How Much Are Medical Billing and Coding Classes? Full Cost Breakdown
This guide breaks down the real cost of medical billing and coding classes in 2025, across every training format and certification level. Whether you’re planning for CPC, CPB, or both, you’ll know exactly what you should be paying—and what to avoid.
Average Cost Across the US
The cost of medical billing and coding classes in the U.S. ranges from $399 to over $5,000, depending on course format, credentialing goals, and delivery model. But the numbers alone don’t tell the full story. What really matters is what each price tier includes—or leaves out. Without knowing that, many students choose programs that seem cheap but end up costing far more due to missing essentials like exam prep, software training, or job support.
Low-End, Mid-Tier, and Premium Programs
1. Low-End Courses ($399–$899)
Low-end programs are usually 100% self-paced, non-interactive, and stripped down to videos and PDFs. They're often advertised through third-party marketplaces with no dedicated medical coding focus. These programs rarely include:
Exam registration or voucher fees
Mentorship or grading
EHR simulation or real billing exercises
They often skip specialty coding and don’t follow the AAPC CPC or CPB exam blueprints closely. Students in this tier often fail on the first try or spend extra buying mock exams, software tools, or live coaching afterward. Total cost with add-ons? Usually $1,200–$1,500 once everything is purchased a la carte.
2. Mid-Tier Programs ($1,000–$2,500)
Most serious learners land here. Mid-tier courses are often offered by coding schools, online medical academies, and some community colleges. They typically include:
Full access to CPC or CPB-aligned content
Graded practice exams
Instructor access (email or Zoom)
Some specialty module coverage (e.g., OB/GYN, psych, ortho)
Many also bundle one exam voucher, which alone costs $399–$499 through AAPC. With a mid-tier course, you're less likely to face hidden costs—and far more likely to pass on your first attempt. These programs are ideal for learners who want a complete certification roadmap without overpaying.
3. Premium Programs ($2,800–$5,500+)
At this range, you’re paying for live training or institutional branding. These include:
Bootcamps or synchronous classes (online or hybrid)
University-backed programs or private schools
Instructors delivering real-time teaching via Zoom or in person
Timed, proctored exams and cohort tracking
You’ll often get two or more certifications bundled (usually CPC and CPB), exam scheduling support, and career services—but the price is high because you're paying for overhead.
Still, many premium courses don’t include lifetime access, software simulation, or job performance feedback—and they often expire after 6 or 12 months. If you miss your exam window, you may need to pay to re-enroll.
Geographic Variation and Format Differences
In-person programs offered at trade schools or community colleges vary by state. A college-based CPC prep course in California may cost $3,000+, while a similar program in Texas might run $1,800 for residents. These usually require textbook fees, travel, and set schedules, which increase hidden costs.
In contrast, online-only programs like AMBCI offer national pricing with flat rates regardless of location—making them more affordable for learners in high-cost metro areas.
| Program Tier | Average Cost Range | What’s Included | Common Drawbacks |
|---|---|---|---|
| Low-End Courses | $399–$899 |
- Self-paced video/PDF content - Basic concepts only - No live instruction - No exam voucher |
- No EHR/billing software practice - No grading or feedback - Not exam-aligned - Hidden costs add $800+ post-purchase |
| Mid-Tier Programs | $1,000–$2,500 |
- CPC/CPB-aligned content - Mock exams + instructor access - Some specialty modules - Usually includes 1 exam voucher |
- Limited live teaching - May lack EHR simulation - May expire within 12 months |
| Premium Programs | $2,800–$5,500+ |
- Live classes / hybrid options - University or bootcamp format - Multi-cert bundles (e.g. CPC + CPB) - Career support + timed testing |
- Expensive with strict expiration - Often no lifetime access - May still lack software/practice feedback |
| In-Person College Programs | $1,800–$3,200 (state-dependent) |
- Semester format - Instructor-led on-campus - Textbook-based learning |
- Requires travel - Fixed schedules - Additional textbook & exam fees |
| Online National Programs (e.g. AMBCI) |
$1,200–$2,500 (flat-rate) |
- Consistent pricing - Dual-certification options - Live mentoring + lifetime access |
- None if program includes job support + exam prep - Best for self-disciplined learners |
What Affects Pricing?
