Medical Billing and Coding Certification Programs: What’s Included?
A proper certification program doesn’t stop at theory. It must cover code systems in depth, real-world billing logic, hands-on software training, live claim practice, and mock audit cycles—because that’s what employers expect from day one. If you’re missing any of those, you’re not job-ready.
This breakdown cuts through the marketing and shows you exactly what top-tier billing and coding programs include, what to demand from any course, and how to know if a certification actually prepares you for the CPC, CPB, or dual-track medical coding roles you’re aiming for.
Core Curriculum Breakdown
The foundation of any medical billing and coding certification program is its curriculum—and this is where programs either launch your career or quietly sabotage it. The best certifications don’t just teach you what codes exist—they teach you how to use them in real billing situations, how to avoid denials, and how to document for compliance audits. If a program skimps on these fundamentals, you won’t be prepared for real-world billing logic or AAPC/AMA exam standards.
Here’s a detailed breakdown of the three most critical content pillars every high-level billing and coding program should include.
CPT, ICD-10-CM, and HCPCS
At the center of all coding training are the three core code systems:
CPT (Current Procedural Terminology): Used to report services provided by physicians and outpatient settings. You’ll learn how to choose the right CPT codes for everything from office visits to surgical procedures, and how to avoid upcoding or undercoding, which directly impacts claim rejections or audits.
ICD-10-CM (Diagnosis Coding): This is where most beginners struggle. You must learn how to assign specific diagnostic codes that reflect patient conditions with clinical accuracy—and how to navigate tabular lists, conventions, and exclusions with speed and precision.
HCPCS (Healthcare Common Procedure Coding System): Essential for durable medical equipment (DME), Medicare billing, ambulance services, and supplies not covered under CPT. Most underqualified coders fail here because their training lacks real-case exposure to how these codes appear in payer requirements.
You’re not just memorizing code books—you’re learning how to use each system together, accurately, and under payer scrutiny.
Claims, Denials, and Payer Protocols
Great coders don’t just code—they understand the entire claim lifecycle. That includes:
Form completion (CMS-1500 and UB-04)
Insurance verification workflows
Claim submission timing and tracking
Denial reasons and appeals handling
You should be trained to identify what causes soft vs. hard denials, how to analyze explanation of benefits (EOBs), and how to modify claims for resubmission. Most job rejections happen not due to missing codes, but because coders can’t manage payer communication or insurance-specific protocols.
Advanced programs like the CPC + CPB dual-certification path teach students how to work across Medicare, Medicaid, private insurance, and workers’ comp billing, which is the real-world diversity you’ll face in clinics and hospitals.
Compliance, Auditing, and Ethics
No coder is safe from audits. You must be prepared from day one to protect both your employer and your own job. That means understanding:
OIG compliance guidelines
The basics of medical necessity and documentation justification
Recognizing fraud, waste, and abuse triggers
Internal audit cycles and chart review workflows
You’ll be trained in coding to support medical necessity, documenting appropriately for appeal, and spotting red flags before claims are submitted. If your course skips this, you’re walking into your job blind to legal risk.
A serious billing and coding curriculum teaches you how to code ethically, defend your work in audits, and meet payer compliance at every step.
Tools and Software Training
Knowing how to code means nothing if you can’t apply it inside the tools that real billing and coding professionals use every day. Software training is no longer optional—it’s the skillset that gets you hired or rejected in the first five minutes of a job interview. Strong medical billing and coding certification programs embed software literacy directly into their curriculum, so you can chart, code, and submit with confidence the moment you're hired.
Here are the core platforms and tools your training must include—and why they matter.
