Is Medical Billing and Coding Certification Worth It? The Honest Answer
The industry strongly favors professionals who have earned an AAPC-certified billing and coding credential, because it proves competence in CPT, ICD-10, and HCPCS usage from day one.
This article is a direct, no-fluff breakdown of the actual value behind getting certified. You’ll learn how it impacts your starting salary, career mobility, and long-term income potential. We’ll dissect the differences between certified and uncertified paths, and whether the return on investment holds up in 2025’s economy. No filler—just what you need to know before enrolling.
The Real ROI of Certification
For anyone entering healthcare support roles, time and money are your two most limited assets. A smart certification should offer fast ROI, measurable job access, and income upside—not just a piece of paper. That’s where billing and coding training stands out. Done right, it gets you job-ready in under six months and starts paying back immediately through higher entry-level salaries and better job mobility. But how does this play out financially, over both the short and long term?
Career salary before vs after
Uncertified entry-level professionals in administrative healthcare jobs often start with salaries in the $29,000–$35,000 range, especially in smaller clinics or outpatient centers. Employers see these hires as high-risk, requiring months of on-the-job training, frequent correction, and external oversight. That’s not a foundation for fast growth.
Once you add an AAPC-accredited billing and coding certification, the picture changes. Starting salaries jump to $43,000–$52,000 depending on location and facility type. Even without prior experience, certified coders get better job offers because they bring recognized skills in CPT, ICD-10, and HCPCS from day one. Within 1–2 years, those same professionals often earn between $55,000–$65,000, particularly in hospitals and insurance firms.
That’s not a minor difference—it’s a 20–35% salary lift just by getting certified before entering the job market.
Job accessibility and employer preference
One of the most under-discussed benefits of certification is access—to interviews, to shortlists, and to actual job roles. Healthcare organizations are under constant pressure to meet compliance and reimbursement requirements, and they don’t have the time to train unprepared staff from scratch. That’s why certified candidates automatically move to the top of the pile.
Hiring managers aren’t just filtering for resumes that mention medical billing—they’re searching for verifiable credentials. An AAPC-certified billing and coding credential instantly tells them you’re proficient in core coding standards and capable of managing EHR systems, claim submissions, and audit documentation without hand-holding.
Across large hospital networks, third-party billing companies, and even telehealth startups, job listings are increasingly requiring certification as a baseline. Not having one doesn’t just limit your starting job options—it often eliminates you from consideration altogether.
How certification accelerates ROI in real life
Most students can complete a billing and coding program in 4 to 7 months, depending on whether they study part-time or full-time. Within two months of certification, the majority land roles that pay back their training cost within the first year. That’s a sharp contrast to nursing or allied health degrees, which often take 2–4 years before breaking even.
Over a 5-year timeline, certified professionals consistently outperform uncertified peers in promotion eligibility, raise percentages, and lateral movement into auditing, compliance, or managerial roles. These compound returns are rarely talked about—but they matter. A strong certification doesn’t just boost your first job—it sets up every job after that.
If you’re choosing between certifications, always ask one question: will this program give me recognized proof of billing and coding mastery? If the answer is yes, and the program prepares you for AAPC-accredited exams, then it’s not just worth it—it’s one of the smartest investments in healthcare right now.
| Factor | Certified Path (e.g., AAPC) | Uncertified Path |
|---|---|---|
| Time to First Job | 30–90 days after certification | 5–7 months longer on average |
| Starting Salary | $43,000–$52,000 | $28,000–$34,000 |
| Salary After 2 Years | $55,000–$65,000 | $35,000–$42,000 (if promoted) |
| Job Application Success Rate | High—often recruited by employers | Low—often filtered out by ATS |
| Break-Even Timeline | 2–4 months (training cost recouped) | No clear break-even (low salary lift) |
| Lifetime Earnings (10 years) | $450,000–$600,000+ | $310,000–$400,000 |
| Advancement Opportunities | Auditor, Compliance Officer, Manager | Limited; often stagnant roles |
| Remote Work Eligibility | High—remote coding roles common | Low—mostly in-office data roles |
Comparing Certified vs Uncertified Paths
When evaluating a career in medical billing and coding, your trajectory can take two distinct paths: certified or uncertified. Both will lead you into the healthcare system, but only one gives you fast-track job access, higher long-term earnings, and employer trust from day one. Understanding these differences helps you make a decision that protects your time, money, and career potential.
