Guide to CPC (Certified Professional Coder) Exam Terms
The Certified Professional Coder (CPC) exam is the most recognized credentialing test for medical coders in the United States. Offered by the AAPC, this exam measures your ability to interpret physician documentation, apply CPT®, ICD-10-CM, and HCPCS Level II codes accurately, and understand reimbursement systems. Passing the CPC exam isn't just about memorizing procedures—it requires fluency in CPC exam terminology, including clinical language, modifier logic, and code structure. Whether you're a medical billing specialist, coding student, or transitioning healthcare professional, mastering this terminology is what separates passing scores from costly retakes.
Why does terminology matter so much? Because every CPC question is a layered puzzle built on precise language. Misinterpreting a single term—like “excision” vs. “resection” or “sequela” vs. “complication”—can derail an otherwise correct answer. Even seasoned coders stumble on traps embedded in exam-specific language. If you're preparing for CPC certification, knowing the exam domains, the structure of code books, and real-world use of key terms isn't optional—it's the foundation. This guide will decode the language of the exam, demystify commonly misunderstood terms, and show how those terms tie directly into coding success, job readiness, and audit-proof documentation.
Core CPC Exam Domains Explained
Understanding the CPC exam domains isn’t about memorizing topic names—it’s about knowing what each domain truly demands. The AAPC’s exam blueprint outlines what skills are tested, but many candidates underestimate the depth required in areas like medical terminology, coding guidelines, and proper code set application. Below, we’ll break down three core areas that consistently shape your performance on exam day.
Coding Guidelines and Conventions
Every code set—CPT, ICD-10-CM, and HCPCS—comes with strict rules that dictate how codes should be selected. These aren't just filler questions; roughly 70% of exam errors stem from overlooking these instructions. For example:
In CPT, guidelines before section headers (e.g., surgery) outline when certain codes are reportable together.
ICD-10-CM uses symbols like “Excludes1” and “Code first” that directly impact sequencing logic.
HCPCS guidelines determine when a supply or medication can be billed independently or as part of a procedure.
Misapplying a guideline, even with the correct code, can mean a failed question. You must treat guidelines as mandatory—not optional reading.
Medical Terminology and Anatomy
Every multiple-choice question assumes you can translate clinical documentation into codable procedures. That requires command over:
Prefixes and suffixes (e.g., -ectomy, -ostomy, endo-, peri-).
Anatomical structures (knowing duodenum vs. jejunum matters).
Disease types and classifications (e.g., acute, chronic, congenital).
Questions won’t always hand you the body part or system in simple terms—they’ll use phrases like “proximal phalanx of the second digit,” and expect you to identify both location and applicable code logic. Strong medical language fluency is non-negotiable for accurate interpretation.
HCPCS, CPT, and ICD Code Sets
Each code set tests a distinct skill:
CPT evaluates procedural accuracy, especially for surgical coding, radiology, and evaluation & management services.
ICD-10-CM assesses diagnostic precision based on symptomatology, etiology, and sequela logic.
HCPCS Level II covers durable medical equipment, drugs, and non-physician services—often overlooked but critical.
Expect integrated questions that ask you to apply CPT and ICD codes together in context of modifier usage or documentation necessity. You’ll also face real-world overlaps—like a patient receiving a DME item (HCPCS), with a procedure (CPT), and diagnosis (ICD-10). Recognizing how all three work together is vital for exam-day performance.
| Domain | Focus Area | Key Skills Tested |
|---|---|---|
| Coding Guidelines & Conventions | Code-specific rules from CPT, ICD-10-CM, and HCPCS | Understanding “Excludes1”, “Code First”, and CPT-specific bundling or reporting instructions |
| Medical Terminology & Anatomy | Clinical vocabulary and anatomical comprehension | Translating terms like “proximal phalanx” or “ostomy” into accurate code logic |
| HCPCS, CPT, and ICD Code Sets | Application of procedural, diagnostic, and supply-related coding | Combining CPT, ICD-10, and HCPCS codes with correct modifier usage in real-world documentation |
Breaking Down Coding Book Structures
Success on the CPC exam depends not just on knowing codes—but on navigating the physical books under pressure. Time is your enemy during the test, and mastering book structure is what gives top scorers their edge. You’re allowed to bring non-electronic, paper-based code books into the exam, and knowing exactly where to find what you need is half the battle.