EHRs, Billing Portals, Audit Logs
1. Electronic Health Records (EHRs)
You must learn how to navigate at least one major Electronic Health Record (EHR) system. Employers expect coders to extract diagnosis codes, procedure notes, and clinical data directly from the EHR. The most commonly used platforms include:
Epic
Cerner
Athenahealth
eClinicalWorks
Your program should include sandbox access or simulations that allow you to:
Pull diagnosis and treatment information
Match notes to CPT/ICD-10 codes
Navigate from encounter history to claims
If your training doesn’t include actual EHR usage, you’ll be slower—and more error-prone—than job-ready candidates.
2. Billing Portals and Clearinghouses
Beyond coding, you must know how to:
Submit claims through platforms like Availity, Kareo, or PracticeSuite
Check payer-specific requirements before submission
Resubmit corrected claims post-denial
Strong certification programs walk you through how to build and submit a full claim using real templates and live clearinghouse rules. Understanding real-time eligibility checks, billing queue workflows, and insurance plan validation are critical for fast claim turnaround.
3. Audit Logs and Internal Review Tools
You should also learn how to work within:
Audit log reports that track claim modifications
Compliance dashboards that flag code discrepancies
Internal review forms used during peer audits
High-level programs include mock audit labs, where you practice spotting documentation gaps, modifier misuse, or bundled billing violations—before those issues trigger payer penalties.
Why Software Fluency Equals Job Readiness
Employers don’t have weeks to train you on tools. If your resume doesn’t show you’ve already worked inside EHRs, billing software, and claim tracking platforms, they’ll move on to someone who has. Certification without system experience is a red flag.
That’s why AMBCI’s CPC + CPB dual-certification program trains students inside simulated interfaces that reflect actual hospital and clinic workflows—not just codebooks and theory.
If you want recruiters to take your application seriously, your software fluency must be real, recent, and replicable.
| Category | Key Platforms | Why It Matters |
|---|---|---|
| Electronic Health Records (EHR) | Epic, Cerner, Athenahealth, eClinicalWorks |
Enables extraction of diagnosis and procedure data directly from patient encounters. Trains you to map clinical notes to CPT/ICD-10 codes. Vital for accurate and efficient claim generation. |
| Billing Portals & Clearinghouses | Availity, Kareo, PracticeSuite |
Teaches real-world claim submission, payer rules, and denial resubmissions. Prepares you to handle billing queues and validate insurance plans. Critical for reimbursement speed and accuracy. |
| Audit Logs & Review Dashboards | Internal Audit Tools, Compliance Reporting Systems |
Simulates peer audits, modifier misuse detection, and bundled billing violations. Builds documentation accuracy and error prevention. Essential for avoiding payer penalties and maintaining compliance. |
Hands-On Practice: What to Expect
What separates a certificate-holder from a hireable billing and coding professional isn’t theory—it’s execution under simulated pressure. Employers aren’t just hiring someone who “knows the codes.” They want someone who can take a real chart, identify errors, apply the correct codes, and submit a claim that won’t bounce back. The only way to build this confidence is through hands-on, structured practice embedded into your training program.
If your certification doesn’t include these components, you’re walking into the job market untested.
Case Studies, Real Claims, and Worksheets
1. Case-Based Coding Assignments
You should expect your training to include:
Dozens of specialty-specific case studies
Encounters pulled from common fields like orthopedics, pediatrics, dermatology, and cardiology
Practice converting real-world notes into CPT, ICD-10-CM, and HCPCS codes
Each case should be accompanied by:
A full patient history and encounter summary
Provider notes with intentional ambiguity or missing info
Worksheets that simulate real documentation gaps
This kind of challenge teaches you how to code around incomplete or confusing provider language, which happens frequently in practice.
2. Full Claim Lifecycle Exercises
Beyond identifying codes, you need to practice:
Filling out CMS-1500 and UB-04 claim forms by hand and digitally
Submitting test claims into simulated clearinghouses
Handling common rejections, denials, and “pending” flags
Look for programs that let you submit and correct mock claims, so you’re comfortable not just with clean submissions, but with the fixing process—where most coders fall short on the job.
