! AI assists coders but doesn’t replace human expertise. Professionals are still needed to interpret medical records and ensure compliance.
-
Oncology and inpatient coding are among the highest-paying and most in-demand specializations in 2025.
10 Lesser-Known Facts About Medical Coding and Billing
The ICD-10 coding system has over 70,000+ codes!
While the exact number of codes in ICD-10 is not explicitly stated in the search results, ICD-10 is known for its expanded code set compared to its predecessor, ICD-9, which significantly increased the specificity and number of codes available for diagnoses and procedures.
Live Link: https://www.aapc.com/resources/what-is-icd-10
Medical coding is used for disease tracking and research, not just billing.
Medical coding systems like ICD-10 are used not only for billing but also for tracking diseases, statistical analysis, and research. They provide standardized data that can be used for various purposes beyond billing.
Live Link: https://www.linkedin.com/pulse/medical-coding-process-staffingly-1e
Some coders earn six figures with the right specialization.
A coding mistake can cost thousands—accuracy is crucial.
Coding errors can indeed be costly. A survey found that many medical bills contain errors, which can lead to financial losses for healthcare providers.
The first-ever medical code dates back to England in the 17th century.
AI and machine learning now assist coders in identifying billing errors.
AI technologies such as NLP and machine learning are increasingly used to assist in medical coding and billing by automating tasks, improving accuracy, and reducing errors.
Live Link: https://etactics.com/blog/will-medical-billing-and-coding-be-replaced-by-ai
Some coders work for the FBI, investigating healthcare fraud.
Outsourcing medical coding is a billion-dollar industry.
Many coders start their own businesses after a few years.
Coding skills can transfer to data analytics and IT jobs in healthcare.
The skills acquired in medical coding can be transferable to other roles in healthcare, such as data analytics and IT, due to the technical and analytical nature of the work
Live Link: https://www.vlmshealthcare.com/news/expanding-the-scope-of-medical-coders-beyond-coding
Conclusion: Your Next Step Towards Certification
The future of medical coding and billing is brighter than ever. Whether you're starting fresh or looking to advance your career, getting certified in 2025 is your best move. With high demand, excellent salary potential, and remote work opportunities, this is one of the smartest career paths in healthcare.
If you're serious about securing the best certifications, check out AMBCI Certification Institute—your gateway to becoming a top-tier medical coding and billing professional!