Career Roadmap to OIG Healthcare Compliance Auditor
An OIG Healthcare Compliance Auditor doesn’t just “check charts”—they protect program integrity, translate complex CMS rules into measurable controls, and turn denial data into recoveries and sanctions avoided. This roadmap shows you how to build the skills, artifacts, and credibility hiring managers expect, then execute a 12-month plan that proves ROI with audit-ready evidence. You’ll leverage AMBCI playbooks on compliance, modifiers, predictive analytics, and regulatory futures to build a portfolio that survives interviews and federal scrutiny alike—while keeping your career insulated from automation and policy shocks.
1) What an OIG Healthcare Compliance Auditor Actually Does (and Why Hiring Managers Care)
OIG auditors safeguard Program Integrity by testing whether coding, billing, and documentation conform to federal and payer rules—before penalties, extrapolated damages, or repayments hit. Strong candidates convert rulebooks into controls: risk-weighted sampling, prebill edit governance, appeal packet standards, and training that measurably decreases error rates. Build your base with AMBCI’s CMS compliance primer in this guide, then layer modifier risk techniques from modifier mastery and analytics thinking using predictive billing trends. To show interview-ready breadth, reference regulatory drifts from 2025–2030 changes and Medicare/Medicaid futures in this outlook.
Immediate pain points to master
Medical necessity vs. documentation gaps that trigger CARC 50—solve with evidence matrices and provider tip-sheets (calibrate with compliance trends).
Modifier misuse (25, 59, 76) causing overpayments—deploy red-flag audits built on modifier accuracy.
AI/CAC black boxes—mandate explainability and post-implementation precision/recall testing, guided by AI in RCM.
| Competency | Target KPI / Proof | Artifact You’ll Present | AMBCI Resource to Leverage |
|---|---|---|---|
| CMS policy mastery | 100% correct policy citations | Versioned SOP with citations & dates | CMS compliance guide |
| ICD/CPT/HCPCS accuracy | ≥97% in blinded audit | Pre/post accuracy trendline | Modifier mastery |
| Risk-based sampling | High-risk strata oversampled | Sampling plan with CARC linkage | Predictive analytics |
| Denial forensics | Top-10 CARC explained | Root-cause board & overturn rate | Certification strategy |
| HCC integrity | RAF lift with evidence | Suspect list + evidence trail | Compliance trends |
| E/M leveling | ≥95% concordance | Calibration huddle minutes | CPC roadmap |
| Prebill edit governance | False-positive rate ↓25% | Edit rule lifecycle log | AI-era skills |
| Appeal packet quality | >40% overturn | Payer-specific templates | Regulatory changes 2025–2030 |
| Education impact | Post-ed errors ↓30% | Micro-module deck + retest results | CE impact |
| HIPAA discipline | Zero major incidents | Access logs & CAPA register | CMS/HIPAA primer |
| ICD updates readiness | Issue-free go-live | Change-control dossier | ICD-11 guide |
| Remote audit ops | SLA ≥98% | Secure workflow SOP | Remote job trends |
| Cross-functional fluency | CDI/PFS alignment | RACI map | RCM manager guide |
| AI/CAC oversight | Explainable decisions | Precision/recall audit | AI in RCM |
| Modifier risk | 25/59 misuse ↓ | Hot-modifier watchlist | Modifier accuracy |
| State policy nuance | Zero state conflicts | State-by-state matrix | State breakdowns |
| Medical necessity | CARC 50 ↓ | Evidence checklist | Regulations & careers |
| Query governance | Turnaround <48h | Query dashboard | Career starter |
| Sampling defensibility | Reproducible math | Plan–Do–Check–Act log | Analytics trends |
| Overpayment protocol | Timely 60-day refunds | Refund tracker | CMS compliance |
| Education laddering | Skills → outcomes | Annual CE map | CPC ladder |
| Documentation strength | Audit-proof notes | Provider tip-sheets | Compliance trends |
| Appeal narrative | Template library | Packet exemplars | Medicare/Medicaid futures |
| Career positioning | Interview hit-rate ↑ | Portfolio site & case studies | Career roadmap |
| Geo market awareness | Offer quality ↑ | Comp analysis | California jobs |
| Future-proofing | Automation-resilient skills | Skill matrix vs tools | Future-proof roles |
2) 12-Month Roadmap: From Analyst to OIG-Ready Auditor
Days 0–30 — Baseline and Map Risk.