CPT Manual Section Breakdown
The CPT book is the most heavily tested, making up over 60% of the CPC exam. It’s divided into major sections like:
Evaluation and Management (99202–99499)
Surgery (10021–69990) – the largest section, organized by body system
Radiology, Pathology & Laboratory, and Medicine
Each section has its own guidelines. These aren’t filler—they determine correct code usage. For example, the Surgery section has “Separate Procedure” notations that restrict billing when more extensive procedures are performed. Also, never skip the “Parenthetical Notes” under codes—they clarify modifier usage, bundling rules, and cross-references.
Navigating quickly within CPT means flagging sections, using highlighters sparingly, and understanding how codes flow from general to specific. Even the index isn’t always reliable—you need to confirm code accuracy within the full listing.
How to Navigate ICD-10-CM Chapters
The ICD-10-CM book is organized into 21 chapters based on body systems and condition types. For example:
Chapter 9: Diseases of the Circulatory System
Chapter 19: Injury, Poisoning & External Causes
Chapter 21: Factors Influencing Health Status (Z codes)
Each chapter starts with its own guidelines and includes Tabular Lists and Alphabetic Indexes. Don’t rely on the index alone. Always verify the code in the tabular list to check for Excludes1/2 notes, sequencing instructions, or required additional characters.
HCPCS Level II Reference Tips
The HCPCS manual often trips up test-takers because it appears small but is dense with detail. Key tips:
Familiarize yourself with code ranges A0000–V9999, especially for DME and supplies.
Understand per-unit billing logic. Some codes refer to per-dose, not per-service.
Learn which codes require documentation or prior authorization—this appears in code descriptions and is tested.
Speed, structure, and knowing how to cross-check references between books will cut your answering time by up to 30%, which is crucial across 150 questions.
Most Common CPC Exam Terms You Must Know
Memorizing lists of coding terms won’t cut it—understanding their contextual meaning will. The CPC exam is designed to test your ability to interpret terminology as it's used in real claims, audits, and physician documentation. Below are the top term categories you must know cold.
Medical Necessity vs. Medical Decision Making
These two concepts appear alike—but on the CPC exam, confusing them is a guaranteed point loss.
Medical Necessity is the justification for a service, rooted in the diagnosis. It's what payers want to see: that the procedure was essential for the patient's condition. If the diagnosis doesn’t align with the procedure code, even the “right” CPT code will fail medical necessity checks.
Medical Decision Making (MDM) refers to the provider’s cognitive work—how they assessed the patient’s risk, data complexity, and problem severity. It drives Evaluation & Management (E/M) levels and is heavily tested.
Example: A low-complexity diagnosis may support an E/M code level 3, but if the MDM shows high complexity—due to multiple management options or significant data review—a higher E/M level may be justified.
Modifiers and Their Clinical Impacts
The CPC exam tests modifier logic in dozens of ways. Modifiers clarify when, why, or how a service was delivered. Memorizing what each one means is only step one—you must also apply them in bundled, time-sensitive, and procedural overlap scenarios.
Modifier 25 indicates a separately identifiable E/M service on the same day as a procedure.
Modifier 59 distinguishes services that are not normally reported together.
Modifier 51 flags multiple procedures in a single session.
The exam often embeds these in narratives. You’ll see phrasing like “unrelated procedure on the same day” or “distinct procedural service” instead of the modifier itself. Read between the lines.
Incorrect modifier use leads to claim denials and compliance risks. Learn their impact not just on reimbursement—but on provider audits.
Place of Service, Units, and Bundling
These terms affect billing accuracy, reimbursement, and documentation audits.
