Guide to Transitioning from Medical Coder to Health Information Manager
You’ve mastered CPT, ICD-10-CM/PCS, and payer logic. Now it’s time to scale your impact beyond individual claims into data governance, compliance, analytics, and leadership—the core of Health Information Management (HIM). This zero-fluff roadmap shows you how to convert coder strengths into HIM wins, build a portfolio that proves executive value, and navigate certifications, technology stacks, and first-90-day deliverables. Throughout, you’ll see AMBCI internal links embedded on the most relevant phrases—so you can deepen skills in predictive analytics, automation, ethics, and salary strategy while you climb.
1) From Coder to HIM: What Changes (and What Scales)
Scope shifts from codes to systems. As a coder, you optimize at the chart level. As a Health Information Manager, you own information quality across the enterprise—documentation standards, privacy, regulatory readiness, interoperability, analytics pipelines, and cross-department education. Your language must expand from CPT/ICD details to data governance, risk, and ROI. Start by standardizing terminology with clinical documentation integrity terms and claims submission terminology, then build dashboards anchored to CARC codes so executives see denial risk in financial language.
Your new KPIs. You will report clean-claim rate, first-pass payment velocity, appeal overturn percent, audit readiness scores, and privacy incident rates. Tie each to education cadences powered by continuing education accelerators and to automation guardrails informed by AI in RCM trends. If your organization spans multiple states, bring comp and staffing realism using state-by-state salary maps plus California and Florida market intel.
Risk posture. HIM leaders prevent regulatory exposure by codifying ethical billing standards and FWA detection into policy, training, and audits. That’s how you justify budget for technology, staff, and education while staying aligned with reimbursement model shifts and upcoming regulations.
| Coder Strength | HIM Responsibility | Action You’ll Take | Proof & KPI |
|---|---|---|---|
| CPT/ICD accuracy | Data quality governance | Define coding standards + audits | ↑ Clean-claim % |
| Policy lookups | Regulatory readiness | Map payer regs to SOPs | ↓ CO-50/97 |
| Denial appeals | Enterprise CARC analytics | Top-10 CARC dashboards | ↑ Overturn % |
| Provider queries | CDI alignment | MEAT & specificity playbooks | ↑ HCC validity |
| E/M leveling | Education programs | MDM micro-lessons + audits | ↓ Recoupments |
| Chart review | Audit lifecycle | Pre-/concurrent/post-bill mix | ↓ Rework hours |
| Scrubber use | Tool stack ownership | Optimize edits + rules | ↑ First-pass pay |
| Specialty coding | Risk-based sampling | Payer/RVU triage | ↑ Audit ROI |
| Modifier logic | NCCI governance | 59/XS edit policy | ↓ Bundling denials |
| Telehealth rules | Virtual-care compliance | POS 02/10, 95/GT checks | 0% POS denials |
| Appeal packets | Evidence libraries | Template & citation index | ↑ Speed to file |
| ICD specificity | HCC/RAF integrity | Chronic sweeps & linkage | >90% valid HCCs |
| Workflow savvy | Process redesign | Swimlanes & SLAs | ↓ Cycle time |
| Doc templates | Template governance | E/M & orders controls | ↑ Doc quality |
| Query etiquette | Provider relations | Consultative coaching | ↓ Repeat errors |
| Detail orientation | Privacy & security | Access & retention rules | ↓ Incidents |
| Report reading | Exec dashboards | Denial + revenue views | ↑ CFO alignment |
| Policy updates | Reg watch | Monthly change logs | ↓ Surprise denials |
| Teamwork | Cross-functional leadership | RCM/CDI/IT cadence | ↑ Throughput |
| QA mindset | Continuous improvement | PDCA cycles + metrics | ↑ Stability |
| Tools literacy | Interoperability | Data handoffs & formats | ↓ Data loss |
| Audit notes | Defensible records | Evidence trails & sign-offs | ↑ Readiness |
| Problem solving | Incident response | Root-cause + CAPA | ↓ Recurrence |
| Numbers focus | Financial alignment | Revenue-linked KPIs | ↑ Budget wins |
| Mentoring | Talent pipeline | LMS + ladders | ↑ Retention |
| Docs & SOPs | Policy hub | Single source of truth | ↑ Compliance |
| Trend spotting | Forecasting | Seasonality & payers | ↑ Planning |
2) Skills & Certifications That Unlock HIM Roles
Leadership + data competencies. You’re moving from code assignment to system stewardship: governance charters, documentation standards, privacy enforcement, and cross-team SLAs. Anchor your language in coding software terms so clinical, IT, and finance stakeholders share definitions. Build credibility with quick wins tied to financial audit principles and ethical frameworks.
HIM-aligned study plan. Design a 12-week track that layers documentation integrity, denial analytics, and regulatory readiness. Use continuing education accelerators to structure CEUs that also serve your portfolio. Keep a running dossier of policy changes with 2025–2030 regulatory timelines and forecast operational impacts using reimbursement model shifts.
Market reality check. Base your title/compensation ask on team maturity and state demand using salary guides plus California/Florida benchmarks. This is the simplest way to negotiate budget for additional analysts, a CDI specialist, or upgraded scrubber rules.
3) 90-Day Transition Plan that Executives Respect
Days 1–30 — Assess & stabilize.
Map your ecosystem: EHR, encoder/scrubber, analytics, edit rules, CARC reporting. Normalize nomenclature with terminology guides and CDI terms.
Risk snapshot: Build a “Top 10 Denials” board grounded in CARC families and flag quick wins tied to automation.
Education cadence: Launch weekly 15-minute huddles; pick high-leverage topics (modifier 25, MDM pitfalls, POS 02/10) supported by ethical rules.
Days 31–60 — Redesign & prove ROI.