Time to job placement
Uncertified individuals often assume that simply learning the basics of billing or coding on YouTube or through low-cost online platforms will be enough to land a job. But the reality is that without a formal credential, resumes get skipped, and applications hit dead ends. Even when interviews happen, candidates face skepticism about whether they can meet HIPAA-compliant documentation, payer standards, or error-free claim cycles.
On average, uncertified job seekers take 5 to 7 months longer to secure their first role, often settling for data entry or assistant-level work with limited exposure to full-cycle billing processes.
Certified candidates, especially those who have completed AAPC-approved programs, have a drastically different experience. Their resume shows proof of education in ICD-10, CPT, HCPCS, claims cycle, modifiers, and payer policy compliance. Employers see them as plug-and-play professionals, which cuts down hiring risk.
Most certified coders land jobs within 30–90 days after completing their program, especially when supported by career placement services. Employers in hospitals, urgent care chains, and third-party billing agencies often maintain direct pipelines with training institutions to recruit new talent. Certification doesn’t just open doors—it shortens the distance to employment.
Stability and long-term growth
Even if an uncertified individual manages to get into the workforce, their path forward is steep and uncertain. Without formal credentials, they’re often locked into lower-paying positions and are the first to be cut during restructuring or automation rollouts. Their roles typically cap out below $50,000/year, with limited opportunity for raises or role changes.
Certified professionals, on the other hand, aren’t just getting jobs—they’re building careers. Certification qualifies them for consistent advancement through levels such as coding specialist, auditor, revenue cycle analyst, and compliance officer. Every additional year of experience stacks on top of that foundation, opening doors to roles that cross over into insurance, consulting, and healthcare policy.
One of the key reasons for this growth is credibility. Certification—particularly the AAPC-certified billing and coding credential—signals to employers that you understand claims optimization, appeals processes, preauthorization coding, and insurance carrier expectations. These aren't skills easily taught on the job.
More importantly, certified coders are better insulated from market volatility. As healthcare shifts toward digital records and AI-assisted claims management, employers are actively retaining certified professionals who can adapt, audit, and ensure compliance—skills machines can’t replicate.
Over a 10-year span, the lifetime earning potential of a certified coder can exceed $100,000 more than an uncertified peer, purely from differences in salary progression and advancement opportunities.
Financial Investment vs Earnings
A common concern before enrolling in any healthcare program is the financial commitment: “Will I earn back what I spend—and how fast?” When it comes to medical billing and coding, this question is not only fair—it’s crucial. A certification should give you financial leverage, not just credentials. Here’s a transparent look at what the numbers say.
Program costs vs starting salaries
The cost of a reputable billing and coding program can range between $1,200 to $3,500, depending on provider, included materials, and certification prep. Some higher-end programs also include exam fees, resume prep, job coaching, and EHR platform access, which add long-term value.
But cost alone means nothing without comparison to outcome. Here’s how certification stacks up in real-world entry-level pay:
Uncertified candidates: Typically land data entry or junior admin roles with starting salaries around $28,000–$34,000. These roles often plateau within 1–2 years, with little room for upward movement.
Certified professionals: Particularly those with an AAPC-certified billing and coding credential, start closer to $42,000–$50,000—sometimes higher in urban regions or hospitals. That’s a $14,000+ salary delta right out of the gate.
If you land a mid-range certified job at $46,000/year and paid $2,000 for your certification, your entire program cost equals less than 5% of your first-year salary—a ratio very few training programs can match.
Break-even point and lifetime value
Understanding the break-even timeline helps answer the most practical question: How long until I recoup my investment? Let’s break it down.
1. Break-even timeline:
If your program cost is $2,500 and your salary boost compared to an uncertified peer is $14,000 annually, you recoup that in just over two months of work.
With part-time roles or remote billing positions, break-even may stretch to 4–6 months, still well under a year.
2. Lifetime earnings delta:
Let’s conservatively assume:
A certified coder earns $14,000 more annually than an uncertified peer
They work 10 years without changing fields
That’s a $140,000 difference over a decade—without even factoring in raises, promotions, or specialization (auditing, compliance, etc.).