3. Cross-Checking with Documentation Standards
Your worksheets should teach you how to:
Justify codes based on supporting documentation
Spot mismatches between diagnostic and procedural claims
Use audit tools to pre-check your work before “sending” the claim
Programs like AMBCI’s CPC + CPB certification require students to complete graded, scenario-based exercises—many of which are reviewed by certified auditors. This feedback loop builds real-world awareness of billing risk, fraud flags, and best-practice justification.
Why This Practice Actually Matters
On-the-job coding isn’t clean. You’ll rarely have perfect notes, and you’ll constantly need to ask:
Is this code justifiable?
Is this claim clean enough to pass Medicare filters?
Does the payer allow this combination of codes for this procedure?
Only hands-on, case-based practice gives you the instincts to answer those questions fast—before you make a mistake that costs your employer money or risks legal exposure.
If your certification skips this step, you’re not trained—you’re just technically informed. And in today’s hiring landscape, that’s not enough to get past a coding interview.
Exam Prep and Career Coaching
Even the most content-rich certification program is incomplete without a structured path to passing your exams and landing your first job. That’s why the best medical billing and coding programs don’t just teach codes—they walk you through how to pass the CPC, CPB, or dual-certification exams, and how to position yourself as a strong hire the moment you’re certified.
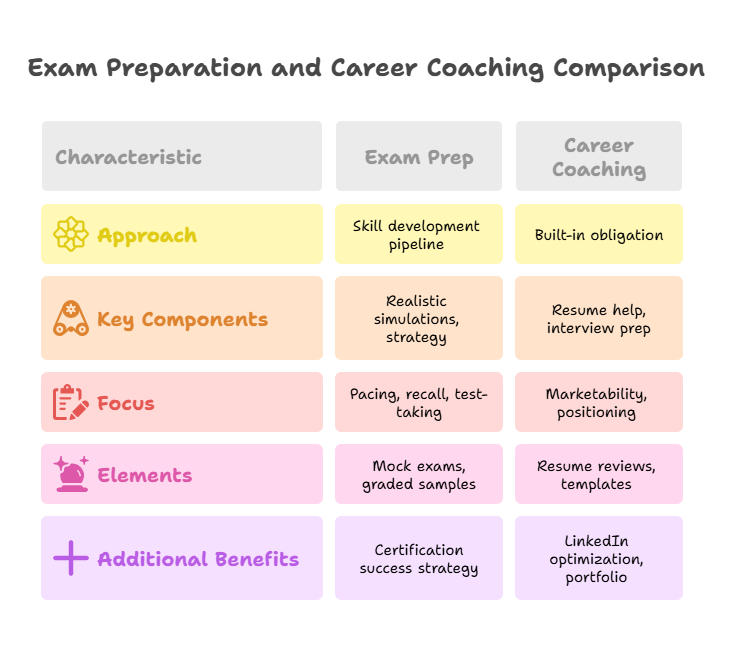
Strong programs approach exam prep as a skill development pipeline, not a guessing game. And they treat career coaching as a built-in obligation, not a post-course upsell.
Mock Tests, Resume Help, Interview Prep
1. Realistic CPC and CPB Exam Simulations
A great program includes:
Timed, full-length mock exams that simulate the CPC and/or CPB structure
EHR-based simulations that reflect real coding encounters
Access to graded charting samples with breakdowns of what went right—or wrong
For example, AMBCI’s CPC + CPB program embeds mock exams at key checkpoints, ensuring you’re building pacing and recall as you move through the course—not just cramming at the end. You learn not just how to choose codes, but how to navigate through distractors, multiple correct answers, and legally sensitive gray areas—just like you’ll face on the test.
2. Certification Success Strategy
Most people fail certification exams not due to lack of knowledge, but due to test fatigue, pacing errors, or misreading chart-based scenarios. A real prep system trains you on:
Time-boxing each section and tracking completion velocity
Skimming for high-yield information in exam case notes
Using answer logic and elimination methods when uncertain
Smart prep isn’t about doing more questions—it’s about understanding how the exam is built to test how you think under pressure. A program that doesn’t simulate this won’t get you ready.
