Advanced Billing & Coding for Interventional Radiology
In interventional radiology (IR), accurate billing and coding aren’t just back-office tasks—they directly affect revenue integrity and compliance. The complexity of image-guided procedures, bundled services, and evolving payer guidelines makes coding in IR one of the most detail-intensive segments in healthcare. Without precision, even high-volume practices risk claim denials, underpayments, or audits.
This guide offers a practical breakdown of advanced billing strategies and coding best practices tailored to interventional radiology. You’ll learn how to correctly assign CPT, HCPCS, and ICD-10 codes, avoid the most common billing errors, and optimize reimbursement workflows through documentation and payer alignment. Whether you’re a medical coder, billing specialist, or radiology practice manager, this resource will help you navigate IR billing with clarity and control—backed by the precision today’s revenue cycle demands.
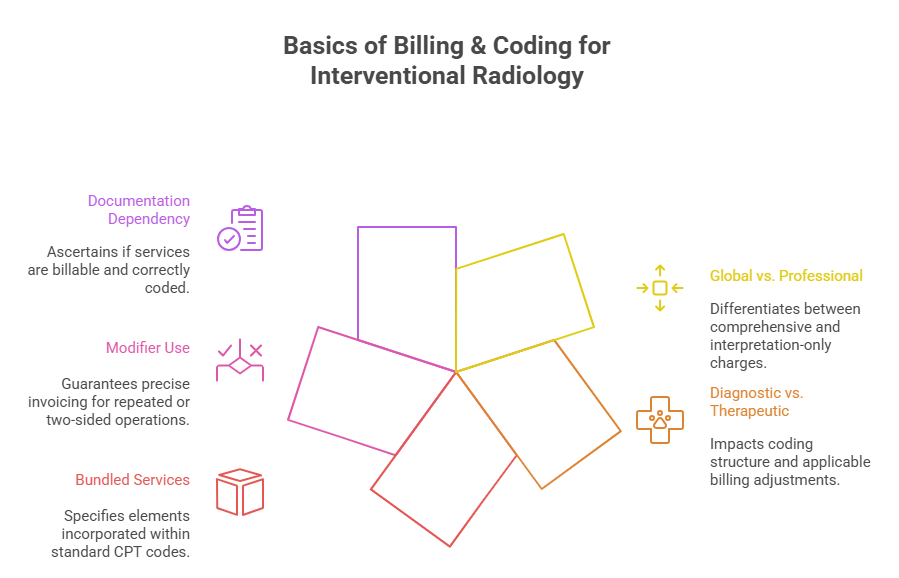
Understanding the Basics of Billing & Coding for Interventional Radiology
Interventional radiology (IR) blends diagnostic imaging with minimally invasive procedures—making its billing landscape uniquely complex. Unlike general radiology, IR often involves multiple components: imaging guidance, device usage, procedural work, and post-procedure care. Billing professionals must determine whether services are bundled or separately reportable and understand global vs. professional components when assigning codes.
IR coders must also distinguish between diagnostic and therapeutic intent. For example, a diagnostic angiogram followed by a stent placement may be billed differently than a therapeutic-only encounter. These nuances require deep familiarity with coding hierarchies and procedural anatomy. Mastering the fundamentals of IR billing sets the stage for applying advanced coding techniques without risking compliance issues or missed reimbursement.
The Role of Interventional Radiologists in the Billing Process
Although physicians aren’t responsible for coding, their role is pivotal. Accurate documentation from the interventional radiologist drives clean claims. Providers must detail procedure location, imaging guidance used, devices deployed, access sites, and procedural endpoints.
When physicians omit key details—such as bilateral involvement or selective catheterization levels—coders lack the clarity needed to bill correctly. Collaboration between coding teams and IR physicians ensures that operative reports align with documentation standards and payer requirements. Practices that train their providers to dictate with coders in mind significantly reduce denials, delays, and audit risks.
Common Procedures and Their Codes
IR coding often includes procedures like angioplasty, embolization, thrombolysis, and image-guided biopsies. Each of these has a distinct CPT structure tied to complexity, imaging use, and intent. For instance, embolization coding varies by target location, approach, and number of vascular territories treated.