If you’re wondering why one medical billing and coding course costs $499 while another charges $2,499, the difference comes down to what’s built into the training—and what’s missing. Four major factors affect the pricing of certification programs: the number of instructional hours, level of mentorship, inclusion of exam-related fees, and the tech platform delivering the course.
Hours, Mentorship, Exam Fees, Platform Used
1. Total Course Hours
The length and depth of the curriculum significantly impact the cost. A 20-hour course that only explains code categories costs less than a 150-hour course that simulates full billing workflows, EHR usage, and payer-side audits. Real career-prep programs are longer for a reason—they match what employers expect.
Courses aligned with AAPC’s CPC or CPB exams typically range from 80 to 180 hours, depending on whether they include practice cases, specialty modules, or advanced claim correction logic. The more time and structure involved, the more you can expect to pay—but the better your job outcomes.
2. Instructor Access and Mentorship
Courses that include live Q&A, instructor-reviewed assignments, or 1-on-1 support cost more—but they’re also what help you pass on your first attempt. If a program offers chat-only support or delayed email replies, you’re essentially on your own. That saves money, but it often leads to confusion, errors, and exam retakes.
Courses like AMBCI’s CPC + CPB program include mentorship, graded charting, and live feedback, which drives success on both the test and the job market.
3. Exam Inclusion and Certification Prep
If your course doesn’t include the CPC or CPB exam voucher, expect to pay an extra $399–$499 per exam. Many low-cost courses skip this entirely, meaning you're not only underprepared—you’re also hit with a big surprise fee when you're ready to test.
Premium programs usually bundle one or both exams, mock tests, and application support, which saves you time and money long term.
4. Platform and Software Integration
Courses hosted on platforms like Thinkific or Teachable are cheaper to deliver and often lack software simulation or interactive assignments. Programs that use proprietary dashboards with real EHR or billing interfaces are more expensive—but they’re also far more valuable when it comes to landing your first job.
Hidden Costs Most Don’t Notice
Many students budget for the cost of a medical billing and coding class—but forget to account for the additional expenses that stack up after enrollment. Some of these are predictable, while others are buried in fine print or deliberately left out of the advertised tuition. Knowing what to expect helps you avoid surprise charges and assess the real investment you’ll need to make to get certified and job-ready.
Materials, Certification, Renewal, Practice Tools
1. Required Books and Code Manuals
If your course doesn’t include official CPT, ICD-10-CM, and HCPCS books, you’ll need to buy them separately—and they’re not cheap. A full set of updated code manuals can cost $180 to $300, depending on whether you're buying AAPC-approved editions or bundling for both coding and billing prep.
Many low-end or stripped-down courses leave these out, meaning students can’t even complete assignments or mock exams without spending hundreds extra.
2. Certification Exam Fees
The CPC or CPB exam isn’t always included in course tuition. If your provider doesn’t bundle it, you’ll need to pay $399–$499 per exam directly to AAPC. That doesn't include membership fees (another $140/year), which are required to sit for the exams.
Some programs market low tuition but skip certification entirely—leaving students “trained” but unable to test without registering and paying separately.
3. Software Licenses and Practice Interfaces
If you want to simulate real-world billing or coding workflows, you’ll need access to software platforms like Availity, Kareo, or mock EHR environments. Courses that include simulated billing tools or SOAP note documentation prep tend to be more expensive—but they also replace the need for third-party tools after you graduate.
Without built-in tools, you may need to pay $20–$60/month for coding platforms or claim software just to stay sharp during your job search.
4. Recertification and Continuing Education
Once you're certified, maintaining that certification requires CEUs (Continuing Education Units) and renewal fees. AAPC requires:
18 CEUs per year for CPC
36 CEUs every two years for dual certifications
Plus annual membership fees
Many students don’t budget for these ongoing requirements. If your training provider offers CEU modules or renewal support, that can save you $200–$500 per year depending on how you source credits.
5. Retake Fees and Add-On Coaching
If you fail your exam, you’ll pay for a retake. Some programs offer one free retake, but many do not. That’s another $299–$399, plus more if you need private tutoring or crash-course prep.
Courses like AMBCI’s CPC + CPB certification avoid this by bundling in exam prep tools, live reviews, and mock assessments, so you’re less likely to face repeat charges.
