Predicting Changes in Healthcare Reimbursement Models by 2027
By 2027, healthcare reimbursement won’t look anything like today’s fee-for-service system. The rise of value-based care, AI-enabled audits, and real-time claim adjudication is forcing coders, billers, and providers to adapt faster than ever. Payment models are shifting toward outcomes, interoperability, and automation, demanding new skill sets from every revenue professional. This article dives deep into upcoming reimbursement transformations, blending insights from AMBCI’s research and training frameworks to help coders anticipate payer behaviors, reduce denials, and master predictive billing workflows—turning uncertainty into opportunity across both private and public reimbursement landscapes.
1) From Volume to Value: The Inevitable Reimbursement Shift
The traditional fee-for-service system rewarded quantity—every lab, visit, or test meant more revenue. But the next era, outlined in Comprehensive Guide to MACRA & Quality Payment Programs, is about value-based reimbursement (VBR). By 2027, providers will be paid for outcomes, efficiency, and documentation integrity, not just volume.
Coders will serve as quality assurance analysts, ensuring accurate risk adjustments and clinical measure reporting. Leveraging frameworks from Ethical Practices in Medical Billing and Comprehensive Guide to Clinical Documentation Integrity (CDI), they’ll become key contributors to provider scorecards that determine future reimbursements.
For those trained through AMBCI’s Medical Billing & Coding Certification, compliance and accuracy will directly translate into revenue preservation.
2) The Data Economy: How Predictive Analytics Is Rewriting Payer Behavior
By 2027, reimbursement will be data-driven at every layer. Coders who understand predictive analytics from Predictive Analytics in Medical Billing: Key Trends & Opportunities will see patterns in denials before they occur. AI tools can now analyze historical claims to predict which submissions are at risk, saving organizations millions.
As detailed in AI in Revenue Cycle Management: Upcoming Trends for Medical Coders, AI-enhanced RCM solutions will dominate the reimbursement process—training models on millions of claim outcomes. Coders equipped with these tools not only increase clean claim rates but gain negotiation leverage with payers through accurate data-driven insights.
3) MACRA, MIPS, and the Expanding Web of Accountability
The Medicare Access and CHIP Reauthorization Act (MACRA) continues to evolve through 2027, expanding metrics under the Merit-Based Incentive Payment System (MIPS). Providers and coders who fail to align with these programs risk payment reductions up to 9%. Using AMBCI’s Comprehensive Guide to MACRA & Quality Payment Programs ensures coders can interpret scoring criteria correctly and integrate it into their claims.
Complementing this with data validation strategies from Comprehensive Guide to Denials Prevention and Management and ethics reinforcement from Ethical Practices in Medical Billing strengthens both coding credibility and reimbursement predictability.
MACRA-linked reimbursement requires cross-functional literacy—combining coding knowledge, compliance awareness, and data analytics—to ensure sustainability under evolving payment conditions.
Quick Poll: What’s Your Biggest Reimbursement Concern?