Place of Service (POS) codes identify where the service occurred (e.g., 11 = office, 21 = inpatient).
Units define how many times a service was performed. For HCPCS, some drugs are coded per milligram, not per injection.
Bundling means combining services into one code. Know when procedures are inherently included in others—like post-op pain management bundled in anesthesia.
Questions may test your understanding of unbundling (which is a billing error) or services that seem separately billable but aren’t. Knowing when not to code something is as important as knowing when to.
| Term Category | Definition / Usage | Why It’s Tested |
|---|---|---|
| Medical Necessity vs. MDM |
Medical Necessity = Justifies the procedure based on diagnosis. MDM = Clinical reasoning complexity. |
Drives E/M level selection and determines claim approval. |
| Modifiers (25, 59, 51) | Clarify how/why services were performed. Embedded in case narratives—not listed directly. | Misuse causes denials and audit flags; critical for interpreting bundled vs. unbundled services. |
| Place of Service, Units, Bundling |
POS = Where service occurred Units = Frequency of service Bundling = What’s included in a single code |
Errors in these areas lead to incorrect reimbursement or compliance violations. |
Coding Scenarios: What the Terms Look Like in Practice
Knowing definitions is one thing. But in the CPC exam, you’re expected to apply terminology in real-world medical documentation. This section breaks down how terms show up in actual coding questions and how misreading just one can cost you the point.
Real-Life Modifier Use
Modifiers appear in nearly every clinical scenario on the CPC exam. You’re not given a list—you’re given a story. For example:
“A 65-year-old patient presents for lesion removal on the forearm and is also evaluated for hypertension management.”
Here’s what you must extract:
A procedure (lesion removal)
A distinct E/M service (hypertension)
Therefore: Modifier 25 applies to the E/M
Another case:
“Bilateral inguinal hernia repair performed using laparoscopic technique.”
Don’t just grab a bilateral code. Recognize that Modifier 50 may be appropriate only if both procedures are unilateral and need distinct reporting. The CPC tests your grasp of when modifiers are appropriate—and when they’re overused.
Sample Evaluation & Management Coding Breakdown
E/M services are a cornerstone of CPC testing. You’ll often see vague clinical notes like:
“Physician evaluated a new patient with three chronic conditions, reviewed labs, and ordered an MRI.”
Here’s how to break it down:
New patient = higher weight
Multiple stable problems = moderate complexity
Data reviewed = MRI and labs = 2+ elements
Result: Moderate MDM → 99204 or 99214 based on context
The challenge lies in decoding the wording. The terms won’t say “moderate MDM”—they’ll describe enough elements for you to assign the correct level.
Coding Pitfalls with Terminology
Some terms deliberately confuse test-takers. Examples:
“Simple repair” vs. “Layered closure” — the former refers to CPT 12001–12007, the latter requires intermediate repair codes.
“Subsequent visit” vs. “Established patient” — not interchangeable. “Subsequent” applies in inpatient care, not outpatient settings.
“With” vs. “Due to” — these two terms change code sequencing in ICD-10-CM.
CPC scenarios aren’t hard because of obscure knowledge—they’re hard because the terminology is precise. Misinterpreting one word changes everything.
| Modifier Use in Context | E/M Coding Breakdown | Terminology Pitfalls |
|---|---|---|
| Lesion removal + hypertension evaluation → Apply Modifier 25 to E/M | New patient, 3 chronic conditions, MRI + labs → Moderate MDM → 99204 or 99214 | “Simple repair” = CPT 12001–12007; “Layered closure” = intermediate repair codes |
| Bilateral hernia repair (laparoscopic) → Use Modifier 50 only if both are unilateral | MDM elements described indirectly; decode to assign E/M level correctly | “Subsequent visit” ≠ “Established patient” — different care settings |
| Modifiers are embedded in narratives; not listed—must be inferred contextually | Look for time-based and complexity cues in vague language | “With” vs. “Due to” → affects ICD-10-CM sequencing and code logic |
Decoding CPC Exam Question Language
The CPC exam doesn’t just test your coding skills—it tests how well you interpret the language of medical documentation and question construction. Every word is intentional. Knowing how to decode this phrasing separates high scorers from borderline failures. Let’s break down the three most important linguistic patterns in CPC questions.
