Future Innovations in Medical Billing Software & Financial Management
The financial backbone of healthcare is transforming faster than ever. By 2030, medical billing software will no longer be just a tool — it will be an intelligent financial ecosystem powered by automation, predictive analytics, and blockchain-backed transparency. These innovations are redefining how practices manage claims, revenue cycles, and patient payments. This article explores how technology will reshape medical billing, compliance, and cash flow management, helping coders and billing specialists stay ahead in a fully digitized healthcare economy.
1. The New Architecture of Medical Billing Systems
The next generation of billing platforms is being rebuilt for end-to-end automation. Instead of fragmented software for claim entry, coding, and reconciliation, future systems will operate as AI-integrated revenue networks that predict errors, guide audits, and optimize reimbursements in real time.
As explored in AI in Revenue Cycle Management: Upcoming Trends for Medical Coders, automation now enables instant detection of inaccurate CPT or ICD codes — slashing denial rates by over 40%. By 2030, algorithms will even recommend payer-specific optimization paths before claims submission.
Integration with cloud APIs and digital ledgers will ensure audit-proof accuracy. Tools referenced in How Automation Will Transform Medical Billing Roles by 2025 highlight how hospitals are already adopting API-first billing infrastructures that connect seamlessly with EHR and insurance systems.
These next-gen ecosystems will also embed real-time compliance layers, like those discussed in Understanding HIPAA Compliance in Medical Billing, ensuring all transactions meet U.S. and international health data regulations.
2. Financial Automation and Predictive Intelligence
The next major leap for billing systems lies in predictive financial intelligence. Machine learning algorithms will continuously analyze claim success rates, AR aging, and reimbursement cycles to forecast revenue health weeks in advance.
According to Predictive Analytics in Medical Billing: Key Trends and Opportunities, predictive RCM models already reduce claim lag times by 30%. By 2030, these models will become autonomous advisors, adjusting staff priorities and alerting billing teams about payer-specific risks.
Automation tools mentioned in Mastering Revenue Cycle Management: Complete Guide show how smart reconciliation algorithms will flag missing payments instantly, closing the loop between coding accuracy and financial control.
Additionally, AI-based contract management systems will verify whether payers are meeting negotiated reimbursement terms, protecting organizations from silent revenue leaks.
3. Integration of Payment Portals and Patient Engagement
The patient experience is becoming a financial journey of its own. As outlined in Future Skills Medical Coders Need in the Age of AI, healthcare organizations are now judged not only by their clinical quality but also by how easily patients can understand and settle bills.
Modern billing systems integrate self-service payment portals, real-time cost estimators, and AI-driven payment reminders, leading to faster reimbursements and higher patient trust.
Integrations like these, discussed in Guide to Selecting Medical Billing Software Solutions, show that software is evolving toward end-user empathy, where transparency and financial literacy are core user experience metrics.
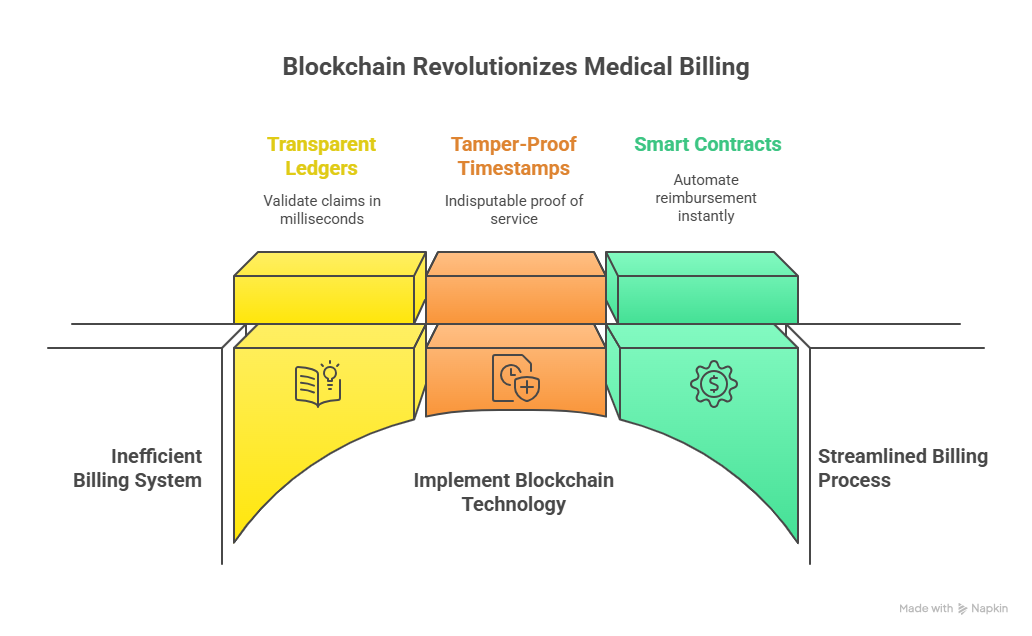
4. Blockchain and Decentralized Trust in Medical Billing
Blockchain will be the trust engine of healthcare finance. With transparent ledgers, billing systems can validate claims in milliseconds — no middlemen, no manual reconciliation. Each transaction will carry a tamper-proof timestamp, creating indisputable proof of service.
As analyzed in Upcoming Regulatory Changes Affecting Medical Billing 2025–2030, regulators are moving toward decentralized reporting systems that require immutable audit trails. Blockchain billing will satisfy these demands automatically.
Smart contracts will ensure payers release funds instantly when conditions are met — automating reimbursement without human intervention. The result: fewer denials, zero manual reconciliation, and faster patient refunds.
5. The Road Ahead: AI Collaboration, Compliance, and Workforce Upskilling
By 2030, billing professionals will operate in AI-supervised environments where automation executes transactions, but humans provide oversight, ethics, and optimization.
This evolution aligns with Comprehensive Guide to Denials Prevention and Management, which emphasizes how coders must master tools that combine financial reasoning with compliance monitoring.
Continuous upskilling will focus on AI literacy, fintech awareness, and interoperability management, preparing professionals for hybrid roles that merge finance, compliance, and predictive modeling.
6. FAQs: Future Innovations in Medical Billing Software
-
AI will automate coding, claim validation, and forecasting — transforming billing teams into financial analysts.
-
Blockchain enables tamper-proof claim records and automated smart contract payments between providers and payers.
-
Yes — professionals will oversee automation, manage exceptions, and ensure ethical data compliance.
-
By upgrading to systems with predictive dashboards and automation modules outlined in Guide to Selecting Medical Billing Software Solutions.
-
Data interpretation, RPA management, and financial modeling will define top-tier billing specialists.
-
They’ll gain access to transparent, affordable, and real-time financial engagement tools.
-
Specialized AI, RPA, and financial data analytics certifications from AMBCI and similar institutions.