Coders must know when to apply add-on codes for catheter placement, imaging, and sedation. Misusing or omitting these codes results in underbilling. Familiarity with core CPT ranges—such as 36200–37299—and understanding modifiers like -59, -LT, or -RT is essential. Every code chosen must reflect the full procedural scope and align with payer-specific bundling policies.
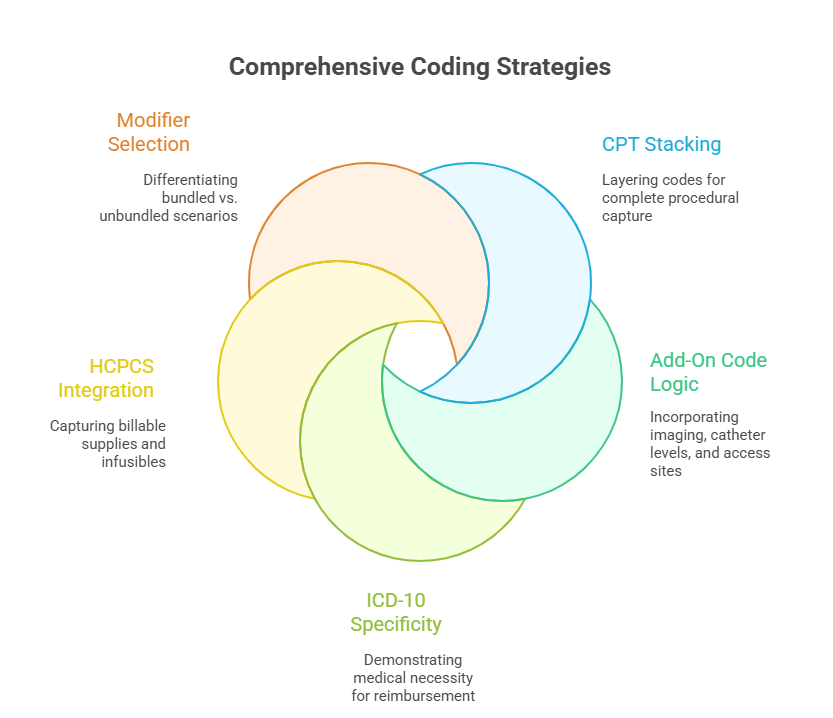
Advanced Coding for Interventional Radiology Procedures
Advanced interventional radiology (IR) coding requires a layered understanding of procedural logic, sequencing, and medical necessity. It’s no longer enough to assign a primary CPT and move on. Each procedure may involve multiple vascular territories, varying catheter placements, and intraoperative decisions—all of which affect code selection. Coders must read beyond the surface of op reports and look for decision points that shift documentation from a base code to one with multiple add-ons or modifiers.
Bundling and unbundling rules vary across payers. National Correct Coding Initiative (NCCI) edits must be checked for all combinations. Coders should also use modifier -XU, -XS, or -59 appropriately when services are distinct, especially when imaging is separately billable. Mistakes in these areas don’t just lead to denials—they can trigger audits or recoupments.
Correct Use of ICD-10 Codes
ICD-10 codes support the medical necessity of IR procedures. They explain why the procedure was performed, not what was done. In interventional radiology, precision in diagnostic coding is critical, especially when multiple conditions are treated simultaneously.
Each ICD-10 code should reflect the exact clinical scenario: location of pathology, laterality, and disease specificity. Vague or non-specific codes often result in claim rejections or medical review. For example, coding “peripheral artery disease, unspecified” instead of “atherosclerosis of native arteries of extremities with intermittent claudication” affects both reimbursement and risk scoring. Coders must follow payer policies and ensure that diagnostic codes align perfectly with the documented procedure.
CPT and HCPCS Codes in Interventional Radiology
CPT codes are the backbone of procedural billing, but in IR, code stacking is common. This involves layering base procedures (e.g., embolization) with selective catheter placements, fluoroscopic guidance, and vascular access coding. Knowing when codes are inclusive versus separately billable is essential.
HCPCS Level II codes add another layer—especially for contrast media, catheters, guidewires, and infusion drugs. While not all commercial payers require them, Medicare often does. Coders must identify billable supply codes and bundle them appropriately with the primary CPT, or report them separately when allowed. Cross-referencing CPT/HCPCS use with payer-specific billing manuals is a must for maximizing compliant reimbursement.