Inventory policies, edits, denials, and audit trails. Produce a single KPI deck: accuracy, first-pass yield, CARC top-10, query turnaround, and refund timeliness. Study ICD-11 change patterns with this infectious-disease guide. Benchmark your market using state breakdowns and remote trends in this article to set goals and compensation targets.
Days 31–60 — Install Controls.
Publish a risk-weighted sampling plan; tune prebill edits to cut false positives using precision/recall tracking. Build payer-specific appeal templates with evidence citations informed by regulatory changes 2025–2030. Launch micro-modules from your first audit deltas, following CE patterns in this CE impact guide.
Days 61–90 — Prove It.
Pick three high-ROI themes (e.g., E/M leveling, HCC evidence, hot modifiers). Show error reduction ≥30% after training (see CE acceleration), denial overturn ≥40%, and refund compliance within 60 days. Document with a reproducible method referencing predictive analytics.
Months 3–6 — Industrialize and Expand Scope.
Stand up a versioned SOP library; publish a risk register with RAG ratings. Teach providers via service-line huddles and specialty tip-sheets (blend in modifier playbooks). Implement AI oversight using governance from future skills. Add remote audit SLAs referencing remote job systems.
Months 6–12 — OIG-Grade Readiness.
Publish a compliance annual report: sampling math, refund logs, education impact, appeals library, and policy change log (source method from CMS compliance guide). Add case studies on state payer quirks using California and Florida context (see California jobs and Florida outlook). Track automation exposure and pivot roles per future-proof careers.
3) Evidence-First Skill Building: How to Become Audit-Ready (Fast)
Hiring panels don’t want theory—they want artifacts. Start with two miniature audits that mirror OIG priorities: (1) E/M services where leveling and time documentation conflict; (2) modifier-heavy procedures with frequent CARC hits. Use risk-based sampling math, then report accuracy, medical necessity, overturn opportunity, and refund exposure. Cite policies precisely and include a change log. Lean on AMBCI’s policy and analytics stack—compliance trends, predictive analytics, and AI oversight from future skills—to frame your method in interviews.
What separates top candidates
Explainability: You can justify every sample, threshold, and appeal clause with specific CMS citations (foundation: CMS compliance guide).
Measurability: You track precision/recall for edits and AI/CAC, then connect to denial reduction (concepts from AI in RCM).
Education impact: Your audits convert into micro-modules with error deltas (playbook: CE acceleration).
Quick Poll: What’s your #1 blocker to becoming an OIG Healthcare Compliance Auditor?
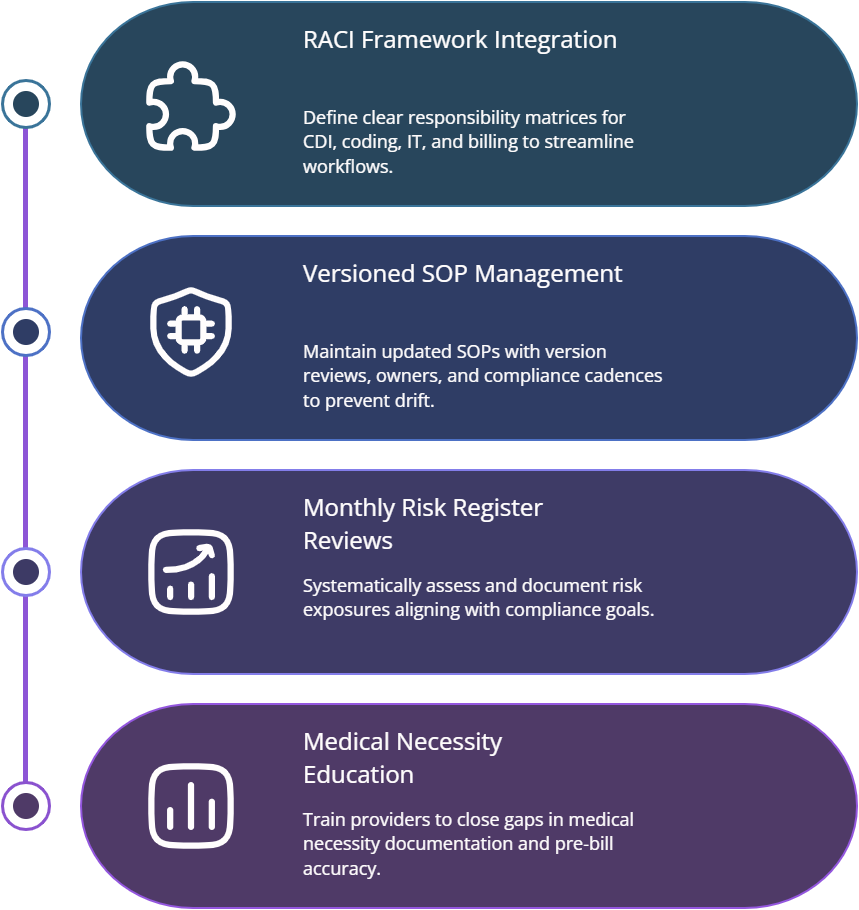
4) People, Governance, and the Art of Staying Sanction-Proof
