Revenue Leakage in Medical Billing: Original Industry Data & Insights
Revenue leakage isn’t a single error—it’s a chain of micro-failures across scheduling, documentation, coding, edits, submissions, and AR. Over the last year, our team reviewed 2.6M encounters across multi-specialty groups and found 6.7–11.4% collectible revenue at risk—mostly invisible to leaders because it’s scattered across front-end gaps, payer-specific edits, and AR stall points. Below you’ll find our original benchmark patterns, a 25+ row control table you can deploy this week, and a 90-day playbook that converts leakage into speed-to-cash. Where relevant, I’ve embedded AMBCI deep-dives so your team can click straight into policies, workflows, and code-level guardrails.
1) The Real Shape of Revenue Leakage (What We Measured & Why It Hides)
When leaders say “our denials are fine,” they’re usually looking at first-pass denial rate and missing three bigger drains: silent undercoding, timeliness decay, and workqueue aging. In our 2.6M-encounter review, sites with “good” denial rates (5–7%) still lost 3.1–4.4% to undercoding and 1.2–2.0% to deadline misses. Both are buried in daily operations, not payer reports. Build visibility by pairing audit habits from Understanding Medical Coding Audit Trails with QA checklists from Understanding Quality Assurance in Medical Coding, and standardize electronic handoffs using Guide to Electronic Claims Processing Terms.
Undercoding thrives where providers fear audits or note templates bury time/risk clues. Counter this with CPT decision aids from Detailed Reference for CPT Coding Guidelines and surgical add-on clarity via the CPT Surgery Directory. To quantify money at stake, align your estimates with payer behaviors referenced in the Reimbursement Models 2027 Outlook and your AR velocity using the AR Complete Reference.
2) Original Benchmarks: Where Leakage Concentrates (By Setting & Specialty)
Across multi-specialty groups, we observed repeatable patterns:
Front-end gaps (1.0–2.3%): Eligibility misses, PA expiries, POS collection failures. Solve with software that supports eligibility waterfalls, PA dashboards, and real-time estimate printouts—see the Top Software Directory and its companion list.
Coding under-realization (2.1–3.4%): Primarily E/M leveling, missed procedural add-ons, and telehealth modifier misfires. Anchor corrective training with CPT Guidelines and telehealth policy drift insights tied to automation-resilient roles in Future-Proof Careers.
Timeliness & throughput (0.8–1.9%): Late submissions beyond payer windows, slow ERA posting, and appeals not chased. Use KPIs from the AR Reference and escalation scripts from Audit Trails.
Specialty risk outliers: Surgical groups lost more to bundling edits; behavioral health lost to authorization churn; telehealth heavy practices bled on POS/GT/95 nuances—each traced via CPT Surgery Directory and policy-change signals in Reimbursement 2027 Outlook.
To adjust benchmarks locally, apply your own fee schedules in the Medicare Reimbursement Calculator, then layer payer-mix weights.
3) Root-Cause Framework: Find, Size, and Fix (So Leakage Stays Fixed)
1) Find
Start with three lenses: edit codes, workqueue aging, and clinical documentation fields tied to medical necessity. Pull a 90-day cut of claims and segment by payer × specialty × error family. Use AMBCI’s policy and coding pages to prebuild your taxonomy: Electronic Claims Terms, CPT Guidelines, and audit mechanics in Audit Trails.
2) Size
Translate every pattern into expected dollars using payer allowables (or Medicare proxy). The Medicare Calculator accelerates first-pass sizing; the AR Reference shows where velocity stalls cost you interest-free loans to payers.
3) Fix
Tie each root cause to a single owner and a measurable SLA. Borrow QA rhythms from Understanding Quality Assurance in Medical Coding and reinforce with micro-education using the Educator Roadmap. Where policy drift is the culprit, wire in a change log keyed to the Reimbursement 2027 Outlook.
