Reference: Understanding Medicare Reimbursement Fully
Medicare reimbursement looks “simple” until you actually have to get a claim paid. Then you meet the real system: coverage rules that change by locality, edits that bundle work you thought was separate, and remittance codes that tell you nothing unless you know how to read them. If you are a coder or biller, your job is not just choosing the right code. Your job is proving medical necessity, matching the right payment methodology, and preventing denials before the claim even leaves your clearinghouse. This guide breaks Medicare reimbursement down end to end, so you can predict payment and fix leakage.
1) Medicare Reimbursement, Fully Explained: The Real Payment Equation
If you want to understand Medicare reimbursement “fully,” stop thinking in terms of one fee schedule. Medicare reimbursement is a chain, and payment only happens when every link holds:
Coverage (is it covered and medically necessary) + Correct coding (CPT, HCPCS, ICD 10 CM diagnosis) + Correct claim construction (modifiers, POS, NPI, taxonomy, dates) + Correct payment system (physician, outpatient, inpatient, DME) + Clean adjudication (edits, coordination, patient responsibility).
That chain is why teams that only focus on codes still bleed revenue. The fastest way to build “Medicare intuition” is to master terminology and workflow language, especially the terms used in the medical claims submission terminology guide and the operational concepts in the coding software terminology guide. Medicare reimbursement is not just a policy topic, it is an execution topic, and execution fails in predictable places.
The four Medicare reimbursement questions that determine payment
Every paid Medicare claim answers these four questions, whether you see them or not:
Is the service covered and justified for this patient on this date.
Was it documented well enough to prove why and how it was performed.
Was it coded and billed correctly based on what was actually done.
Does Medicare’s payment system allow it under that setting, provider type, and site.
If your denials feel random, they are usually one of these four questions being answered “no.” This is why reimbursement skill overlaps heavily with compliance and audit readiness, which is also the theme in coding compliance trends and why payer pressure is rising in upcoming regulatory changes affecting medical billing 2025 to 2030.
Medicare is tightening, and the edits are getting smarter
Modern Medicare reimbursement is increasingly shaped by automation. That means more claims are judged by pattern logic, not human context. If your claim “looks off,” it gets kicked even if the care was real. Understanding this trend is now part of the job, which is why AMBCI also tracks the evolution in the future of medical coding with AI and the practical skill shift in future skills medical coders need in the age of AI. Medicare reimbursement is becoming more “rules plus data,” not “rules plus narrative.”
The most important concept: payment methodology changes the rules
A physician office claim is not paid the same way a hospital outpatient claim is paid. A facility inpatient claim is not paid the same way DME is paid. If you do not identify the payment system correctly, you will misread why something denied and you will apply the wrong fix.
This is one reason why Medicare and Medicaid policy awareness matters beyond coding, and why it helps to keep a bigger picture view using future of Medicare and Medicaid billing regulations alongside operational denial data approaches like predictive analytics in medical billing.
2) Physician and Clinic Reimbursement: How Medicare Actually Prices CPT Codes
Most coders first meet Medicare reimbursement through physician claims, where payment is driven by CPT codes and the Medicare Physician Fee Schedule logic. Even if you never calculate RVUs manually, your daily results are controlled by those mechanics.
Why “correct CPT” is not enough for Medicare payment
Two claims with the same CPT can pay differently because of:
Place of service differences
Modifier context
Provider type and enrollment
Locality adjustments
Bundling and unit limits
This is why claim construction skills matter as much as coding skills, which is also why the medical claims submission terminology guide is not optional reading if you want to stop leakage. It is also why tool literacy matters, because modern edits live inside software, and teams that understand the coding software terminology guide troubleshoot faster.
Modifiers are Medicare’s language for “context”
Medicare uses modifiers to understand if a service was distinct, repeated, staged, or performed in a specific scenario that affects payment. If your modifier choice is “habit based,” Medicare will eventually punish it with bundling or denials because the documentation does not match the story your modifier tells.
This connects directly to compliance enforcement, especially the patterns highlighted in coding compliance trends and why regulation shifts are expected in upcoming regulatory changes affecting medical billing 2025 to 2030. Medicare is becoming less tolerant of sloppy context.
Bundling is not a denial, it is a reimbursement decision
A classic Medicare shock is when a secondary service is not paid, but the claim is not technically “denied.” That is bundling. The work may be considered included in the primary service. The right response is not always an appeal. The right response is verifying whether:
The service is truly separately payable
The services were actually distinct
Documentation supports distinctness
Your modifiers and diagnosis linkage tell the right story
Teams that track top bundling impacts like denial categories get ahead faster. This is where thinking like analytics pays off, especially when applying concepts from predictive analytics in medical billing. Your goal is to predict and prevent, not react and resubmit.