Edit governance: Convert ad-hoc scrubber tweaks into a changelog with owner, rationale, and KPI impact; tie to financial controls.
Pre-bill shift: Move a share of audits upstream; quantify lift in clean-claim % and first-pass pay using predictive analytics.
Template governance: Clamp down on documentation drift with CDI-approved note templates referencing CDI glossary.
Days 61–90 — Institutionalize & scale.
Policy hub: Publish SOPs for NCCI edits, telehealth, and appeals, referencing claims vocabulary and FWA definitions.
Reg watch: Add a monthly governance meeting that tracks upcoming regulations and payment model changes.
Hiring case: Use state salary data to justify a CDI specialist or denial analyst once your first set of KPI lifts is documented.
Quick Poll: What’s your biggest blocker moving into HIM?
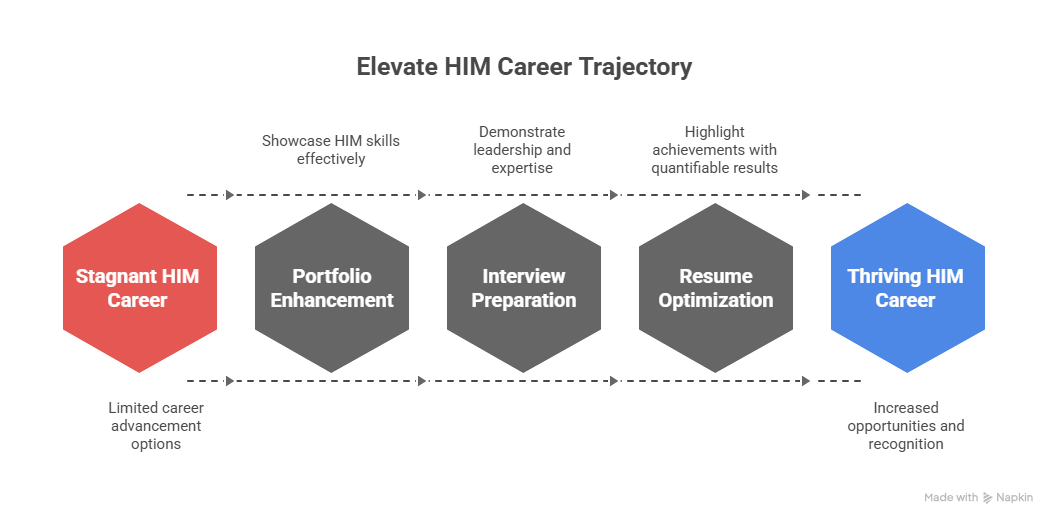
4) Portfolio, Interviews, and Executive Storytelling
Build an HIM-grade portfolio (3 briefs).
Denial governance: A before/after of Top-10 CARC playbooks, edit changes, and a 30-day first-pass pay lift.
CDI-driven HCC integrity: Template redesign tied to CDI terms and >90% valid HCC capture.
Regulatory readiness: SOP library aligned to claims terminology, FWA prevention, and upcoming changes.
Interview drills that signal leadership.
Dashboard walkthrough: Explain your metrics stack and why executives trust it, citing financial audit logic.
Template governance plan: Show how you prevent drift using CDI vocabulary and a quarterly review.
Automation rubric: Define human-in-the-loop acceptance criteria grounded in AI in RCM.
Education cadence: Map 12 micro-lessons using continuing education tactics to demonstrable KPI lifts.
Resume power lines (replace duties with deltas).
“Built CARC-based denial governance program; CO-50/97 down 28% in 90 days; clean-claim rate ↑ from 92.1% to 97.6%; launched CDI templates that pushed >90% HCC validity; instituted edit-rule changelog aligned to financial controls.”
5) Technology, Operations & Change Management Playbooks
Tool stack decisions that matter. Your first wins rarely require new software; they require governance. Start by auditing scrubber rules and encoder mappings against claims vocabulary; stabilize terminology via software terms; and formalize edit ownership on a single page. Add predictive triage fed by denial analytics before pitching any major platform changes.
Education → prevention loop. Convert common failure modes (modifier 25, POS 02/10, chemo hierarchy) into 10-minute micro-lessons and measure impact weekly. Anchor messaging to ethical principles and FWA language so compliance signs off quickly.
Regulatory radar. Publish a one-pager each month summarizing upcoming regulatory changes, plus operational adjustments and KPI impacts tied to payment model changes. This keeps IT, finance, and revenue cycle in lockstep.
6) FAQs — Transitioning from Medical Coder to Health Information Manager
-
Run a 90-day plan: (1) build a Top-10 CARC dashboard, (2) stabilize templates using CDI vocabulary, (3) move audits pre-bill via predictive analytics, and (4) publish SOPs aligned to claims terminology. Use salary maps to calibrate your title/comp ask.
-
Useful, but not always first. Many leaders prioritize governance wins and defensible metrics. Stack CEUs with continuing education strategies while proving ROI via financial audit alignment and automation fluency.
-
Translate coding risk into finance KPIs (first-pass pay, overturn %, refund exposure). Normalize language with claims vocabulary and software terms; then present one slide per KPI with red/green targets.
-
Uncontrolled template drift, edit changes without owners, and training with no metrics. Fix them with a changelog tied to financial controls, monthly regulatory watch, and micro-lessons mapped to ethical standards.
-
Present before/after deltas (CO-50/97, clean-claim %, appeal speed) and show how predictive analytics would scale the lift. Use state salary data to price the role; align controls to financial audit expectations.
-
Prove time savings and reduced rework. Roll out two-note pilots with CDI-approved phrasing from CDI glossary, measure clean-claim lift, and spotlight quick wins in a 10-minute huddle.