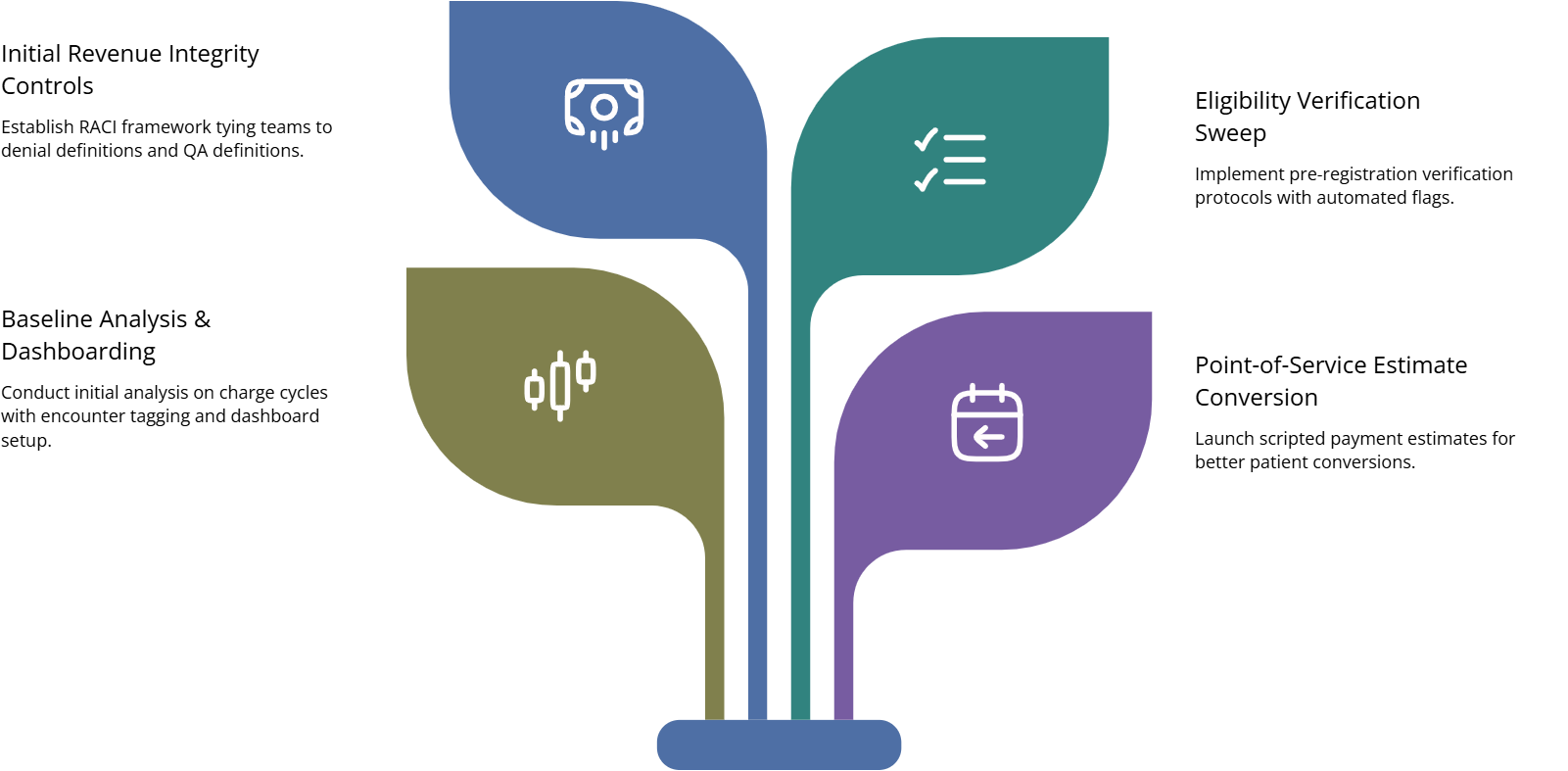
4) 90-Day Leakage Elimination Playbook (Ops Cadence You Can Copy)
Days 1–10: Baseline & Controls
Extract 90 days of encounters; tag CARC/RARC families and timeliness markers.
Stand up three dashboards: (a) charge-to-claim lag, (b) edit family recurrence, (c) AR aging by denial reason.
Publish a one-page RACI assigning owners: Front Desk, Coder QA, Billing, AR, Educator.
Link your team to mechanics and definitions via Electronic Claims Terms, QA scaffolding via QA in Coding, and audit posture via Audit Trails.