Common Billing Errors in Interventional Radiology
Interventional radiology billing demands absolute precision—and even experienced coders make costly mistakes. These errors often arise from misinterpreting bundled procedures, misapplying modifiers, or relying on vague documentation. Since IR often combines diagnostic imaging, surgical technique, and follow-up, misunderstanding procedural intent can result in duplicate billing or missed revenue.
The complexity of IR coding means mistakes aren’t always obvious. A single incorrect modifier, an unreported add-on, or choosing a global rather than professional-only code can lead to claim denials. More importantly, repeated errors invite payer audits, clawbacks, or even fraud investigations. Knowing where coders most often go wrong is the first step to correcting workflow gaps and boosting compliance.
Misuse of Codes and How to Avoid It
Code misuse often stems from assuming CPTs are universally billable. In IR, many services are bundled by default. Imaging guidance is one of the most commonly misunderstood areas—it’s often included in the main CPT, not separately billable. Similarly, catheter placement codes are frequently over-reported due to misreading access levels.
To avoid misuse, coders should:
Cross-check CPT codes against NCCI edits
Verify payer-specific bundling rules
Reference op reports for exact anatomical sites
Use correct modifiers only when clinically and technically justified
Training teams to read IR reports with a coder’s lens is critical. When coders know where to look, they catch omissions that damage claim integrity.
Incomplete Documentation
Even the best code choice fails without proper documentation. IR procedures require highly detailed operative reports, especially when multiple vessels, access points, or imaging modalities are involved. Coders often struggle when reports are vague, missing time elements, or don’t list all components clearly.
Incomplete documentation leads to:
Underbilling due to missing add-ons
Overbilling due to guesswork
Delays in claim approvals from payer queries
To resolve this, coders should collaborate with IR providers to clarify report structure. Templates can help ensure every element needed for accurate coding is captured—from device use to laterality. Better documentation means cleaner claims, faster reimbursement, and reduced post-payment reviews.
Optimizing Reimbursement for Interventional Radiology Services
Maximizing revenue in interventional radiology requires more than accurate coding—it demands strategic alignment of documentation, billing workflows, and payer requirements. With IR’s complex procedures, even minor oversights can result in thousands in lost revenue per claim. Practices that succeed financially are the ones that code proactively, document with reimbursement in mind, and stay current with evolving payer edits.
This section breaks down the two most controllable factors that influence reimbursement outcomes: precise documentation and payer-specific billing knowledge. Together, they empower coders and billing teams to not only defend revenue but to capture its full potential—without triggering compliance issues.
Proper Documentation for Higher Reimbursement
Payers reimburse based on what’s documented—not what was done. That means every access site, imaging technique, device use, and anatomical detail must be explicitly stated in the operative report. Radiologists should describe:
Whether the procedure was diagnostic or therapeutic
The level of catheterization (non-selective, selective, super-selective)
All imaging modalities used and their purpose
Use of structured templates ensures consistency and reduces the chances of missing billable components. Encouraging IR providers to dictate with coders in mind directly increases reimbursement. Every detail is a line item on the claim—and when it’s missing, revenue is lost.
Understanding Payer Policies
No two payers handle interventional radiology the same way. Commercial carriers often bundle services differently than Medicare, and Medicaid may follow its own rules entirely. Practices must develop internal billing guides that reflect carrier-specific policies on:
Bundled vs. unbundled imaging
Frequency limitations on repeat procedures
Requirements for modifier usage
Coverage of HCPCS supply codes
Keeping a current library of payer bulletins, LCDs, and denial trends allows coders to stay ahead of the curve. Regular crosswalks between op reports, CPT updates, and real-time denial patterns help billing teams respond, adapt, and recover faster. Reimbursement optimization starts with staying alert to how each payer behaves.
| Strategy | Benefit |
|---|---|
| Structured Documentation | Captures all procedural elements needed to bill fully and compliantly. |
| Provider-Coder Collaboration | Reduces missing details and improves coding accuracy from the start. |
| Payer Policy Tracking | Ensures code usage and documentation meet carrier-specific expectations. |
| Add-On Code Monitoring | Avoids underbilling by capturing all supporting services and components. |
| Denial Trend Analysis | Identifies patterns to improve future claims and recover lost revenue. |
Leveraging Technology for Improved Billing and Coding Accuracy
Manual coding in interventional radiology increases the risk of errors, delays, and missed revenue. With evolving payer rules and multi-layered procedures, technology is no longer optional—it’s a scalability and compliance tool. Automating key parts of the billing process ensures consistency, reduces human error, and accelerates reimbursement cycles.