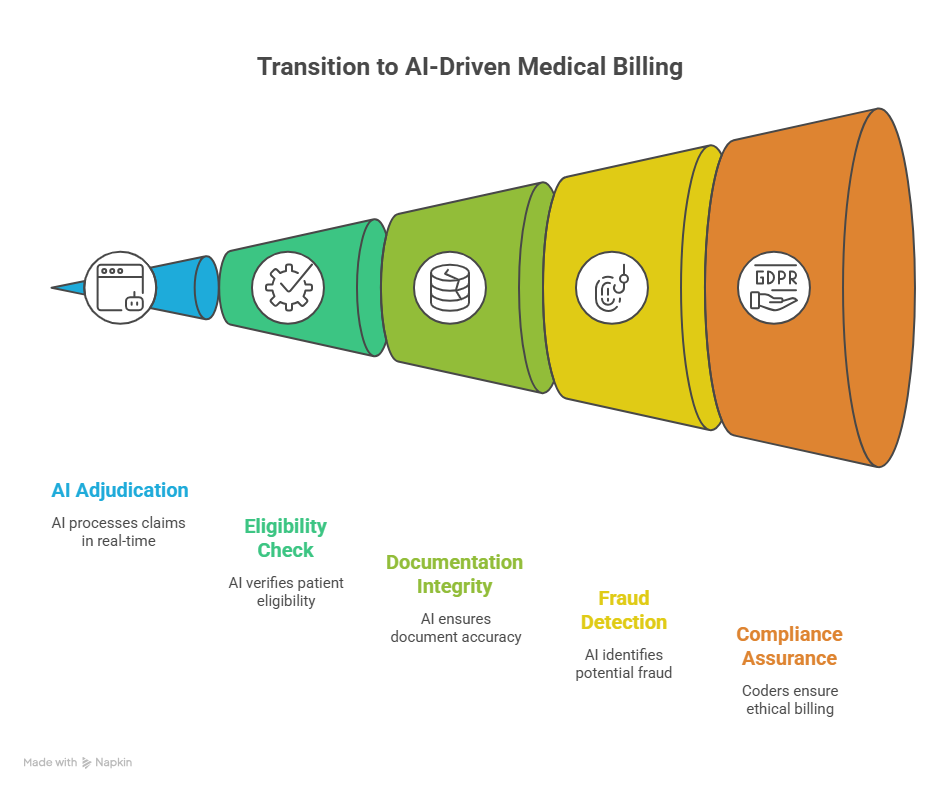
4) AI-Driven Adjudication and Automated Payer Relations
Automation is erasing the traditional lag between claim submission and adjudication. By 2027, AI-powered payers will process and approve claims in minutes. As explained in How Automation Will Transform Medical Billing Roles by 2025, automated adjudication models can scan data for eligibility, documentation integrity, and fraud patterns in real-time.
Coders must understand algorithmic transparency, building on Ethical Practices in Medical Billing to ensure AI models adhere to fair billing logic. Using Understanding Insurance Claim Adjustment Reason Codes (CARCs) enables faster correction and resubmission cycles. Coders fluent in automation will move from being claim processors to AI verifiers and payer liaisons, ensuring fairness and compliance coexist with speed.
5) Preparing for a Post-2027 Reimbursement Ecosystem
The next frontier of reimbursement will demand interdisciplinary expertise—combining billing, analytics, policy, and ethics. AMBCI-certified professionals who regularly engage with resources like Future of Remote Medical Billing & Coding Jobs and Understanding HIPAA Compliance in Medical Billing will stay ahead of compliance thresholds.
Coders should also integrate insights from Comprehensive Guide to Medical Coding in Complex Trauma Cases and Advanced Billing & Coding for Interventional Radiology to tackle specialized reimbursement workflows. The future favors coders who think like economists, using predictive data to influence how payers define “value.” Those with data storytelling and compliance auditing expertise will dominate leadership positions across the RCM ecosystem.
6) FAQs: Understanding the Future of Reimbursement Models
-
The universal adoption of value-based care, emphasizing outcomes over quantity. Refer to MACRA & Quality Payment Programs and Ethical Practices in Medical Billing for adaptation strategies.
-
By studying AI in RCM and Automation in Medical Billing, coders can learn how to supervise automated decisions ethically and effectively.
-
Yes—insurers increasingly expect analytics-informed submissions. Courses like Predictive Analytics in Medical Billing prepare coders to anticipate denials before they occur.
-
Remote coders will manage global payers through interoperable tools, referencing Future of Remote Medical Billing for role evolution.
-
The AMBCI Medical Billing & Coding Certification, reinforced by compliance and data analytics micro-certifications.
-
It will phase out gradually. Providers focusing on outcome metrics and bundled payments will outperform traditional models.
-
Ethical oversight, as covered in Ethical Practices in Medical Billing, ensures fairness in algorithmic decisions, protecting both coders and patients.
-
Yes—legislative models are stabilizing parity payments for telehealth, ensuring consistent revenue as outlined in Comprehensive Guide for Telemedicine Services.