“Medicare allowed amount” is your real benchmark
Charge amounts do not matter to Medicare the way they matter to private payers. What matters is the allowed amount and how Medicare splits responsibility between Medicare payment and patient responsibility. If your team does not benchmark expected payments, you will miss underpayments and incorrectly blame coders for what is actually a payment logic issue.
If you want a future proof approach, learn where AI and automation are heading in AI in revenue cycle management and how that affects modern coding roles in future skills medical coders need.
3) Facility Reimbursement: Outpatient vs Inpatient and Why the Payment Rules Change
Facility reimbursement is where many teams get confused because the same clinical service can live in different payment worlds. Your first move is always identifying the setting and then applying the right reimbursement logic.
Outpatient hospital reimbursement: packaging is the hidden rule
Medicare outpatient payment often packages related items into one payment structure. That means certain “supporting services” may be bundled into a primary payment unit. If your facility expects separate payment for every supply or service, they will think they are being underpaid. Your job is to know when packaging is normal and when charge capture is failing.
This is why compliance and workflow reading matters, and why it helps to keep your operational terminology sharp using the medical claims submission terminology guide and your system literacy sharp using the coding software terminology guide.
Inpatient reimbursement: documentation integrity is reimbursement integrity
In inpatient settings, payment is heavily influenced by diagnosis selection and documentation of severity. If documentation is vague, the case groups differently, and the facility loses money even though the care was correct. That is why facility reimbursement lives and dies by documentation integrity, which is exactly the logic behind the clinical documentation integrity terms guide. This is not about gaming. It is about accurately reflecting the clinical reality in words that the payment system can read.
Specialized settings like DME are a different reimbursement universe
DME reimbursement has its own vocabulary, rules, and proof requirements. If your organization touches durable medical equipment, you need to treat it as a separate reimbursement track with its own documentation and billing discipline. Building that knowledge gets easier by pairing reimbursement concepts with niche coding education such as the DME coding guide and maintaining compliance awareness through coding compliance trends.
Medicare rules change, so teams must change processes
Medicare reimbursement is being shaped by evolving regulation, increased payer scrutiny, and automation. Teams that update policies once a year will fall behind. This is why it helps to anchor your planning to broader policy content such as future of Medicare and Medicaid billing regulations and how new healthcare regulations will impact coding careers. The workforce impact is real, especially with the trendline described in the future of medical coding with AI.
4) Coverage, Medical Necessity, and Documentation: The “Make or Break” Layer
Most Medicare reimbursement failures do not happen because the CPT code was wrong. They happen because Medicare did not accept the story your claim told.
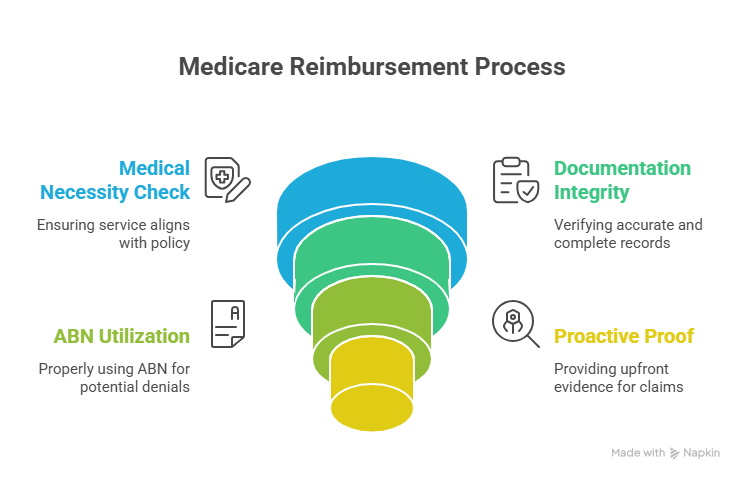
Medical necessity is the reimbursement gatekeeper
Medicare does not pay because a service exists. Medicare pays because a covered service was needed for a documented reason that matches policy rules. If your diagnosis does not support the service, the claim fails even if the work was performed perfectly.
This is where documentation integrity becomes reimbursement integrity. Use the mindset in the clinical documentation integrity terms guide and pair it with compliance awareness from coding compliance trends. The system is designed to pay the provable, not the assumed.
ABN is a reimbursement tool, not a formality
When Medicare is likely to deny, ABN protects the organization and clarifies patient responsibility. But ABNs fail when they are used too late, used too broadly, or filled out poorly. Your workflow must treat ABN as a front end reimbursement safeguard, not a back end apology.
If your team struggles with consistent front end claim behavior, strengthen your claim language discipline using the medical claims submission terminology guide and standardize tool use using the coding software terminology guide. Medicare reimbursement is operational, not theoretical.
Medicare reimbursement is shifting toward proactive proof
Automation is pushing Medicare and contractors toward “prove it up front” behaviors. That means better documentation is not just for audits. It is for faster claims and fewer pended cases. This is why it helps to understand what is coming through how automation will transform medical billing roles and where the data layer is going through AI in revenue cycle management. Even basic Medicare reimbursement is being optimized by algorithms.
