Future Opportunities for Coders in Clinical Documentation Improvement (CDI)
Today, coding goes far beyond assigning CPT or ICD codes. Modern CDI demands an understanding of value-based reimbursement, patient safety metrics, and the intersection of healthcare data with clinical accuracy. As shared by healthcare leaders in the 2025 billing landscape Q&A, documentation specialists who can blend coding expertise with analytical insight will be highly sought after.
If you are preparing for your medical billing and coding certification exam, this is the perfect time to look at how CDI can expand your career. Coders equipped with CDI skills are not only advancing in traditional roles but also moving into consulting, auditing, education, and healthcare IT. Whether you plan to work in hospitals, private practices, or telehealth, CDI expertise gives you a future-proof advantage.
Below, we’ll dive into the future opportunities for coders in CDI, explore growth areas, and outline the certifications and skills you’ll need to thrive.
1. Why CDI Is the Future of Medical Coding
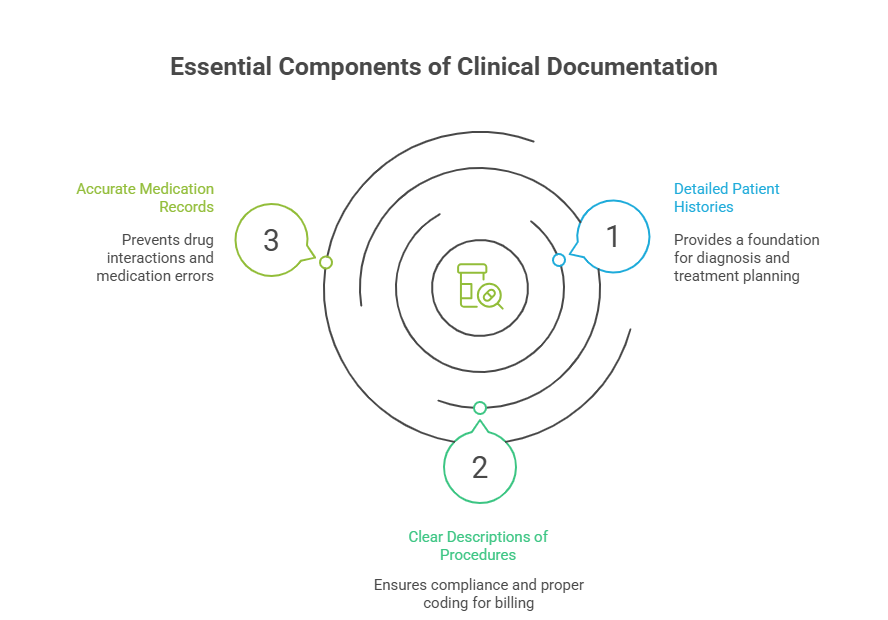
CDI ensures that patient records are complete, accurate, and reflective of true clinical care. This impacts reimbursement, compliance, and patient safety. As healthcare shifts from fee-for-service to value-based care, CDI is becoming essential for providers to avoid revenue loss and penalties.
Coders transitioning into CDI will play a key role in:
Improving hospital reimbursement rates.
Ensuring accurate reflection of patient acuity.
Reducing claim denials and audits.
Supporting clinical research and quality initiatives.
Many coders underestimate CDI, thinking it belongs only to physicians. But with guidelines for accurate clinical documentation expanding, certified coders are uniquely positioned to step into these roles.
| Career Role | Primary Responsibilities | Certification Recommended | Salary Range (2025–2030) |
|---|---|---|---|
| CDI Specialist | Review and improve clinical documentation for accuracy | CCDS, CPC | $72,000–$90,000 |
| Inpatient CDI Coder | Focus on hospital-based records and DRG validation | CCDS, CCS | $78,000–$95,000 |
| Outpatient CDI Coder | Specialize in clinics and ambulatory care | CPC, COC | $65,000–$80,000 |
| Compliance Auditor | Ensure adherence to federal and payer regulations | CPMA, CHC | $75,000–$92,000 |
| Revenue Integrity Analyst | Optimize reimbursement and reduce denials | CRCR | $70,000–$85,000 |
| Healthcare Data Analyst | Analyze CDI-related metrics and trends | RHIA, RHIT | $80,000–$100,000 |
| Clinical Coding Educator | Train coders on CDI requirements | CPC-I, CCS | $68,000–$82,000 |
| Telehealth CDI Specialist | Adapt CDI for remote patient care documentation | COC, CPC | $72,000–$88,000 |
| AI Documentation Analyst | Oversee AI-generated clinical records | CCDS, Informatics | $85,000–$105,000 |
| Denial Prevention Specialist | Resolve issues leading to claim denials | CPMA | $70,000–$86,000 |
| Quality Improvement Officer | Integrate CDI into hospital quality programs | CHCQM | $88,000–$110,000 |
| CDI Consultant | Provide external advisory services to providers | CCDS, CDEO | $95,000–$120,000 |
| Research Documentation Specialist | Support clinical research accuracy | CRCP | $75,000–$90,000 |
| MACRA/QPP Specialist | Align CDI with value-based payment models | MACRA Certification | $82,000–$100,000 |
| Global Health CDI Coder | Support international healthcare organizations | CCDS, ICD-10 CM training | $68,000–$85,000 |
2. The Role of Coders in Reducing Denials
Claim denials cost healthcare billions annually. Coders with CDI skills are critical in preventing these costly errors. A denial often stems from incomplete documentation—not incorrect coding. Coders who master insurance claim adjustment codes and pair them with CDI training will cut denials significantly.
These coders work with physicians to ensure charts justify medical necessity, capture secondary diagnoses, and prevent gaps. Hospitals and practices are actively hiring CDI coders as denial prevention specialists.
3. Telehealth and CDI
The expansion of telemedicine has created new challenges for documentation. Without in-person visits, providers often under-document encounters. Coders who specialize in telehealth CDI ensure that digital consultations are fully captured, coded, and reimbursed.
The telemedicine coding guide already highlights new CPT codes for remote monitoring and e-visits. By 2030, CDI coders in telehealth will be vital to both patient access and provider sustainability.
Which CDI Career Path Interests You Most?
4. CDI and Value-Based Care
Government programs like MACRA and the Quality Payment Program are putting CDI at the center of value-based reimbursement. Coders who understand MACRA and QPP requirements will be in demand for years to come.
Hospitals need CDI specialists to ensure records reflect risk-adjusted patient outcomes. By aligning coding with clinical quality, CDI coders directly influence hospital star ratings and reimbursement bonuses.
5. Skills Coders Need to Transition into CDI
Future CDI coders will need more than just coding expertise. Essential skills include:
Knowledge of clinical workflows and terminology.
Proficiency with electronic medical records and billing software.
Understanding of payer regulations and compliance.
Analytical ability to interpret hospital metrics.
Strong communication skills for physician collaboration.
Adding a CDI-focused certification such as CCDS (Certified Clinical Documentation Specialist) or CDEO (Certified Documentation Expert Outpatient) enhances career prospects significantly.
6. FAQs
-
Yes, but it’s best to first gain coding experience. Many employers prefer coders with 2–3 years of inpatient or outpatient coding before moving into CDI.
-
The CCDS credential is the gold standard, but coders can also benefit from CPC, CCS, and CPMA.
-
No. CDI opportunities are growing in clinics, outpatient centers, and telehealth organizations.
-
Yes. Countries adopting ICD-10 and value-based payment models are increasingly hiring CDI specialists.
-
Projections place CDI salaries between $75,000–$110,000, depending on specialization and experience.
-
Start with essential study strategies for coding students, pursue certifications, and gain hands-on EMR experience.