Terminology in Case Studies
Case studies make up a major portion of CPC questions. These are typically 2–4 sentence clinical narratives, often packed with embedded terms that dictate the correct code choice.
For example:
“The patient was brought in for arthroscopic debridement of the right knee joint with extensive synovectomy.”
This isn’t just a knee procedure. It involves:
Endoscopic technique (arthroscopic)
Extent of the procedure (extensive vs. limited)
Anatomical site (right knee joint)
One wrong assumption about the word “extensive” vs. “limited” could lead to selecting a code with the wrong RVU—and thus failing the question. Read every term like a billable event.
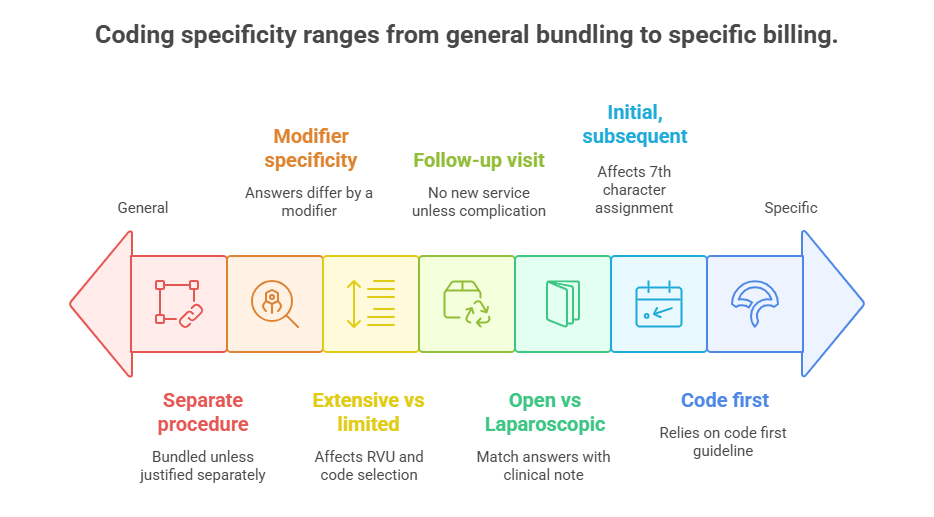
Keywords that Indicate Traps or Hints
CPC exam writers embed clues and traps into phrasing. Common signal terms include:
“Separate procedure” – alerts you that the procedure may be bundled unless justified separately
“Follow-up visit” – typically suggests no new service is billable unless a complication is addressed
“Initial encounter”, “subsequent encounter”, or “sequela” – crucial for ICD-10-CM seventh-character assignment
Ignore these terms, and you risk choosing a code that fails sequencing rules or doesn’t meet medical necessity logic.
Answer Choice Logic Based on Key Terms
Here’s the trick most coders miss: the answer choices themselves contain context. For example:
If all four answers differ by only one modifier, the scenario likely tests your knowledge of modifier specificity.
If codes vary by approach (e.g., open vs. laparoscopic), look for that exact term in the clinical note.
Don’t guess—dissect. Find the keyword that aligns directly with what differentiates one answer from the next. If you can’t, the question may be testing a “code first” or “includes” note, so revisit the hierarchy of coding logic.
How CPC Exam Terms Connect to Real-World Coding
CPC exam terminology isn’t academic—it’s practical. Every tested term reflects a real scenario faced daily by professional coders. Understanding how these terms transfer into actual job responsibilities is what makes Certified Professional Coders (CPCs) more hireable, audit-proof, and reimbursement-ready.
Employer Expectations
Employers don’t just want certified coders—they want coders who can communicate fluently in payer and provider language. This includes:
Identifying medical necessity in a provider’s note before submitting a claim.