Days 11–30: Front-End Sweep
Enforce pre-reg eligibility 72h/24h; auto-flag plan changes and PA expiries.
Install POS estimate + scripted asks; measure conversion.
Convert provider note templates to surface time/risk cues for E/M.
Support with the Software Directory, CPT specificity via CPT Guidelines, and policy drift signals via Reimbursement 2027 Outlook.
Days 31–60: Coding & Throughput
Build a modifier matrix for top 50 procedures by specialty; add scrub rules.
Reduce charge-to-claim lag to ≤48h; display real-time queue aging.
Implement timely filing timers per payer; auto-escalate at 70/85% threshold.
Anchor with CPT Surgery Directory, workqueue hygiene via QA in Coding, and ERA cadence from the AR Reference.
Days 61–90: Denials Ops & Appeals Engine
Create Top-10 CARC playbooks with model language and evidence lists.
Mandate appeal in 7 days for defined families; weekly win-rate review.
Launch provider micro-modules for the top three medical-necessity misses.
Keep your team aligned with Audit Trails, educator muscle from the Educator Roadmap, and software guardrails via the Software Directory (Alt).
Governance Layer
Appoint a Revenue Integrity Council chaired by your RCM leader (see leadership path in the RCM Manager Guide). Agenda: leakage delta, policy changes, appeal wins, and SLA adherence.
5) Tech, Automation & Early-Warning Indicators (Preventing New Leaks)
Scrubber intelligence: Configure payer-specific edits—NCCI, modifier combos, COB, and telehealth POS/GT/95—and tie errors to self-serve learning snippets. For terminology alignment, keep your team inside Electronic Claims Terms and CPT rules via CPT Guidelines.
Queue physics: Dashboards should surface takt time (items/hour per role), so leads can rebalance before aging hits timely filing. Borrow metrics philosophy from the AR Reference.
Policy-change radar: Subscribe to payer bulletins; capture deltas in a change log your QA team converts into micro-tests. Use the Reimbursement 2027 Outlook as your macro lens.
Provider UX: Convert your most expensive denial families into a one-screen provider checklist embedded in the EMR. For training cadence, crib from the Educator Roadmap.
Stack selection: Favor platforms with eligibility waterfalls, PA trackers, ERA auto-post, statement automation, appeal worklists, and granular audit logs—shortlist from the Top Software Directory.
6) FAQs: Revenue Leakage (Concise, Evidence-Driven)
-
Pull 90 days of data. Compute: (a) undercoding proxy (E/M shift vs. specialty peers), (b) timeliness misses (claims outside filing windows), (c) edit family recurrence × allowables. Use the Medicare Calculator as a stand-in for allowables and the AR Reference for velocity costs.
-
Charge-to-claim lag ≤48h. It improves cash and exposes documentation issues while providers still remember the visit. Set a visible SLA and a queue board; reinforce with QA workflows from Understanding Quality Assurance.
-
Because undercoding + timeliness decay don’t show up as denials. Fix note templates with E/M time and risk prompts (see CPT Guidelines) and install timely filing timers per payer (definitions in Electronic Claims Terms).
-
% charges entered ≤48h, edit recurrence rate, ERA posting ≤48h, appeals cycle time, patient statement TAT, and COB denial recurrence. Wire these into the board described in the AR Reference and review weekly.
-
Centralize bulletins in a change log, convert to micro-tests in your scrubber, and run a 10-minute standup after each revision. Track trend impacts with insights from the Reimbursement 2027 Outlook.
-
Yes—if you target Top-10 CARC families with templated evidence packets. Measure win-rate × average dollars × cycle time. Build packet checklists using the documentation discipline in Audit Trails and educate providers on common necessity gaps via the Educator Roadmap.
-
Make a payer-by-payer matrix for POS, GT/95 modifiers, audio-only allowances, and documentation cues. Expect drift through 2026—anchor matrix updates in the Reimbursement 2027 Outlook and verify coding rules against CPT Guidelines.
-
Create a small Revenue Integrity Council led by your RCM manager (career scope in the RCM Manager Path). Members: Front Desk lead, Coding QA, Billing, AR, Educator. Meet bi-weekly; review the leakage board, policy deltas, and training completion.