Career Coaching That Moves You Into a Job
Passing the exam isn’t the finish line—it’s the start of your marketability. Which is why the best programs include:
1-on-1 resume strategy reviews from coders or healthcare HR professionals
Interview prep focused on behavioral, technical, and EHR questions
Pre-written resume and cover letter templates tailored to remote billing, hospital coding, or specialty clinics
You’ll also learn how to:
Showcase your software fluency (Epic, Cerner, clearinghouses)
List your mock claim submissions and audit logs on a resume
Frame certification + training as equivalent to experience
AMBCI’s course, for instance, includes personalized LinkedIn optimization sessions, portfolio feedback, and employer-specific positioning strategies—so you’re not just certified, you’re shortlisted.
Why This Support Determines Your ROI
Many students choose cheaper courses thinking they’re saving money. But when those programs fail to get them past the exam—or leave them guessing during the job hunt—the cost doubles in time and lost income.
Programs with built-in exam simulation and job-market coaching drastically increase pass rates, reduce time-to-hire, and help you step into the workforce fully prepared.
If your certification doesn’t guide you through both the test and the hiring funnel, it’s not complete—and you’ll feel that gap the moment your resume hits a real employer’s desk.
What matters most to you in a billing & coding certification program?
Self-Paced vs Live: Learning Format Matters
When choosing a medical billing and coding certification program, most learners focus on curriculum content—but format matters just as much. How the course is delivered directly affects how well you retain information, how fast you finish, and how prepared you are for exams and job interviews. The wrong format can stall your progress, while the right one accelerates both comprehension and placement.
Both self-paced (asynchronous) and live (synchronous) formats have their advantages—but they serve different learner types. Understanding the trade-offs ensures that your format matches your schedule, learning style, and professional goals.
Asynchronous vs Synchronous Trade-Offs
1. Self-Paced (Asynchronous) Programs
Self-paced programs are designed for flexibility. You get instant access to all course materials and can complete them on your own time, at your own speed. This is ideal for:
Full-time workers or students juggling multiple responsibilities
Independent learners who don’t need reminders or scheduled sessions
Those in different time zones who can’t attend live classes
Key strengths:
Complete at your own pace—often in 4 to 12 weeks depending on your schedule
No pressure to “keep up” with a cohort
Rewatch modules or redo practice cases multiple times
However, self-paced doesn’t mean “solo.” High-quality asynchronous programs like AMBCI’s CPC + CPB certification still include:
Live mentoring via chat, email, or scheduled Zoom sessions
Graded assignments with instructor feedback
Built-in accountability check-ins to track progress
What separates effective self-paced formats from passive ones is structure. If the program just dumps videos without real evaluation, your performance will plateau. Look for platforms that simulate job tasks, provide real EHR exercises, and offer access to instructors when you hit roadblocks.
2. Live (Synchronous) Programs
Synchronous programs follow a real-time schedule. You attend instructor-led sessions at specific times—usually over Zoom or in-person cohorts. These are best for:
Learners who benefit from immediate Q&A and group learning
People who struggle with staying motivated on their own
Those who want the closest possible replication of a classroom environment
Key advantages:
Structured routine keeps you on track
Live demonstrations of coding, form completion, or mock claim reviews
Peer interaction and collaborative discussion improve engagement
But live formats have downsides:
Less flexibility (miss a session, and you're playing catch-up)
Slower overall course completion
Often more expensive due to instructor availability and scheduled hours
Programs like AMBCI solve this by offering a hybrid format—self-paced core modules paired with optional live coaching, Q&A sessions, and assignment reviews, so learners get the best of both systems.
Choosing the Right Format for You
Ask yourself:
Do I need external structure or can I self-manage deadlines?