Spotting incomplete documentation that fails to support a high-level E/M code.
Knowing which modifiers avoid denials and which trigger red flags.
You’re not just coding—you’re translating provider intent into billable, compliant data. Mastering exam terms means mastering the language of revenue cycle compliance.
Role in Claim Submission and Audits
Claims are often denied due to terminology misuse. For example:
Failing to connect diagnosis language to the procedure performed results in medical necessity denials.
Incorrect use of modifiers 25 or 59 can lead to accusations of unbundling or duplicate billing.
Mislabeling POS codes may misalign with payer rules.
When audits hit, coders who understand terminology don’t panic—they reference code guidelines, documentation standards, and payer policies confidently. CPC exam prep terms are the same ones used in appeals and RAC audits.
Use in Risk Adjustment and Reimbursement
In risk adjustment models (like HCC coding), even a small terminology error can cost thousands. Example:
Coding “history of diabetes” instead of “uncontrolled diabetes mellitus” affects risk scoring, which drives insurer reimbursement.
These models rely heavily on ICD-10-CM specificity and terms like “chronic,” “complication,” or “acute on chronic.” CPC-level knowledge of those distinctions is what qualifies coders for high-paying roles in payer organizations.
What AMBCI’s Medical Billing and Coding Course Teaches You About CPC Exam Language
If you're serious about mastering the terminology required for CPC exam success and excelling in a real medical coding job, AMBCI’s Medical Billing and Coding Certification delivers the edge you need. This isn’t a generic overview—it’s a deep-dive, 200+ module program designed to build term fluency, procedural accuracy, and payer-savvy billing logic from the ground up. Unlike outdated textbook prep, AMBCI uses active-learning tools, real-world case examples, and exam simulation drills to train coders in exactly the language and coding frameworks tested by the AAPC.
Whether you’re preparing for the CPC or CPB exam, or looking to increase your employability with clinical teams and revenue cycle managers, this certification closes the gap between book knowledge and on-the-job results.
Terms Covered in the Curriculum
The curriculum doesn’t just mention coding terms—it drills them through interactive examples, quizzes, and coding labs. You’ll develop real command over:
Evaluation & Management (E/M) terms like MDM, time-based coding, and problem complexity
ICD-10-CM classification phrases including laterality, manifestations, and encounter type logic
CPT terminology and procedural pairings, especially in surgical and anesthesia coding
Every module builds your ability to translate vague physician language into precise, billable code sets. This is terminology training built for high-stakes exam environments and payer audits alike.
Interactive Tools for Memorizing Terms
AMBCI integrates gamified flashcard decks, audio-spoken definitions, and clinical scenario builders to help students actively retain terminology. Instead of reading static lists, you engage with:
Matching games for modifiers and usage context
Drag-and-drop sequencing challenges for code hierarchy logic
Timed drills simulating CPC case-based questions
These tools help boost memory retention by over 40%, especially for coders with no clinical background.
Why Terminology Mastery Improves Exam Scores
The majority of CPC exam failures don’t come from code lookup errors—they come from terminology misinterpretation. AMBCI trains you to:
Instantly recognize which words trigger code exclusions or inclusions
Decode multi-layered clinical notes under time constraints
Choose between lookalike answer choices by identifying the one word that shifts context
If you want to go into your exam reading like an auditor and coding like a revenue expert, this is the program built to get you there.
Frequently Asked Questions
-
The most effective way to memorize CPC terminology is through active recall and context-based learning. Instead of passively reading lists, use flashcards, scenario drills, and mock coding cases that apply terms in real contexts. Prioritize confusing pairs like excision vs. resection or modifier 25 vs. 59. Repetition spaced over multiple sessions enhances long-term retention. Resources like AMBCI’s interactive tools also offer gamified flashcards and drag-and-drop terminology maps. These methods improve recall speed, which is crucial during the exam’s time crunch. Always follow up each term with its usage example and test your understanding using real clinical documentation samples.