3. Additional cost savings from certification:
Shorter job hunt duration (saving 3–6 months of unemployment)
Reduced need for remedial training or bootcamp refreshers
Lower application rejection rate—saving both time and money
When you zoom out, an AAPC-accredited billing and coding certification becomes one of the highest-yield education investments in the healthcare field. You're not just paying for a course—you're buying your way into a faster hiring cycle, higher salary ceiling, and resilient long-term income.
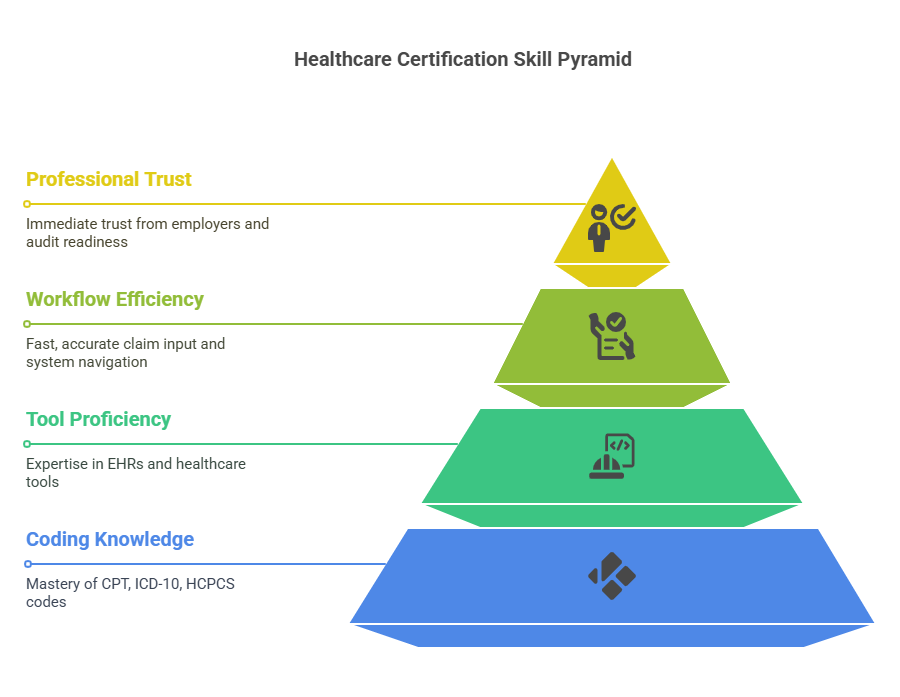
How Certification Improves Skills
Technical skill is the currency of healthcare admin—and without it, your resume holds little weight. Certification isn’t about memorizing codes; it’s about building practical fluency in healthcare reimbursement systems. From code sets to digital platforms, employers expect certified professionals to be job-ready from day one. Two skill areas matter most: medical coding mastery and tool proficiency.
Knowledge of CPT, ICD-10, HCPCS
Every diagnosis and procedure must be translated into codes. If you can’t code it, a provider doesn’t get paid. That’s why CPT, ICD-10, and HCPCS form the backbone of certification programs.
CPT tracks procedures and services like physician visits and lab tests. Accurate CPT use reduces denials and boosts reimbursements.
ICD-10 codes represent diagnoses and conditions. Errors here are a major reason for claim rejections.
HCPCS covers services not in CPT—like ambulance rides and equipment—crucial for Medicare/Medicaid compliance.
An AAPC-certified billing and coding program trains you to interpret documentation, apply modifiers, and follow payer-specific rules—not just memorize code sets. Certified coders deliver speed, accuracy, and compliance under pressure.
Confidence using EHRs and tools
EHRs like Epic, Cerner, and Kareo run the back end of modern healthcare. Certification teaches not only theory but also real-world workflows needed to code directly from patient charts.
Key advantages:
Fast, accurate claim input: Coders extract clinical data, apply correct codes, and submit clean claims—avoiding denials and delays.
System navigation: Certified coders adapt faster to multi-tab interfaces, dropdowns, and custom data fields.
Workflow automation: Tools like claim scrubbing and denial alerts become assets—not barriers—when properly used.
