Medical Billing and Coding Certification in Indiana: Complete Guide for 2025-2026
Indiana's healthcare ecosystem is shifting rapidly toward value-based care, and with it comes the rising demand for CPC and CPB-certified professionals. From Indianapolis to Evansville, health systems are aggressively hiring coders and billers who can navigate payer-specific documentation, ensure audit compliance, and reduce denial rates. Whether you’re targeting hospital revenue cycle teams, outpatient specialty clinics, or remote RCM contracts, certification is now essential in Indiana’s healthcare hiring pipeline.
How to Become a Certified Medical Biller and Coder in Indiana
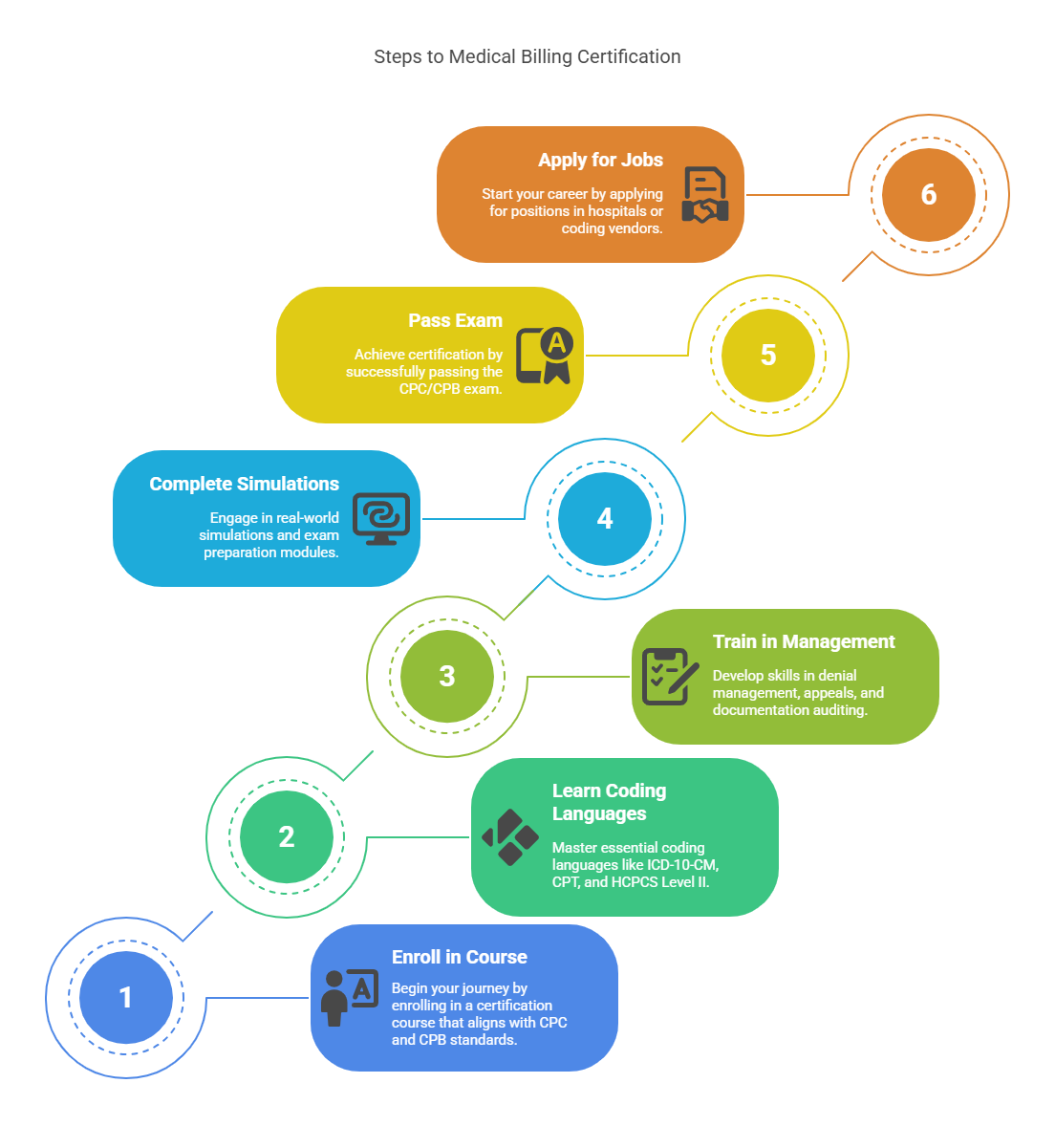
If you're starting or upskilling in Indiana, here's the direct path to getting certified:
Enroll in a CPC + CPB-aligned certification course that covers coding, billing, and audit prep
Learn ICD-10-CM, CPT, HCPCS Level II, and payer-specific modifier usage
Train on denial management, appeals, documentation auditing, and financial workflows
Complete real-world simulations and exam prep modules
Pass the CPC/CPB exam, then apply for jobs with hospitals, coding vendors, or national RCM platforms
To boost your claim approval rate and documentation accuracy, review this medical coding compliance dictionary with NCCI edit logic, bundling/unbundling rules, and OIG watchlist terms.
Which billing/coding setting are you most interested in for Indiana?
Salary Expectations and Hiring Trends in Indiana
Indiana’s salary bands reflect national averages, with significant bonuses for dual-certified candidates and those trained in specialty billing.
| City | Avg Salary (CPC+CPB) | Key Employers |
|---|---|---|
| Indianapolis | $56,000–$65,000 | IU Health, Eskenazi Health, Franciscan Alliance |
| Fort Wayne | $52,000–$60,000 | Parkview Health, Lutheran Hospital |
| Evansville | $50,000–$58,000 | Deaconess Health System, Ascension |
Coders with specialty knowledge—especially in durable medical equipment (DME) billing and chiropractic practices—are particularly sought after in Indiana’s outpatient networks.
What Indiana-Based Coders Learn in Certification Programs
Indiana’s job market rewards deep technical knowledge. Your certification training will include:
ICD-10 and ICD-11 code structure
Evaluation & Management (E/M) coding and CPT modifiers
Billing workflows and claims submission terminology
CDI (clinical documentation integrity) rules and audit vocabulary
FWA prevention protocols and fraud indicator terms
Specialized fields like chiropractic billing and behavioral health
To stay compliant with Medicare audits, especially for dual-eligible patients, it's worth mastering the financial audit terms coders use daily.
Where Certified Billers and Coders Work in Indiana
After certification, job opportunities in Indiana span both on-site and remote employers:
Hospital billing and coding departments (IU Health, Ascension, Community Health Network)
Multi-specialty physician groups and ambulatory surgical centers
Third-party billing companies with Indiana-based clients
Home health, hospice, and rehab facilities needing specialized DME coders
Fully remote CPC/CPB roles with national payers and EHR-integrated platforms
Explore other markets like Florida or Alaska to compare telehealth billing opportunities and salary trends.
Frequently Asked Questions
-
Yes. AAPC-recognized certification (CPC, CPB, or both) is a baseline requirement for most employers.
-
Yes—many Indiana-based coders now work remotely for national RCM companies and hospital systems across state lines.
-
Yes. Reputable certification programs include FWA training and compliance modules to prep you for real-world audits.
-
Most use Epic or Cerner, so familiarity with those EHRs—and CDI terms—is a major plus.
-
Absolutely. Indiana providers are transitioning toward ICD-11 documentation standards ahead of schedule due to integrated system upgrades.