Today’s IR practices leverage multiple systems to improve performance:
Computer-Assisted Coding (CAC) pulls structured data directly from reports and matches it with appropriate CPT/ICD codes.
AI-driven tools flag documentation gaps, suggest modifiers, and validate code combinations against NCCI edits.
RCM dashboards and analytics tools help track claim approval rates, denials by reason, and payer-specific trends in real time.
Technology also bridges communication between coders and providers. Integrated platforms allow radiologists to dictate within structured templates, which sync directly into EHRs and billing systems. This eliminates duplication and preserves coding integrity at every handoff.
For optimal results, IR groups should:
Train coding staff to audit CAC output for accuracy
Integrate claim scrubbers before submission to catch payer mismatches
Regularly update coding software with current payer rules and CPT updates
Leveraging these systems doesn’t replace coders—it elevates their role into analysts and claim strategists. The result? Fewer rejections, faster payments, and a billing operation that scales with case complexity.
| Tool or System | Function |
|---|---|
| Computer-Assisted Coding (CAC) | Suggests CPT and ICD codes from structured clinical documentation. |
| Claim Scrubbers | Detects code conflicts, modifier issues, and payer mismatches before submission. |
| EHR Integration | Transfers provider dictation and templates into coding platforms efficiently. |
| Analytics Dashboards | Tracks approval rates, denial reasons, and real-time revenue performance. |
| AI Modifier Assistants | Flags incorrect or missing modifiers based on op report analysis. |
How the AMBCI Medical Billing and Coding Certification Elevates IR Billing Accuracy and Career Growth
In interventional radiology, billing isn’t just complex—it’s high-stakes. The AMBCI Medical Billing and Coding Certification equips coders with the precision, compliance mindset, and procedural fluency needed to thrive in this demanding specialty. It goes beyond theory, offering coders real-world frameworks for managing IR workflows, payer variations, and documentation alignment.
The AMBCI curriculum emphasizes:
Anatomy-specific code mapping
Diagnostic-vs-therapeutic coding distinctions
Modifier logic tailored to radiology scenarios
Fraud prevention strategies and audit readiness
This is especially valuable in IR, where procedures often involve overlapping services and gray areas in code hierarchy. Certified coders are trained to analyze operative reports critically, choose correct CPT/HCPCS combinations, and align claims with payer expectations—without leaving revenue on the table.
Beyond skill-building, the AMBCI certification also boosts earning potential and job access. Many hospitals, radiology groups, and third-party billing firms now prioritize certified applicants for IR-focused coding roles. It also opens the door to consulting, auditing, or lead coding positions within multi-specialty practices.
For anyone managing IR billing or seeking to specialize in radiology coding, AMBCI offers not just training—but career leverage that directly translates into higher accuracy and stronger reimbursement performance.
Frequently Asked Questions (FAQs)
-
Interventional radiology (IR) combines diagnostic imaging with therapeutic procedures—often in the same session. This introduces multiple variables: catheter placements, fluoroscopic guidance, device usage, and varying procedural intents. Unlike diagnostic radiology, IR often requires the coder to evaluate selective vs. non-selective vascular access, procedural staging, and device deployment. Each component has unique CPT rules, modifier needs, and bundling logic. Payers frequently change policies regarding what is separately billable. Because IR reports are dense and vary by physician, billing professionals need procedural fluency and strong documentation analysis skills. Without these, it’s easy to undercode, overbill, or trigger audits—making IR one of the most demanding coding specialties.