HIPAA-compliant logging: Certification builds secure habits for working with protected health data.
Trained coders walk into jobs speaking the language of tools, not just terminology—earning immediate trust from employers and staying audit-ready at all times.
Tie-In: AAPC-Certified Billing & Coding Program
Among dozens of online training programs, very few actually prepare students for real-world billing and coding roles. Our AAPC-certified billing and coding program is designed to eliminate the fluff, accelerate your job-readiness, and produce candidates that employers want to hire immediately.
Why our certification is worth it
Our training isn’t about just passing the exam—it’s about transforming learners into professionals that hospitals, insurers, and private practices can trust on day one. What makes our program different?
Comprehensive CPT, ICD-10, and HCPCS instruction: You’ll master the three primary code sets with examples across 200+ real case scenarios so you’re fluent in multi-specialty environments.
Built-in EHR simulator training: Unlike theory-based programs, we embed EHR functionality into your workflow. You’ll practice coding directly from patient charts, just like you'd do in a clinic or revenue cycle firm.
Live mentor feedback: Every student gets access to 1-on-1 mentorship with certified coders, giving you fast correction, confidence, and guidance every step of the way.
Exam-focused prep with unlimited practice: You’ll receive tailored drills that reflect current AAPC exam standards—no outdated PDFs or generic lessons.
More than just theory, our curriculum delivers job functionality, payer compliance understanding, and career guidance, all under the umbrella of AAPC standards.
The Fastest Path to Employer-Ready Medical Coding Skills
When you're comparing billing and coding courses online, the surface-level similarities can be misleading. Many programs advertise certification prep—but few are designed to deliver career-focused, employer-ready skills in under two months. Here’s exactly how our program stands apart:
Career-paced, not just self-paced
Our curriculum is mapped to a 7-week completion path, with every module engineered for one outcome: get hired fast. You’ll get CPC exam prep, real-world case studies, resume reviews, and soft skills that make you stand out in interviews.200+ specialty modules across real healthcare domains
Most programs stop at generalist coding. Ours prepares you for cardiology, orthopedics, pediatrics, oncology, dermatology, and beyond—because specialization opens doors and boosts income.Lifetime access and ongoing updates
Coding rules change. Insurance policy shifts. Regulations evolve. That’s why your certification includes refresher lessons, compliance updates, and policy walkthroughs for years after you graduate.Real hiring support, not just a certificate
You don’t get dumped into the job market alone. Alumni receive continued access to private job boards, hiring partner connections, and interview preparation—all designed to get you working faster.
Long-Term Career Trajectories
A medical billing and coding certification isn’t just about landing your first job—it’s about accelerating your career beyond the entry level. The reality is, employers don’t just want coders—they want coders who can grow into auditors, analysts, managers, and compliance officers. And that’s exactly where certified professionals win.
Roles you can grow into (auditor, manager, etc.)
Once you’ve gained 12–24 months of experience in a coding role, doors start opening quickly—especially if you're working with high-volume providers or multi-specialty networks. Certified professionals often step into roles like:
Coding Auditor: These professionals review the accuracy of submitted claims, conduct internal audits, and help organizations prepare for payer or government inspections. Auditors often earn $65,000–$80,000 annually.
Revenue Cycle Analyst: These roles focus on claim optimization, reimbursement strategy, and data-driven improvements across the billing lifecycle.
Compliance Officer (entry-level): Certified coders with strong documentation and HIPAA knowledge often assist legal or compliance departments to minimize audit risks.
Billing Supervisor or Coding Team Lead: These professionals manage coding teams, oversee accuracy metrics, and coach junior staff—a natural step up from senior coder roles.
Each of these roles brings a jump in pay, responsibility, and career security—and each is far more accessible when you’ve earned an AAPC-certified billing and coding credential.
How certified coders move up faster
Uncertified workers may eventually gain some hands-on knowledge, but it happens slowly—and often without a clear promotion path. Certified coders are different. They already speak the language of CPT, ICD-10, and payer policies. They already know denial management, modifier logic, and how to interact with EHRs across specialties.
Here’s why certified coders advance faster:
They get assigned to high-stakes coding tasks early, building credibility in high-billing departments like radiology or surgical units.
