Medical Billing and Coding Certification in New Jersey: Complete Guide for 2025–2026
New Jersey’s providers—from Hackensack Meridian and RWJBarnabas to independent multi-specialty groups—are scaling revenue-cycle operations and hiring certified talent that can keep denials down and cash flow predictable. With growing payer audits, compliance updates, and telehealth expansions, the demand for certified medical billers and coders has never been higher across New Jersey’s healthcare network. If you want a remote-friendly career with measurable growth, an AMBCI-aligned medical billing and coding certification is the fastest, most practical route. This state guide distills exactly what employers in NJ screen for, how long certification really takes, and how to position yourself against regional markets like Pennsylvania, Rhode Island, Massachusetts, and Connecticut—so you can negotiate confidently and land interviews faster.
1) New Jersey’s Hiring Climate & Why Certification Matters
New Jersey is a payer-dense state: commercial PPOs, Medicare Advantage plans, and NJ FamilyCare (Medicaid) all apply strict edit logic. Employers increasingly shortlist candidates who can prove ≥96% first-pass claims, accurate ICD-10-CM and CPT® coding, and sub-40-day A/R. AMBCI’s case-based curriculum maps tightly to those expectations, which is why recruiters prefer résumés that cite AMBCI plus evidence such as “reduced CO-97 bundling denials by 18% within 60 days.” If you’re benchmarking the Garden State, compare salary ladders with Pennsylvania’s hospital systems, clean-claim targets in Rhode Island’s payer hubs, externship models in Massachusetts, and weekend pathways in Connecticut. You’ll see one consistent theme: certified candidates move to interviews faster and negotiate stronger starting pay.
Employers in North Jersey (Bergen, Essex, Passaic) lean hospital and multi-specialty; Central/South Jersey (Middlesex, Monmouth, Camden) adds ambulatory surgery centers, cardiology, ortho, behavioral health, and primary care networks. That mix explains demand for coders who can switch contexts—E/M leveling for primary care, procedure coding for ortho, and telehealth modifiers (95/GT) with policy-specific documentation for behavioral health. For additional regional signals, compare coastal hiring in South Carolina, compliance emphasis in Maryland, and payer transparency trends in Virginia to sharpen your interview script.
New Jersey Medical Billing & Coding — 2025–2026 Salary, Skills & Job Outlook
2) Fastest Path to Certification (Prereqs, Timeline, Curriculum)
Prereqs: High school diploma/GED and basic computer literacy. Strong vocabulary in human anatomy and clinical terminology helps you accelerate through ICD-10 chapters. Learners who preview AMBCI’s glossary finish faster and retain more.
Timeline: Most NJ candidates complete an AMBCI-aligned program in 4–6 months. The fastest cohorts schedule weekly coding labs and two full mock exams. If you need a weekend or hybrid structure, benchmark Connecticut’s flexible intensives, Massachusetts’s commuter tracks, Rhode Island’s hospital partnerships, and Pennsylvania’s externship pipelines to choose a cadence that fits your work week.
Curriculum anchors:
Medical Terminology & Anatomy (documentation language that supports medical necessity)
ICD-10-CM foundations, CPT®/HCPCS coding, and modifier mastery (-25, -59, telehealth 95/GT)
Claim lifecycle: charge entry → edits → submission → posting → A/R triage → appeals
HIPAA, audit defense, and payer policy interpretation (NJ FamilyCare + MA plans)
If you plan to relocate or work fully remote, keep an eye on policy nuances in Maryland, Virginia, Maine, and Vermont—your interviewers will appreciate that multi-state fluency.
3) Salary Ladders, Remote Hiring & Where New Jersey Leads
Starting pay for certified entry-level roles typically lands between $38K–$42K, with rapid lift to the $52K–$58K band once you demonstrate KPI movement—clean-claim percentage, denial turnaround, and days in A/R. Specialists managing cardiology, orthopedics, behavioral health, and ASC coding frequently cross $70K+ as they master NCCI edits and documentation nudges that survive audits. To contextualize your ask, compare salary bands with Pennsylvania’s academic systems, remote first roles in Wisconsin, payer-centric opportunities in Maryland, and compliance-heavy openings in Massachusetts.
Remote hiring is robust in NJ due to proximity to New York–Philadelphia revenue hubs. Large systems and national RCM vendors hire home-based staff, especially those who cite Epic + eClinicalWorks/Kareo proficiency. If you’re optimizing for remote, study telehealth billing norms in Washington, cross-state remotes in West Virginia, and compact timelines in Utah to see how candidates frame their portfolios.
Quick Poll: What’s Your Biggest Challenge in Medical Billing?
