Workforce Demographics Report: Medical Coders & Billers in 2025
The medical billing and coding workforce in 2025 looks nothing like it did even five years ago. Remote work, automation, ICD-11 adoption, and payer pressure have reshaped who enters the field, who stays, and who advances. Age, geography, education, certification paths, and specialization now directly influence income stability and job security. This report breaks down the real workforce demographics behind medical coders and billers in 2025, translating raw trends into career intelligence you can actually use to future-proof your role and earning potential.
1. Age, Experience, and Career Stage Breakdown in 2025
Medical billing and coding is no longer dominated by a single age cohort. In 2025, the workforce is split across early-career entrants, mid-career specialists, and late-career compliance anchors, each playing a different economic role inside the revenue cycle. Entry-level professionals aged 22–30 often enter through structured pathways like the step-by-step guide to starting a medical billing and coding career, drawn by remote flexibility and lower barriers to entry compared to clinical roles.
The fastest-growing cohort sits between ages 31–45. These professionals usually transition from administrative healthcare roles or upskill mid-career, leveraging certifications to access higher-paying opportunities described in the ultimate salary guide for certified medical billing specialists. They dominate denial management, audit preparation, and payer-facing roles because they combine operational speed with policy literacy.
Professionals aged 46 and above increasingly anchor compliance, education, and leadership functions. Many follow trajectories outlined in the career roadmap for medical coding educators, or shift into revenue integrity roles where experience matters more than throughput. This demographic trend explains why organizations struggling with audits often lack senior coders who understand historical payer behavior, a gap highlighted in coding accuracy impact reports.
2. Gender, Geography, and the Remote Work Shift
Medical billing and coding remains a female-dominant profession, but 2025 data shows a gradual increase in male participation, especially in analytics, compliance, and revenue integrity roles. Remote work has fundamentally reshaped geographic demographics. Coders in historically lower-paying regions now compete directly with metropolitan peers, a shift reflected in the state-by-state medical coding salary guide.
This geographic leveling increases opportunity but also competition. Employers now prioritize output quality, denial avoidance, and audit readiness over physical location. Teams that once relied on local labor pools now recruit nationally, sometimes globally, while still maintaining compliance with rules discussed in medical coding compliance dictionaries. For individuals, this means resumes must clearly signal value through certifications, specialties, and documented performance metrics rather than tenure alone.
3. Education, Certification, and Skill Stratification
The biggest demographic divider in 2025 is certification status, not education level alone. Professionals with structured credentials consistently outperform non-certified peers in salary, retention, and promotion speed, as documented in expert strategies to maximize your medical billing certification. Employers increasingly treat certification as proof of ethical billing, documentation discipline, and audit readiness.
Skill stratification has intensified. Generalists handle volume, while specialists command premium compensation. Coders trained in ICD-11 specificity, DME, or complex specialties such as those outlined in the DME coding guide or chiropractic coding terms guide face lower automation risk. Education is no longer static. Ongoing learning through continuing education acceleration paths has become a demographic differentiator separating stable earners from those experiencing wage stagnation.
Quick Poll: What Defines Your Role in 2025?
4. Workforce Pressure Points: Burnout, Turnover, and Automation
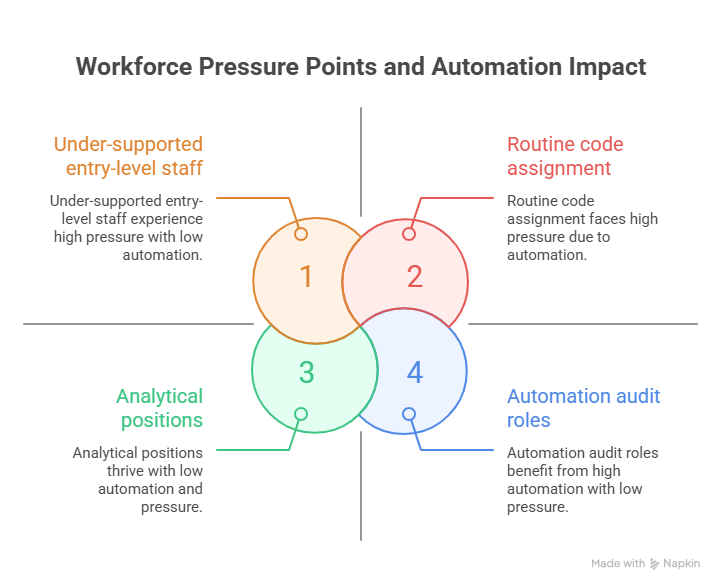
Burnout remains a defining demographic force. High denial volumes, constant payer policy changes, and aggressive productivity quotas accelerate turnover, especially among under-supported entry-level staff. Studies referenced in coding denials management analysis consistently show that teams without senior mentorship not only experience higher error rates but also lose talent faster due to stress, rework, and lack of career clarity. Over time, this creates a costly cycle where inexperienced replacements amplify denials instead of reducing them, which is exactly how organizations end up bleeding money through hidden revenue leakage and repeatable common medical coding errors.
Automation reshapes but does not eliminate roles. Routine code assignment and charge entry face pressure, yet analytical, compliance-driven, audit, and documentation-integrity positions continue to expand, aligning with forecasts in future innovations in medical billing software. Workforce demographics increasingly favor professionals who can validate automation outputs, interpret payer logic, and correct upstream documentation issues, rather than competing directly with automated tools on speed alone. That advantage compounds when coders keep up with training through continuing education and position themselves for higher-stability roles highlighted in emerging job roles for certified medical coders.
5. Career Outlook and Demographic-Driven Opportunities
Demographic shifts reveal opportunity clusters. Regions with aging populations demand more experienced coders capable of managing complex comorbidities, reinforcing the value of ICD-11 mastery shown in reimbursement impact studies. Meanwhile, younger professionals entering the field benefit most by targeting specialties, certifications, and roles mapped in top emerging job roles for certified medical coders.
Those who align career moves with demographic demand curves enjoy greater income stability and advancement, especially when supported by insights from future-proof coding career guides.
6. FAQs: Workforce Demographics of Medical Coders & Billers in 2025
-
Yes, but viability depends on specialization, certification, and adaptability. Generalist roles face wage pressure, while certified specialists in ICD-11, audits, and compliance remain in strong demand.
-
Mid-career professionals who upskill through certifications and continuing education tend to advance fastest, as shown in career acceleration guides.
-
Remote work increases competition but also expands opportunity. Job security now depends more on measurable performance and audit outcomes than location.
-
Yes, especially without mentorship. Organizations lacking senior coders experience higher turnover among entry-level staff, according to hospital revenue impact research.
-
Certification is the single strongest predictor of salary, stability, and leadership access in 2025, as reinforced across multiple AMBCI workforce studies.