They’re trusted to train or review others’ work, giving them leadership visibility.
They’re more likely to be nominated for compliance and QA projects, because they already understand audit standards and claim precision.
Over time, that turns into real leverage. By year three, many certified coders move into analyst or lead roles. By year five, they’re often earning $75,000+ annually, sometimes even transitioning into remote consulting or payer-side positions.
In short, certification doesn’t just open the door—it lays down the entire blueprint for long-term, upward mobility.
What matters most to you in a billing & coding program?
In Summary
If you’re asking whether a medical billing and coding certification is worth it—the honest answer is only if you choose the right one. In 2025, employers don’t have the time or budget to train unprepared staff. They want professionals who can code accurately, use EHRs fluently, and understand payer systems inside out.The right certification doesn’t just get you hired—it raises your starting salary, accelerates your career timeline, and gives you leverage across every future promotion or job change. Programs like the AAPC-certified billing and coding credential aren’t academic exercises—they’re tools of real economic mobility.
In an industry that values precision, compliance, and speed, being uncertified means working harder for fewer results. Being certified means becoming the person hiring managers trust, rely on, and eventually promote. You’ve now seen the data, the salary deltas, the job path differences, and the real-world outcomes. If you're serious about healthcare, certification isn’t a cost—it’s the smartest move you can make.
Frequently Asked Questions
-
A medical billing and coding certification is a professional credential that proves you understand how to convert patient data, diagnoses, procedures, and treatments into standardized codes used for insurance claims and health records. Certification programs train you in CPT, ICD-10, and HCPCS code sets, as well as HIPAA compliance, claims processing, and EHR systems. The goal is to make you job-ready to handle the full billing cycle—from reviewing clinical notes to submitting clean claims. The most recognized credential in the field is the AAPC-certified billing and coding certification, which aligns closely with real-world employer needs. Certification ensures you're prepared to meet strict payer policies and audit standards, which directly impacts your hireability and salary.
-
Technically, you can apply for some entry-level jobs without certification, but your chances of getting hired—and advancing—are extremely limited. Most employers now list certification as a required or preferred qualification, especially in hospitals, large clinics, and insurance companies. Without it, you may be relegated to clerical roles that don’t involve actual billing or coding responsibilities. Certification, especially from an organization like AAPC, serves as proof that you understand medical terminology, claim cycles, code sets, and digital health systems. It also reduces the training burden on employers, making you a safer hire. In short, certification is not legally mandatory, but it is practically essential if you want access to competitive, full-scope billing roles.
-
Costs can vary widely depending on the provider, training format, and what’s included. A reputable program typically ranges from $1,200 to $3,500. Some low-cost options under $1,000 are available, but they often lack AAPC exam prep, mentorship, or employer-level depth. Comprehensive programs usually include CPT/ICD-10/HCPCS instruction, access to EHR simulators, practice exams, and certification exam fees. You’ll also want to factor in costs for study guides, resits (if needed), and any required memberships for exam eligibility. While that upfront investment might seem high, most certified coders earn back their full program cost within 6–12 months of employment. Certification is one of the most affordable healthcare career investments with fast ROI.
-
Most certification programs are designed to be completed in 4 to 7 months, depending on whether you study full-time or part-time. Some intensive bootcamp formats promise results in 6–8 weeks, while more flexible online options allow you to work at your own pace over a year. The key isn’t just speed—it’s how thoroughly the program prepares you for AAPC exams, real patient documentation, and full billing workflows. If the program includes EHR practice, exam coaching, and hands-on claim simulation, expect about 120–180 hours of training. With consistent effort, certification is one of the fastest ways to enter a high-demand, professional healthcare role.
-
Job prospects are strong—and getting stronger. The U.S. Bureau of Labor Statistics projects a 8–9% growth rate in medical records and health information jobs through 2032. Certified billing and coding professionals are especially in demand across hospitals, ambulatory centers, telehealth platforms, and third-party billing firms. Employers prefer candidates who are already fluent in coding systems, EHRs, and compliance protocols, which is exactly what certification demonstrates. Many certified coders land jobs within 30–90 days of completing their program, especially if the school offers hiring support. With the rise of remote roles, certified professionals now have nationwide job access and better negotiating power.