Will I realistically study 5+ hours a week without live accountability?
Do I prefer watching demos, or doing hands-on cases at my own pace?
If you want to fast-track your certification without losing quality, structured self-paced programs with integrated support and feedback loops offer the best ROI.
| Category | Included Features | Why It Matters |
|---|---|---|
| Core Curriculum | 200+ specialty-specific lessons | Covers outpatient, inpatient, and advanced specialties like cardiology, orthopedics, psychiatry |
| Case-based SOAP analysis and charting walkthroughs | Builds real-world fluency instead of just theory or code memorization | |
| Claims, appeals, modifiers, and payer compliance training | Prepares you for real-life claim cycles, documentation, and payer rules | |
| Exam Prep & Mentorship | Full CPC + CPB mock exams | Practices timing, stress management, and blueprint accuracy |
| Live mentor access for questions and feedback | Certified instructors support you in applying tricky concepts | |
| Graded claims with custom instructor feedback | Refines your submissions with real coding insight | |
| Exam pacing benchmarks and study timelines | Helps track weekly progress and avoid cramming pitfalls | |
| Job-Ready Career Support | Billing/coding resume review + LinkedIn optimization | Makes you instantly credible to recruiters and HR systems |
| Cover letter templates for clinical & remote roles | Saves time and helps tailor your pitch for billing/coding jobs | |
| Portfolio building with mock claims, EHR samples, audit prep | Lets you showcase your work to employers during interviews | |
| Lifetime access to course updates and instructor Q&A | Keeps your credentials and skills fresh post-certification |
What You Get in AMBCI’s CPC+CPB Program
The AMBCI CPC + CPB Dual Certification Program isn’t just a bundle—it’s a fully structured training ecosystem that moves you from zero experience to fully job-ready across both billing and coding. While many programs only prepare you for one certification or skip real case practice, AMBCI’s course is built to help you pass both exams, build real-world fluency, and get hired faster.
This program doesn’t leave learning outcomes to chance. It integrates specialty-specific training, guided support, and exam-focused evaluation into every module—so you’re not just taking a course, you’re building a career foundation that recruiters take seriously.
200+ Specialty Lessons, Live Mentoring, AAPC Exam Prep
At the core of the AMBCI program are:
200+ modular lessons spanning general, outpatient, and specialty billing and coding
Focus areas include cardiology, orthopedics, dermatology, psychiatry, pediatrics, and more
Deep dives into claims management, appeals, payer compliance, and modifier use
Each section includes real EHR charting examples, video walkthroughs, and case-based SOAP analysis, so you’re not memorizing—you’re applying.
You’ll also receive:
Live mentoring access with certified instructors for clarification or charting feedback
Multiple full-length CPC and CPB mock exams
Time-tracking benchmarks to help you pace your exam prep and practice under stress
Graded claim review exercises with customized instructor guidance
The entire course is tailored to the AAPC’s latest CPC and CPB exam blueprints, meaning every module you complete directly builds toward the scoring areas you’ll be tested on.
One Course, Two Certifications, Full Job Support
Earning both CPC and CPB together doesn’t just make you more marketable—it increases your eligibility for roles in:
Hospital billing departments
Multi-specialty clinics
Outsourced coding firms
Revenue cycle compliance teams
After passing your exams, AMBCI gives you tools to actually secure a role—not just a PDF certificate. That includes:
Resume reviews tailored to billing/coding roles
LinkedIn profile feedback and keyword optimization
Pre-written cover letter templates for remote and clinical coding jobs
Portfolio-building guidance so you can showcase EHR documentation, mock claims, and audit preparation work
Because the course is CPD-accredited and exam-aligned with AAPC standards, your credentials will be recognized in U.S. and international healthcare systems, with lifetime proof of training.
Most importantly, you’re not going through this alone. Even after passing the certification, you’ll still have lifetime access to updates, refresher modules, and instructor Q&A—so you can remain sharp and certified, no matter how the industry evolves.