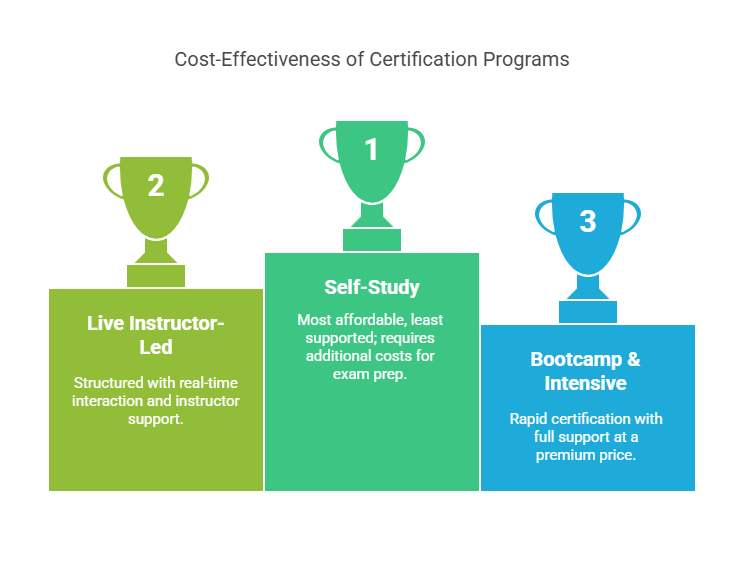
Cost Comparison: Self-Study vs Live vs Bootcamp
Choosing between self-paced, live, and bootcamp-style programs isn’t just about preference—it directly affects how much you’ll spend, how fast you’ll finish, and how prepared you’ll be to pass your exam. Each format has strengths and trade-offs, and the one you choose should reflect both your learning style and your long-term certification goal.
Time vs Money Tradeoffs
1. Self-Study Programs ($399–$1,200)
Self-study courses are the most affordable, but also the least supported. You’ll typically get:
Access to video modules and PDFs
Zero or limited instructor feedback
No guaranteed exam voucher or resume support
While this path might only cost you a few hundred dollars upfront, you’ll need to pay separately for:
AAPC membership
CPC/CPB exam registration
Coding books and practice tools
Optional mock exams or retake coaching
In reality, a $599 self-study course may cost $1,300+ by the time you’re truly ready for the exam. Most people using this path take longer to complete their training and may need to retake the exam—adding both time and money to their total.
2. Live Instructor-Led Courses ($1,500–$3,000)
Live courses offer more structure with real-time interaction, set schedules, and access to a certified instructor. These are great for students who:
Need deadlines to stay on track
Value Q&A access for difficult topics
Want support through registration and resume building
The added cost usually covers:
Exam voucher
Instructor-guided case reviews
Graded assignments and CEU-ready modules
Live programs often finish faster because you’re being paced. Many complete in 8–12 weeks, compared to self-paced learners who may take 4–6 months.
3. Bootcamp & Intensive Programs ($3,000–$5,500+)
Bootcamps promise rapid certification with full support—but you’re paying top dollar for speed and branding. These often include:
Dual-cert prep (CPC + CPB)
Live classes (virtual or in-person)
Dedicated mentor check-ins
Interview prep and career guidance
While the sticker price can be steep, the total value may exceed a patchwork of cheaper programs—especially if it includes exam fees, software simulation, job help, and lifetime access.
That said, some bootcamps don’t include all core features—so a $4,000 price tag without real claims practice or ongoing access could still be a poor deal. You’re paying for the label, not always the outcome.
What You Should Pay For: Must-Have Inclusions
Not every expensive course is worth the price—and not every affordable program is a smart deal. The real value of any medical billing and coding class comes down to whether it includes the essential tools, training, and support you need to pass your exam and start working. If a course doesn’t include these five elements, you’re either overpaying—or heading toward unnecessary delays and hidden costs.
Real Claims, Software, Job Help, Certification Access
1. Practice with Real Claims and Mock Charts
You should never be learning only through slides and lectures. Any serious program must include hands-on assignments using mock patient charts, SOAP notes, and real-life claim examples. If you’re not working through:
Modifier use
Denied claim correction
ICD-10 specificity
...then you're not preparing for the real exam or job tasks. Employers—and certification boards—expect practical accuracy, not just textbook knowledge.
2. Software Simulation or Platform Training
Top-tier courses give you access to mock billing systems or EHR simulations. You should be learning how to:
Pull data from documentation
Apply coding logic inside charting interfaces
Build and correct CMS-1500 forms or claims
Without this, you’ll struggle in your first job—especially in remote or multi-specialty roles. Some programs include access to platforms like Kareo, Availity, or custom simulators, which can add real-world readiness without requiring actual clinic access.