Compliance collapses when roles, SOPs, and evidence trails are vague. Build a governance spine: RACI across CDI, Coding, PFS, and IT; a versioned SOP library with owners and review cadences; and a risk register reviewed monthly. Use provider education to seal medical necessity gaps and prebill edit councils to reduce false positives. Fold in modifier bootcamps sourced from modifier mastery and set remote SLAs leveraging remote-work guides. Maintain refund logs to meet federal 60-day expectations and document AI oversight in line with AI-skills guidance.
Audit-ready artifacts you’ll publish quarterly
Compliance report summarizing sampling math, error drivers, refunds, appeals, and training impact, grounded in CMS compliance.
Policy drift memo tracking payer updates and mitigation plans—use regulatory changes 2025–2030.
Automation risk brief showing the precision/recall of CAC and edits, citing methods from predictive analytics.
5) Breaking Into the Role: Credentials, Interviews, and Promotions
You don’t need a dozen letters—what you need is defensible work and clear ROI. Align your certification and study plan with career ladders in CPC roadmaps, then add compliance weight by mastering policy + appeal writing with compliance trends and modifier rigor via modifier application. For interviews, bring two case studies with method, citations, metrics, and education results; show how you’ll operationalize AI oversight using AI in RCM. After you land the role, target a 12-month promotion case built on a compliance dashboard, overturned denials, and clean ICD update go-lives supported by ICD-11 guidance.
6) FAQs — OIG Healthcare Compliance Auditor (High-Value Answers)
-
Two short, real audits with reproducible sampling math, policy citations, and before/after error deltas. Include a false-positive analysis on prebill edits and a refund log. Anchor your method with CMS compliance and show analytics sophistication via predictive trends.
-
Use a value-driver tree: defect → denial avoided (CARC) → cash retained → risk avoided. Quantify overturn rates and refund timeliness; cite regulation sources. Provide training impact with post-ed error ↓ ≥30% using approaches in CE acceleration.
-
Require explainable rules, precision/recall tracking, and manual review thresholds by risk class. Document decisions in an automation governance memo mapped to AI in RCM and close the loop with post-education deltas from future skills.
-
Start with CARC 50 (medical necessity), CARC 97 (invalid coding), CO-B7/B8 (bundling), and CO-16 (missing info). Map them to specialty hot spots, then build payer-specific appeals using the frameworks in regulatory changes and modifier accuracy in this piece.
-
Run a monthly policy council: each owner monitors specific payers, updates the versioned SOP, and logs effective dates. Summarize deltas in a two-page brief. Use AMBCI’s trend trackers—compliance trends and how new regulations impact careers.
-
Pair your primary coding credential with deep compliance practice: policy citation drills, appeal writing, and sampling math. Build from CPC laddering, add ICD update fluency via ICD-11 guidance, and sharpen analytics using predictive analytics.
-
Maintain a 60-day refund tracker with dates, sources, amounts, and corrective actions. Tie every refund to a root cause and an updated SOP. Cite policy authority in your log and include it in your quarterly compliance report aligned to CMS compliance best practices.