Final Thoughts
A medical billing and coding certification program isn’t just about what’s written in the brochure. It’s about what you walk away with: fluency in CPT, ICD-10, and HCPCS, confidence in handling real claims, and readiness to pass two of the toughest exams in the healthcare revenue cycle space.
Many programs teach enough to get you to the exam—but not through it. Even fewer prepare you for what happens after certification: real EHR systems, insurance denials, audit reviews, and employer expectations. That’s why curriculum structure, format, tools, and job support matter just as much as exam prep.
The AMBCI CPC + CPB Dual Program is built for professionals who want a full-scope, employer-ready edge—not a passive certificate. You learn it, prove it, and apply it the moment you’re hired.
If your goal is real billing and coding fluency—not just another course—you now know what to look for. Don’t settle for surface-level. Invest in a program that makes you undeniable.
People Also Ask
-
CPC (Certified Professional Coder) and CCS (Certified Coding Specialist) serve different roles. CPC, offered by the AAPC, is ideal for those pursuing outpatient and physician-based coding roles. It’s the industry standard for medical coders working in clinics, private practices, or ambulatory settings. CCS, offered by AHIMA, is more hospital-oriented, focusing on inpatient facility coding and often requires deeper knowledge of DRGs, POAs, and inpatient coding logic.
If you're new to the field or aiming for broader outpatient roles, CPC is the more accessible and job-rich path. It’s also more widely recognized in remote and telehealth roles. CCS has more depth but is often pursued as a second-tier credential after experience.
-
Medical billing professionals in managerial roles earn the most, especially those who transition into revenue cycle management (RCM), compliance auditing, or payer negotiation positions. Senior billing analysts, claim denial experts, and billing leads at hospitals can earn $60,000–$85,000+ annually, especially with dual credentials like CPC + CPB.
Freelance medical billers with their own client base or those offering end-to-end billing services for private practices can also command high rates—sometimes $35–$60 per hour, depending on region and specialization. Specialties like orthopedics, cardiology, and neurology also pay higher due to coding complexity. More income often correlates with deeper payer protocol knowledge and multi-specialty exposure.
-
The most crucial skill is accurate code selection under clinical ambiguity. That means being able to:
Interpret unclear provider notes
Navigate multiple correct coding paths
Understand when documentation doesn’t meet medical necessity
Beyond memorization, coders must master critical thinking, especially when working with bundled procedures, modifiers, and medical necessity validation. You’ll also need EHR fluency, since coders work directly within charting systems like Epic or Cerner.
Strong grammar and documentation review skills matter too—many denials stem from mismatched codes and insufficient justification. A coder who knows how to connect clinical intent to payer requirements is far more valuable than one who just knows the books.
-
The “best” field depends on your goals. Here’s how specialties stack up:
Outpatient coding (CPC): Fastest to enter, huge remote market, consistent demand
Inpatient coding (CCS): Higher complexity, often pays more, but harder barrier to entry
Surgical/procedural coding: High pay, but requires intense CPT mastery
Radiology, cardiology, dermatology: High volume and specialty pay bumps
Telehealth and mental health coding: Growing fast, ideal for remote coders
For beginners, outpatient coding with CPC certification is the most versatile and accessible. From there, you can specialize based on your interests or income targets. Dual certification in CPC + CPB makes you more flexible and employable across fields.
-
Successful coders are:
Detail-oriented — small errors can lead to large denials
Independent learners — coding requires regular self-updating
Analytical thinkers — it’s not just copying; it’s about interpreting intent
Comfortable with routine — many tasks are repetitive but require consistency
Confidentiality-focused — handling PHI demands discretion and ethics
If you enjoy solving logic problems, organizing data, and working with structure and accuracy, coding is a strong fit. You don’t need to be outgoing or tech-savvy—you need to be focused, ethical, and resilient under information-heavy tasks.