3. Instructor Access and Assignment Feedback
Even if you prefer self-paced study, you still need someone to review your work and correct your logic. Look for programs that offer:
Assignment grading
1-on-1 coaching (even if limited)
Weekly check-ins or live Q&A
Courses like AMBCI’s CPC + CPB program include feedback loops so you know whether your codes, bundling, or billing logic actually meets exam standards—before you test.
4. Exam Bundle or Registration Guidance
You shouldn’t have to figure out how to register for the CPC or CPB exam on your own. A quality course should either:
Include your exam voucher
Or walk you through the AAPC or NHA registration process
The best programs offer bundled pricing that saves you $400–$500, covers your membership, and ensures you’re not delayed by paperwork errors or scheduling gaps.
5. Resume Help, Job Search Guidance, or CEU Support
Passing the exam is step one. Getting hired is step two. A complete course will help you with:
Building a keyword-optimized resume
Listing CEUs or training on your LinkedIn
Navigating entry-level job boards and freelance leads
These are what turn a certification into a paycheck. If your course ends the moment you pass the exam, it’s not a full-scope solution.
Why Dual Certification Lowers Your Total Cost Long-Term
Many students wonder if they should start with just one certification—usually CPC or CPB—and then return later for the other. But the reality is, that piecemeal approach usually ends up costing more in time, money, and missed opportunities than taking both together through a bundled course.
Standalone programs often charge $1,000–$2,000 per certification, not including exam fees, books, or practice tools. When you pursue them separately, you’ll pay twice for enrollment, twice for exam prep, and often get duplicate modules across both courses.
In contrast, a bundled program like AMBCI’s CPC + CPB course gives you:
One streamlined learning path (no repeated content)
Dual exam prep in a single platform
Real claims work that covers both coding and billing logic
A cost savings of $1,000–$2,500 compared to separate enrollments
It also accelerates your earning power. Dual-certified graduates often qualify for higher-paying hybrid roles immediately—whereas single-cert holders may have to gain experience and retrain later just to access the same jobs.
If your goal is long-term career flexibility and income growth, dual certification isn’t an add-on—it’s the smartest way to start.
What do you care about most in a medical billing & coding program?
AMBCI Delivers Maximum Value with Transparent Pricing
When you’re evaluating medical billing and coding programs, what you’re really buying isn’t just training—it’s exam readiness, job access, and income protection. Most providers either overcharge for shallow content or undercharge by leaving out essential pieces. AMBCI fixes that by delivering a premium dual-certification pathway with zero hidden costs and everything bundled up front.
If you're serious about getting certified and getting hired, AMBCI’s CPC + CPB course is the clearest, most cost-efficient way to do both—without worrying about surprise add-ons.
No Upsells, Exam Bundled, 200+ Specialty Lessons
You don’t pay extra for exam access. You don’t get charged separately for coding tools. And you’re not upsold halfway through just to get feedback or mock test support. With AMBCI, one price gives you:
Full CPC + CPB curriculum (aligned with AAPC exam standards)
Official exam voucher included
Unlimited access to graded assignments and live reviews
200+ specialty modules covering orthopedics, psych, OB/GYN, telehealth, and more
Hands-on practice using mock claims, SOAP notes, and audit-style case reviews
Other programs charge $300–$600 extra for specialty coding or claims exercises. AMBCI builds that in from day one—because the more coding variation you see during training, the more flexible you’ll be as a job candidate.
Pay-Over-Time Options, Lifetime Access
No student should have to delay certification because of price. AMBCI offers flexible monthly payment plans so you can start now, pay gradually, and avoid credit-based finance traps. There’s no tuition creep, no upgrade pressure, and no expiring access.
Most courses cut off access 6 or 12 months after you enroll, which forces students to rush or pay to extend. AMBCI gives you lifetime access, so you can revisit modules whenever your career grows into new specialties, or when it’s time to earn CEUs.
More importantly, AMBCI isn’t just about the exam. It’s about making sure you:
Pass the first time
Know how to apply your skills in live payer workflows
Can land jobs across both billing and coding tracks
Or build a freelance practice with legitimate client-ready skills
If your goal is long-term income, security, and flexibility, there’s no smarter investment than a CPC + CPB program that includes every tool you need to succeed—without surprise costs down the line.