-
For vascular IR procedures, CPT codes typically range from 36200–37299, covering catheter placement, angiography, embolization, thrombolysis, stent placements, and more. Nonvascular procedures—such as image-guided biopsies or drainages—fall into the 50000–60000 series. Coders must know which services are bundled within these CPTs and when to use add-on codes for imaging, guidance, or multiple territories. IR coding often requires stacking codes appropriately and appending modifiers like -59, -XS, or -RT/-LT when necessary. Staying current with CPT updates and payer edits is critical. Misuse of codes in these ranges leads to denials or reduced reimbursement—even when the procedure was performed correctly.
-
Always query the provider. In interventional radiology, even small gaps in documentation can lead to incorrect code selection. If the operative report lacks details like access route, vessel selection, laterality, or device use, coders should reach out for clarification. Use structured query forms and maintain a professional tone—focus on clarification, not correction. You can also implement standardized IR dictation templates that prompt providers to include critical elements. Educating physicians on what coders need to support compliant billing can reduce repetitive errors. The cleaner the initial documentation, the fewer delays and denials you’ll face in the billing cycle.
-
The top reasons include: using a CPT code that’s bundled under NCCI edits, misapplying modifiers, submitting incomplete documentation, and failing to establish medical necessity with the appropriate ICD-10 codes. Many denials stem from misunderstanding what’s included in the primary CPT versus what requires separate reporting. Some payers also require prior authorization for high-cost IR procedures. Others deny claims based on vague diagnosis codes or mismatched place-of-service details. To reduce denials, coders must stay current with each payer’s bundling edits, coverage policies, and modifier rules. Consistent internal audits can catch patterns before they impact revenue at scale.
-
Only in specific cases. Many IR CPT codes already include imaging guidance, especially for vascular access, catheter placement, or fluoroscopic guidance. Billing separately is only allowed when documentation supports a distinct, separately identifiable service not inherent to the primary procedure. This must be supported by clear notes and may require modifiers like -59 or -XS to bypass NCCI edits. For example, separately reporting ultrasound guidance for vascular access may be permissible if it’s not bundled with the main procedure. Coders should reference CPT parenthetical notes and payer-specific policies before submitting claims that split imaging from primary codes.
-
The Medical Billing and Coding Certification from AMBCI provides focused training in procedural coding logic, modifier application, and documentation review—all essential for IR coding. It equips coders with frameworks for analyzing complex op reports, managing payer policy differences, and avoiding common IR coding pitfalls. AMBCI emphasizes compliance, revenue protection, and structured audit readiness—skills that are especially critical in a high-risk specialty like IR. Many employers now prefer or require coders with certification for radiology-specific billing roles. In short, AMBCI doesn’t just help you pass an exam—it builds the operational judgment needed to bill IR procedures with precision and confidence.
-
Coders in IR benefit from computer-assisted coding (CAC) systems, especially those integrated with EHRs and dictation templates. These tools can auto-suggest CPT/ICD combinations based on keywords in the provider’s note, flag mismatches, and recommend modifiers. In addition, claim scrubbers, RCM analytics platforms, and payer-specific code-checking software reduce human error and accelerate approvals. Many organizations also use custom dashboards to track denials by code, payer, or reason, allowing faster resolution. The most effective workflows pair technology with coder oversight. Software should enhance—not replace—coder expertise. Coders who understand both the clinical and tech side of billing are more accurate and efficient.
Conclusion: Mastering Billing & Coding for Success in Interventional Radiology
Success in interventional radiology billing doesn’t come from generic coding knowledge—it comes from precision, specialty training, and real-time adaptability. With evolving payer rules, complex multi-component procedures, and risk-heavy documentation requirements, IR coding demands a level of fluency most specialties don’t. But that challenge is also the opportunity.
Coders and billing professionals who master IR processes position themselves as high-value, irreplaceable assets in the revenue cycle. Whether you’re applying structured CPT/HCPCS combinations, identifying missed modifiers, or aligning op reports with payer edits—every small win adds up to cleaner claims and stronger revenue protection.
Pairing this expertise with a specialized credential like the Medical Billing and Coding Certification from AMBCI gives you the credibility and confidence to lead. It’s not just about billing correctly—it’s about billing smart, billing defensively, and scaling with accuracy.
Mastering IR coding isn’t optional for long-term success—it’s the standard. And the professionals who embrace that standard are the ones who will thrive in the most advanced and lucrative segments of medical billing.