5) Denials, Remittance, and Appeals: How to Turn Medicare “No” Into a Paid Claim
If Medicare reimbursement is a chain, denials management is where you learn which link broke. Your goal is not to appeal everything. Your goal is to categorize denials into fix types and eliminate the root cause.
Read the remittance like a reimbursement detective
The remittance advice does not just say “denied.” It tells you the category of failure through reason and remark codes. The fastest teams build a denial dictionary that translates common codes into:
front end fix
coding fix
documentation fix
coordination fix
appeal with evidence fix
This is denial analytics in practice, and you can apply the mindset from predictive analytics in medical billing to your Medicare work queues. When you treat denials as data, Medicare reimbursement becomes manageable.
Appeals are evidence plus policy language
Medicare appeals succeed when you use policy language and documentation proof, not emotion. A strong appeal includes:
a short issue statement
the policy logic or coverage rationale
excerpts from the medical record that prove necessity and execution
a clear request for reconsideration
If you want to appeal smarter and reduce audit stress, align your process with the audit discipline discussed in the financial audits guide and compliance risk awareness in the fraud waste and abuse terms guide. Medicare reimbursement and audits are linked by one theme: proof.
Coordination of benefits can break Medicare payment silently
Medicare reimbursement also fails when Medicare is not the correct payer order. If eligibility, accident details, or employer coverage is not captured correctly, claims can reject or pay incorrectly. Many teams treat this as “insurance verification,” but it is actually reimbursement prevention work. Tight front end processes reduce back end chaos, which is also a major theme in remote workforce management because distributed teams need standardized steps.
Build a Medicare reimbursement improvement cycle
A high performance Medicare billing team runs a monthly loop:
Identify top denial reasons by volume and dollars
Map each denial to a root cause lever
Update workflows, templates, and coding rules
Train using short examples
Monitor whether the denial category drops
This is the same “continuous improvement” logic behind future focused content like future of remote medical billing and coding jobs and the larger trend pressure in upcoming regulatory changes affecting medical billing. Medicare reimbursement will not get simpler, so your system must get sharper.
6) FAQs: Understanding Medicare Reimbursement Fully
-
Medicare reimbursement is a chain, not a price list. Payment happens when coverage rules accept the service, documentation proves medical necessity, coding matches what was actually done, and the claim is constructed correctly for the right payment methodology. If one link fails, the claim denies, reduces, or bundles. This is why mastering language and workflow matters as much as code selection. Build your foundation using the medical claims submission terminology guide and your systems understanding using the coding software terminology guide.
-
Bundling is a reimbursement rule, not necessarily a denial. Medicare often considers certain services included in a primary service payment, especially when they are integral to performing the main procedure or expected during the encounter. The fix is not always an appeal. The fix is verifying whether services were truly distinct and whether documentation and modifiers prove distinctness. This is also why compliance discipline matters, especially the guardrails described in coding compliance trends.
-
Most medical necessity denials occur when the diagnosis does not support the service under coverage rules, or when the documentation does not prove severity, symptoms, failed treatments, or risk factors. Medicare pays for justified care, not assumed care. Strengthen your documentation expectations using the framework in the clinical documentation integrity terms guide and stay aligned with the regulatory direction in future of Medicare and Medicaid billing regulations.
-
Start by confirming the payment methodology and the claim context. Validate POS, modifiers, units, and whether bundling or adjustments apply. Then compare the remittance codes to your expected payment logic. Underpayments are often explained by a modifier reduction, packaging rules, or patient responsibility allocation, not a coding error. Teams that benchmark expected payments and classify variances outperform teams that only react. This data driven approach aligns well with predictive analytics in medical billing.
-
Stop repeating the same denial categories. Identify the top five denial reasons by dollars, map each to a root cause lever, and fix the upstream workflow with templates, checklists, and short training. Automate work queues so only true exceptions get human time. This is the operational edge described in how automation will transform medical billing roles and the trend view in AI in revenue cycle management.
-
Write appeals like a policy and evidence brief. State the issue, cite the coverage logic, then quote the exact documentation lines that prove medical necessity and correct performance. Avoid generic templates. Medicare appeals succeed when you connect the medical record to the reimbursement rule in a clear, structured way. If you want audit safe appeal habits, align your approach with the financial audits guide and compliance risk awareness in the fraud waste and abuse terms guide.
-
AI is increasing the speed and strictness of claims scrutiny by using pattern detection and rule automation. That means inconsistencies, vague documentation, and unstable coding decisions are flagged faster, even when a human reviewer might have let them pass. Coders and billers who standardize documentation proof, understand edits, and can categorize denials quickly will become more valuable, not less. Track the shift through the future of medical coding with AI and build practical capability using future skills medical coders need.