4) What NJ Employers Test (and How to Prove You’re Ready)
Core measurements:
Clean-claim rate (target ≥96%) and denial rate by code family (E/M, procedural, telehealth)
Edit capture before submission; understanding of NCCI bundling and payer-specific LCD/NCD references
Days in A/R (≤40) and appeal success rate with payer-specific language
Software fluency: Epic + one ambulatory system (eCW, Kareo, Athena)
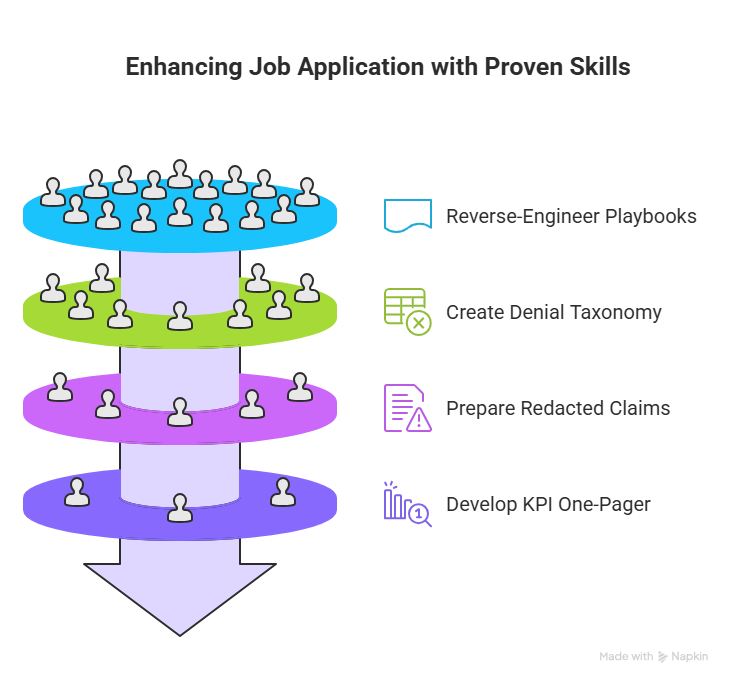
Proof on résumé: Quantify: “Maintained 97% first-pass rate across 1,100+ monthly claims,” “Cut CO-97 by 22% with modifier education,” “Lowered A/R from 52 to 36 days.” For sample phrasing, reverse-engineer state playbooks in Maryland, appeal frameworks in Massachusetts, externship wins in Pennsylvania, and telemetry coding tactics in Washington; use their patterns, then map to NJ payer rules.
Interview signals hiring managers love: A denial taxonomy table (CO-16/CO-97/PR-204 with “fix-paths”), a redacted claim set (one E/M, one surgical, one telehealth), and a KPI one-pager showing your baseline → improvement trend. To see how candidates frame these artifacts, review outcomes shared across Wisconsin’s remote network and CMS-aligned accuracy standards described for Rhode Island.
5) AMBCI Exam Strategy, 6-Week Plan & Portfolio Build
Why AMBCI? The exam mirrors live NJ workflows—payer pre-auth chains, documentation triggers for medical necessity, and bundling checks that general exam preps often ignore. Grads report onboarding faster because the exam feels like day-one work.
Six-week plan (battle-tested):
Weeks 1–2: ICD-10-CM by chapter (focus on musculoskeletal, cardiology, behavioral health). Cross-study Massachusetts and Maryland payer idiosyncrasies to train policy reading.
Week 3: CPT®/HCPCS—E/M leveling (99202–99215), modifiers (-25/-59/95/GT), and ASC packs. Compare documentation tips pulled from Connecticut and Rhode Island.
Week 4: Denial analytics & appeals; compose two payer-specific letters (commercial + MA plan).
Week 5: Two timed AMBCI mock exams; create an error log and retest.
Week 6: Portfolio: redacted claims, denial tracker, KPI one-pager. Align your framing with wins highlighted for Pennsylvania and remote-first narratives in Wisconsin.
Job-search accelerators:
Submit a tailored KPI one-pager with every application.
State your software stack (Epic + eCW/Kareo) in the first two lines of your summary.
Attach a short “denial playbook” PDF; managers love seeing fix-paths.
6) FAQs — New Jersey Medical Billing & Coding Certification (2025–2026)
-
Most learners finish in 4–6 months with an AMBCI-aligned schedule that pairs weekly labs and two timed mocks. If you’re juggling work, mirror the pacing used in Connecticut and Rhode Island weekend cohorts.
-
All appear in job posts, but AMBCI stands out for its scenario-driven assessments that simulate payer edits, ASC bundling, and telehealth documentation—skills echoed in guides for Massachusetts and Maryland.
-
Certified entry-level hires typically land $38K–$42K; rapid movement to $52K–$58K follows when you show KPI improvements. For negotiations, compare metro pay bands with Pennsylvania and coastal expectations in Rhode Island.
-
Yes—New Jersey benefits from tri-state hospital networks and national RCM firms that hire home-based talent. Candidates fluent in Epic + eCW/Kareo and trained on telehealth modifiers (95/GT) stand out—trends mirrored in Washington’s remote hubs and West Virginia’s distributed teams.
-
Expect CO-16 (info missing), CO-97 (bundled), PR-204 (non-covered), and CO-50 (not medically necessary). Use checklists: chief complaint tie-backs, time-based E/M rules, modifier validation, and documentation addenda. For practical denial playbooks, analyze tactics shared in South Carolina and Maryland.
-
Include three redacted claims (E/M, surgical, telehealth), a one-page denial taxonomy with fix-paths, and a KPI snapshot (clean-claim %, A/R days, appeal success). Borrow portfolio ideas from Pennsylvania’s 2025 cohort and remote-first framing in Wisconsin.
-
Absolutely. Candidates from finance/admin excel by leaning on metrics and SOPs. Start with AMBCI’s structured glossary + two weekly practice blocks. If you need momentum models, review compact timelines from Utah and accelerated externships in Massachusetts.
-