-
There is no official list, but you should expect to master over 150 core terms across CPT, ICD-10-CM, and HCPCS Level II. This includes procedural terms like biopsy, debridement, or laparoscopic, diagnostic terms like acute, chronic, sequela, and administrative terms like POS codes, bundling, and modifiers. Beyond memorization, you need to know how they function within documentation and coding logic. Every exam question is built around these terms in context, not isolation. It’s not about quantity—it’s about understanding how they influence code selection, sequencing, and compliance.
-
Yes—and that’s exactly why they matter. CPC exam terms reflect real payer, provider, and documentation language. You’ll encounter the same phrasing in denial letters, claim forms, and provider notes. For example, if you don’t understand what “subsequent encounter for fracture care” means in ICD-10, you could incorrectly bill for a primary encounter. Or misreading “separate procedure” in CPT could cause you to wrongly unbundle services. The terminology tested isn’t academic—it’s the daily language of claims, audits, and reimbursement logic. That’s why mastering it benefits you far beyond the exam.
-
The most commonly tested terms fall into a few categories:
Modifiers (especially 25, 59, 51, and 26)
Medical necessity, MDM, and bundling
Procedure-specific terms like excision, simple repair, closed treatment
ICD-10 encounter descriptors like initial, subsequent, and sequela
Documentation phrases such as evaluation of, history of, or status post
Expect the exam to present these in disguised clinical notes, not as direct questions. Recognizing them in context is what leads to correct code selection. Learning their definitions, clinical implications, and coding logic is critical to scoring high.
-
No, you can’t bring a terminology list or separate notes into the CPC exam. Only official paper-based CPT, ICD-10-CM, and HCPCS Level II code books are allowed, and they must follow AAPC’s guidelines. You can highlight and tab these books, but you cannot add written definitions or sticky notes with terminologies. That’s why internalizing the terms before exam day is so important. Make use of legally allowed notes like underlining key phrases in the books’ guidelines sections. But when it comes to real understanding, preparation—not cheat sheets—will get you through.
-
CPC questions often embed terminology in ways that test your understanding of nuance. For example:
A question may describe a “repeat procedure on the same lesion” without mentioning “Modifier 76,” expecting you to deduce it.
Terms like “with” or “due to” in ICD-10 scenarios alter sequencing and diagnosis linkage.
Words like “limited,” “layered,” or “simple” change the meaning in procedure hierarchy.
These subtle shifts are intentional traps. Success lies in recognizing how a word’s presence—or absence—impacts coding. You must dissect clinical phrasing and connect each term to its coding rule, inclusion, or exclusion logic.
-
Yes, AMBCI’s Medical Billing and Coding Certification is structured to build command over CPC-related terminology. The program includes over 200 modules where terms are integrated into real-world clinical cases, flashcard decks, and interactive scenario builders. Instead of just listing terms, AMBCI teaches you to apply them in:
Modifier-based decision trees
E/M level assignments
ICD-10-CM encounter logic
Code bundling examples
This layered training ensures you’re not just memorizing—you’re thinking like a certified coder. It’s built to meet CPC, CPB, and employer standards alike, making you fluent in the vocabulary of both testing and billing success.
Final Thoughts
Mastering CPC exam terminology is not optional—it’s the foundation of passing the exam and thriving in the field. Every question, every code, every modifier hinges on how well you interpret the language of medicine, billing, and reimbursement. This isn’t just about memorization—it’s about decoding intent, reading between the lines, and translating complex documentation into precise, compliant codes.
If you're preparing for AMBCI’s Medical Billing and Coding Certification, you’re already aligned with a curriculum built to make this language second nature. From modifiers and E/M levels to ICD-10 sequencing and payer logic, terminology isn’t just a topic—it’s the lens through which the entire exam is delivered.
Know the terms. Understand the rules. Apply them under pressure. That’s how coders pass—and professionals get hired.
Poll: What’s the most challenging part of CPC exam terminology for you?