Final Thoughts
Medical billing and coding classes vary in price, but the numbers only matter if you know what they include. A cheap program without exam access, mentorship, or real claims training can end up costing you more in retakes, delays, and lost job opportunities. On the other hand, an expensive program without practical tools or lifetime access can leave you overpaying for short-term results.
The smartest investment is one that gives you complete training, full certification prep, live instructor support, and no surprise fees. That’s where AMBCI’s CPC + CPB course delivers. You get dual certification training, 200+ specialty modules, mock claims, resume help, and both exams included—at a single, transparent price.
If you want to become certified and job-ready without wasting time or money, this is the clear path forward.
Frequently Asked Questions
-
To qualify for a job in medical billing, you typically need three things: a recognized certification, hands-on training, and knowledge of payer systems. The most respected credential is the Certified Professional Biller (CPB) from AAPC, which signals to employers that you understand claims submission, insurance protocols, denials, and HIPAA compliance.
Some employers will accept experience in place of certification, but most remote and mid-level billing positions now require formal credentials. Beyond certification, employers want proof that you can:
Submit clean claims
Manage multi-payer workflows
Use billing software (e.g., Kareo, AdvancedMD)
Courses like AMBCI’s CPB or CPC + CPB track prepare you for this directly by including live billing practice, graded mock claims, and software walkthroughs—ensuring you're not just certified but truly job-ready.
-
Medical billing skills include the technical and analytical abilities required to submit accurate claims, manage payment cycles, and reduce denials. Core skills employers expect include:
Knowledge of CPT, ICD-10-CM, and HCPCS codes
Insurance verification and eligibility logic
Denial management and appeal handling
Familiarity with clearinghouses and payer portals
Billers must also know how to spot mismatched codes, identify claim edits, and follow compliance rules for documentation. Software fluency (e.g., Availity, Kareo, Office Ally) is now considered a baseline requirement.
Courses that focus on real-case training—not just theory—build these skills faster. Programs like AMBCI’s CPB certification train you through real charting and billing assignments, which makes your skills transferable to clinics, hospitals, and remote RCM roles right away.
-
Billing coding is the combined process of assigning medical codes to services and translating them into billable claims. Coders analyze physician documentation and convert diagnoses and procedures into standardized CPT, ICD-10-CM, and HCPCS codes. Billers then use those codes to submit claims to insurers, manage payments, and ensure reimbursement.
In short, coding makes the service billable—and billing gets it paid.
Professionals who do both are often called revenue cycle specialists or medical billing and coding professionals. Certification in both CPC and CPB allows you to handle this full cycle.
Courses that prepare you for both ends—like AMBCI’s dual-certification program—make it easier to secure remote, hybrid, or high-paying compliance positions. Most employers prefer candidates who understand both documentation and reimbursement because they reduce errors and accelerate revenue.
-
There’s no formal degree requirement to become a medical biller. Instead, the eligibility process involves:
Completing a recognized training program
Earning a certification (usually CPB from AAPC)
Building hands-on experience through course assignments or on-the-job practice
Many employers require CPC or CPB certification, especially for remote roles or positions handling multiple specialties. Some entry-level jobs may hire uncredentialed candidates, but they often offer lower pay and limited growth.
A good course—like the one offered by AMBCI—walks you through exam registration, AAPC membership setup, and CEU requirements. It also provides the real-world practice needed to qualify for mid-level roles from day one. With bundled exam fees and live prep, the process becomes faster, more affordable, and easier to complete without delays.
-
There are two main types of medical billing:
Professional billing, used for individual providers like physicians, therapists, or clinics. This is typically submitted using the CMS-1500 form and includes CPT and ICD-10 codes.
Institutional billing, used by hospitals or large facilities. This uses the UB-04 form and includes revenue codes, DRGs, and additional facility-specific data.
Each type has different payer rules, documentation formats, and compliance risks. Some professionals specialize in just one, while others learn both to increase their hiring flexibility.
Programs like AMBCI’s CPC + CPB course focus heavily on professional billing but expose students to elements of institutional billing to help them qualify for a wider range of jobs—including remote and hospital-affiliated coding positions.
Understanding both types increases your ability to work in multi-specialty, payer-facing, or audit-prep roles, which pay significantly more than generalist positions.